
Lecture 7: Alteration of the Reproductive System
alteration of the reproductive system
can range from structural abnormalities to functional abnormalities
ex. delayed puberty, precocious puberty, hormonal and menstrual alterations, infection, and inflammation
many rs disorders such as impotence and infertility can have serious physiological and psychological consequences
alterations of sexual maturation
variety of congenital and endocrine disorders can disrupt timing of puberty
delayed or precocious (early) puberty
both types of disorder involves inappropriate onset of sex hormone production by gonads
delayed puberty
secondary sex characteristics have not appeared in girls by age 13
first sign of puberty is breast development
secondary sex characteristics have not appeared in boys by age 14
95% of cases are simply a constitutional delay
hormonal levels are normal but maturation is happening slowly
5% are caused by some type of disruption of the hypothalamic-pituitary-gonadal axis
precocious puberty
sexual maturation before age 6 in black girls and age 7 in white (and other) girls
sexual maturation before age 9 in boys
precocious puberty occurs in many forms such as
isosexual precocious puberty- premature development of secondary sexual characteristics most commonly due to premature onset of hormones
heterosexual precocious puberty- child develops some secondary sexual characteristics of opposite sex (still before typical onset)
incomplete precocious puberty- partial development of secondary sexual characteristics (some develop early, some develop at normal time)
disorders of the female reproductive system
hormonal and menstrual alterations
primary dysmenorrhea
painful menstruation associated with prostaglandin release in the ovulatory cycles
related to the duration and amount of menstrual flow
secondary dysmenorrhea
painful menstruation related to pelvic pathology
can occur any time in the menstrual cycle
dysmenorrhea is the result of excessive endometrial prostaglandin production
manifestations: pelvic pain with onset of menses
diagnosis: pelvic examination
hormonal and menstrual alterations
primary amenorrhea
failure of menarche (first period) and absence of menstruation of age 14 without the development of secondary sex characteristics and by age 16 with secondary sex characteristics
diagnosis is based on history, physical examination, and clinical symptoms
treatment involves hormone therapy and correction of underlying disorders (hypothalamus, pituitary, ovarian)
secondary amenorrhea
absence of menstruation for three or more cycles or 6 months in women who have previously menstruated
could be caused by structural abnormalities or abnormal ovarian steroid hormones
causes: pregnancy (itself but thats a normal cause, also postpartum but then its not normal), dramatic weight loss due to malnutrition or excessive exercise
normal time to resume menstruation postpartum
if breastfeeding: its common to not have a period while breastfeeding
if not breastfeeding: typically returns 6-8 weeks postpartum, if hasnt returned 3-6 months (or more), might be secondary amenorrhea
symptoms: anovulation, hyperprolactinemia, hirsutism (abnormal hairiness)
hormonal and menstrual alterations
polycystic ovarian syndrome
oligoovaluation (infrequent or irregular ovulation) or anovulation (complete lack of ovulation)
elevated levels of androgens or clinical signs of hyperandrogenism and polycystic ovaries
leading cause of infertility in the us
multifactorial
hyperinsulinism (insulin stimulates androgen secretion and reduces serum sex hormone binding globulin- excessive androgen affect follicular growth)
dysfunction of follicle development
diagnosis: excess androgen level, clinical symptoms
treatment: reversing signs of excess androgen
premenstrual syndrome (pms)
cyclic physical, psychological, or behavioral changes that impair interpersonal relationships or interfere with usual activities
symptoms can be inconsistent from month to month
occurs in the luteal (postovulatory) phase
abnormal nervous, immunologic, vascular, emotional, and gi tissue response to the normal menstrual cycle (>200 symptoms)
common and normal
infection and inflammation
infections of the genital tract can be caused by exogenous (often sexually transmitted) or endogenous (floral bacteria or vagina, or bowel) microorganisms
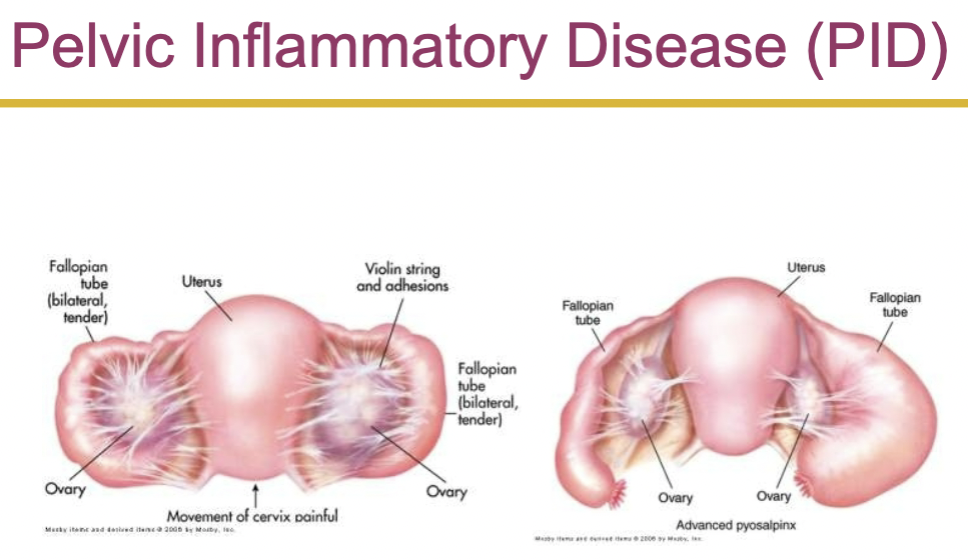
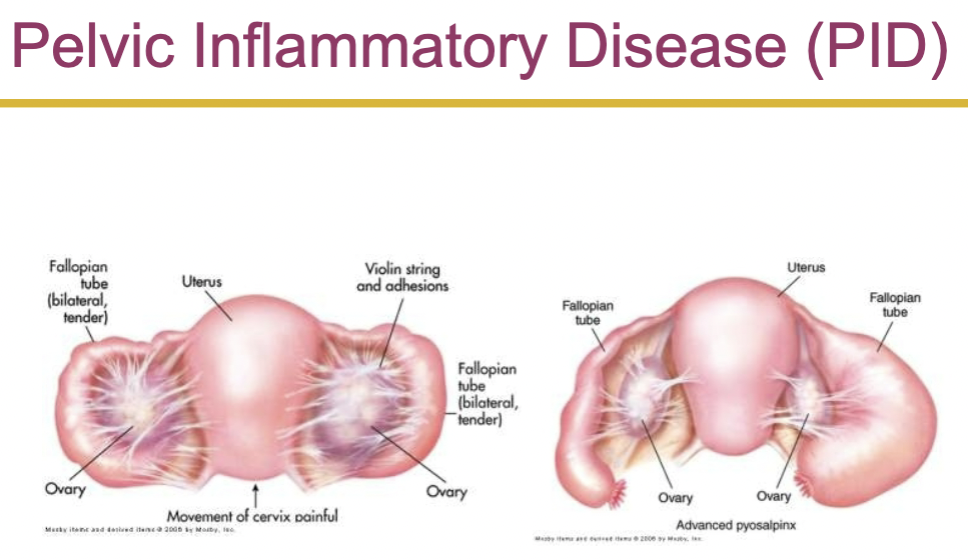
pelvic inflammatory disease (pid)
acute inflammatory disease caused by infection
may involve any organ or combination of organs of the reproductive tract
caused when sexually transmitted bacteria migrate from the vagina to the upper genital tract
vaginitis
infection of the vagina
major cause is sexually transmitted pathogens
develops due to loss of local defense mechanism ex. change of vaginal ph due to disruption of normal flora
alkaline ph occurs before puberty, after menopause, and during pregnancy
cervicitis
inflammation or infection of the cervix
vulvitis
inflammation of the female external genitalia
causes
contact with soaps, detergents, lotions, hygienic sprays, shaving, menstrual pads, perfumed toilet paper, or nonabsorbing or tight fitting clothing
vulvitis may increase susceptibility to vaginal infections that spread to the labia
pelvic relaxation disorders
the bladder, urethra, and rectum are supported by the endopelvic fascia and perineal muscles
the muscular and fascial tissue loses tone and strength with aging
cannot maintain the pelvic organs in proper position
can lead to displacement of uterine, bladder, urethra, or rectum
uterine prolapse- decent of the cervix or entire uterus into vaginal canal
vaginal prolapse
benign growths and proliferative conditions
benign ovarian cysts
may occur at anytime of life but most common during reproductive years
occurs when hormonal imbalance is common (puberty)
functional cysts such as follicular cysts and corpus luteum cysts are caused by variation of normal physiologic events
benign cysts are produced when a follicle or number of follicles are stimulated but no dominant follicle develops and reaches maturity
corpus luteum cyst may develop due to hormonal imbalances
female reproductive cancer
malignant tumors of rs are common
cervical cancer
most common cancer in women
it is a progressive disease (pre malignant lesion usually occur 10-12 years before the development of invasive carcinoma
caused by human papilomavirus (hpv)
diagnosis: since asymptomatic- regular cytological screening is necessary. clinical symptoms in late stages include, vaginal bleeding, abnormal discharge
vaginal cancer- the rarest
vulvar cancer
endometrial cancer- cancer of glandular epithelium of uterine lining
uterine sarcoma
ovarian cancer
sexual dysfunction
organic (ex. chronic illness) and psychological disorders can be implicated in sexual dysfunction
disorders of desire (inhibited sexual desire, decreased libido)can be a biological sign of depression or substance abuse
vaginismus- involuntary muscle spasm in response to penetration due to prior sexual trauma or fear of sex
anorgasmia (orgasmic dysfunction)- inability to achieve orgasm due to chronic illness (ex. diabetes, alcoholism, hormonal deficiencies)
rapid orgasm- after orgasm- little interest in sex (chain of events that could occur)
dyspareunia (painful intercourse)- women may have pain during arousal, orgasm, or initiation of intercourse due to ex. lack of lubrication
impaired fertility
infertility
inability to conceive after 1 year of unprotected sex with the same partner
fertility can be impaired by factors in the man, woman, or both
fertility tests
structural
hormonal
disorders of the male reproductive system
disorders of the urethra
urethritis
inflammation of the urethra usually, but not always, caused by a sexually transmitted disease
nonsexual origins can be due to urologic procedures, insertion of foreign objects, anatomical abnormalities, or trauma
urethral strictures
fibrotic narrowing of the urethra caused by scarring
commonly due to trauma or untreated or severe urethral infections
disorders of the penis
phimosis and paraphimosis in which penile prepuce (foreskin) is ‘too tight’
phimosis
the foreskin has a narrow opening
the inability to retract foreskin from the glans of the penis (distal to proximal)
paraphimosis
inability to replace or cover the glans with the foreskin (proximal to distal) leads to formation of constricting band around penis
frequently caused by poor hygiene or chronic infections
penile cancer
carcinoma of the penis is rare
mostly squamous cell carcinomas
disorders of the scrotum, testis, and epididymis
disorders of the scrotum
varicocele, hydrocele, and spermatocele are common disorders
varicocele
inflammation/dilation of veins in the spermatic cord
caused by inadequate or absent valves in the spermatic cord
varicocele reduces blood flow to the testicles and interferes with spermatogenesis
the blood flow/blood drainage is inefficient (it pools) which can interfere with temperature and the microenvironment
hydrocele
scrotal swelling due to collection of fluid within the tunica vaginalis
imbalance between fluid secretion and reabsorption
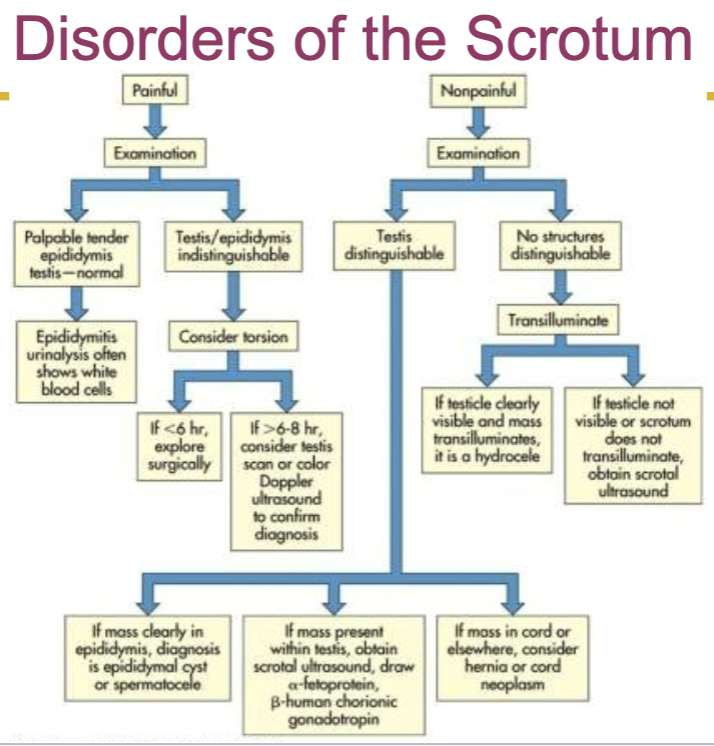
disorders of the testis
cryptorchidism
failure of one or more of the testes to descend from the abdominal cavity into the scrotum
ectopic testis
testis that has strayed from the normal pathway of descent
diagnosis in both cases is based on physical examination
treatment: hormone (gnrh, hcg) may initiate descent, if not, surgery
torsion of the testis
rotation of the testis
the rotation causes the twisting of the blood vessels in the spermatic cord
painful and swollen testis
condition may be spontaneous or follow physical exertion or trauma
if cannot be corrected manually, surgery must be performed
disorders of the epididymis
epididymitis
inflammation of the epididymis
common in sexually active young men
the pathogenic microorganism reaches the epididymis by ascending the vas deferens from an already infected bladder or urethra
pain is the main symptom
treatment include
antibiotics
symptom relief medication
disorders of the prostate gland
benign prostatic hyperplasia
enlargement of the prostate gland
symptoms associated with urethral compression
relationship to aging (80% of men before ag 80 will experience it)
evaluation
digital rectal exams
prostate specific antigen (psa) monitoring
prostitis
inflammation of the prostate
normal protective barriers
similar symptoms to bph
prostitis can be
acute bacterial
chronic bacterial
nonbacterial
cancer of the prostate
95% of prostate neoplasms are adenocarcinomas and demonstrate peripheral zone growth
prostatic cancer is asymptomatic until its advanced stages
symptoms are similar to bph
causes: dietary factors, hormones (ex. androgen), vasectomy, familial factors
male sexual dysfunction
in males, normal sexual response includes: erection, emission, and ejaculation
the causes of sexual dysfunction due to organic factors are
vascular
vascular disorders can prevent erection
endocrine
can reduce testosterone production
neurologic disorders
can interfere with sympathetic and parasympathetic innervations needed for erection
chronic diseases
renal failure and diabetes mellitus
penile diseases and penile trauma
iatrogenic factors
surgery and pharmaceuticals
impairment of sperm production and quality
spermatogenesis require hormone and growth factors
fsh, lh, and testosterone
androgen binding protein, inhibin b, and other peptides
adequate spermatogonia
sperm count >= million/mL
spem motility
antisperm antibodies
drugs and toxins in the semen
disorders of the breast
galactorrhea
persistent and sometimes excessive secretion of milky fluid from the breasts of a woman who is not pregnant or nursing
galactorrhea can also occur in men
women with galactorrhea also experience menstrual abnormalities
breast cancer
most common cancer in american women
leading cause of death from ages 40-44
second most common killer after lung cancer
reproductive factors
hormonal factors
environmental factors and lifestyle
radiation
diet
chemicals
physical activity
familial factors and tumor related genes
Lecture 7: Alteration of the Reproductive System
alteration of the reproductive system
can range from structural abnormalities to functional abnormalities
ex. delayed puberty, precocious puberty, hormonal and menstrual alterations, infection, and inflammation
many rs disorders such as impotence and infertility can have serious physiological and psychological consequences
alterations of sexual maturation
variety of congenital and endocrine disorders can disrupt timing of puberty
delayed or precocious (early) puberty
both types of disorder involves inappropriate onset of sex hormone production by gonads
delayed puberty
secondary sex characteristics have not appeared in girls by age 13
first sign of puberty is breast development
secondary sex characteristics have not appeared in boys by age 14
95% of cases are simply a constitutional delay
hormonal levels are normal but maturation is happening slowly
5% are caused by some type of disruption of the hypothalamic-pituitary-gonadal axis
precocious puberty
sexual maturation before age 6 in black girls and age 7 in white (and other) girls
sexual maturation before age 9 in boys
precocious puberty occurs in many forms such as
isosexual precocious puberty- premature development of secondary sexual characteristics most commonly due to premature onset of hormones
heterosexual precocious puberty- child develops some secondary sexual characteristics of opposite sex (still before typical onset)
incomplete precocious puberty- partial development of secondary sexual characteristics (some develop early, some develop at normal time)
disorders of the female reproductive system
hormonal and menstrual alterations
primary dysmenorrhea
painful menstruation associated with prostaglandin release in the ovulatory cycles
related to the duration and amount of menstrual flow
secondary dysmenorrhea
painful menstruation related to pelvic pathology
can occur any time in the menstrual cycle
dysmenorrhea is the result of excessive endometrial prostaglandin production
manifestations: pelvic pain with onset of menses
diagnosis: pelvic examination
hormonal and menstrual alterations
primary amenorrhea
failure of menarche (first period) and absence of menstruation of age 14 without the development of secondary sex characteristics and by age 16 with secondary sex characteristics
diagnosis is based on history, physical examination, and clinical symptoms
treatment involves hormone therapy and correction of underlying disorders (hypothalamus, pituitary, ovarian)
secondary amenorrhea
absence of menstruation for three or more cycles or 6 months in women who have previously menstruated
could be caused by structural abnormalities or abnormal ovarian steroid hormones
causes: pregnancy (itself but thats a normal cause, also postpartum but then its not normal), dramatic weight loss due to malnutrition or excessive exercise
normal time to resume menstruation postpartum
if breastfeeding: its common to not have a period while breastfeeding
if not breastfeeding: typically returns 6-8 weeks postpartum, if hasnt returned 3-6 months (or more), might be secondary amenorrhea
symptoms: anovulation, hyperprolactinemia, hirsutism (abnormal hairiness)
hormonal and menstrual alterations
polycystic ovarian syndrome
oligoovaluation (infrequent or irregular ovulation) or anovulation (complete lack of ovulation)
elevated levels of androgens or clinical signs of hyperandrogenism and polycystic ovaries
leading cause of infertility in the us
multifactorial
hyperinsulinism (insulin stimulates androgen secretion and reduces serum sex hormone binding globulin- excessive androgen affect follicular growth)
dysfunction of follicle development
diagnosis: excess androgen level, clinical symptoms
treatment: reversing signs of excess androgen
premenstrual syndrome (pms)
cyclic physical, psychological, or behavioral changes that impair interpersonal relationships or interfere with usual activities
symptoms can be inconsistent from month to month
occurs in the luteal (postovulatory) phase
abnormal nervous, immunologic, vascular, emotional, and gi tissue response to the normal menstrual cycle (>200 symptoms)
common and normal
infection and inflammation
infections of the genital tract can be caused by exogenous (often sexually transmitted) or endogenous (floral bacteria or vagina, or bowel) microorganisms
pelvic inflammatory disease (pid)
acute inflammatory disease caused by infection
may involve any organ or combination of organs of the reproductive tract
caused when sexually transmitted bacteria migrate from the vagina to the upper genital tract
vaginitis
infection of the vagina
major cause is sexually transmitted pathogens
develops due to loss of local defense mechanism ex. change of vaginal ph due to disruption of normal flora
alkaline ph occurs before puberty, after menopause, and during pregnancy
cervicitis
inflammation or infection of the cervix
vulvitis
inflammation of the female external genitalia
causes
contact with soaps, detergents, lotions, hygienic sprays, shaving, menstrual pads, perfumed toilet paper, or nonabsorbing or tight fitting clothing
vulvitis may increase susceptibility to vaginal infections that spread to the labia
pelvic relaxation disorders
the bladder, urethra, and rectum are supported by the endopelvic fascia and perineal muscles
the muscular and fascial tissue loses tone and strength with aging
cannot maintain the pelvic organs in proper position
can lead to displacement of uterine, bladder, urethra, or rectum
uterine prolapse- decent of the cervix or entire uterus into vaginal canal
vaginal prolapse
benign growths and proliferative conditions
benign ovarian cysts
may occur at anytime of life but most common during reproductive years
occurs when hormonal imbalance is common (puberty)
functional cysts such as follicular cysts and corpus luteum cysts are caused by variation of normal physiologic events
benign cysts are produced when a follicle or number of follicles are stimulated but no dominant follicle develops and reaches maturity
corpus luteum cyst may develop due to hormonal imbalances
female reproductive cancer
malignant tumors of rs are common
cervical cancer
most common cancer in women
it is a progressive disease (pre malignant lesion usually occur 10-12 years before the development of invasive carcinoma
caused by human papilomavirus (hpv)
diagnosis: since asymptomatic- regular cytological screening is necessary. clinical symptoms in late stages include, vaginal bleeding, abnormal discharge
vaginal cancer- the rarest
vulvar cancer
endometrial cancer- cancer of glandular epithelium of uterine lining
uterine sarcoma
ovarian cancer
sexual dysfunction
organic (ex. chronic illness) and psychological disorders can be implicated in sexual dysfunction
disorders of desire (inhibited sexual desire, decreased libido)can be a biological sign of depression or substance abuse
vaginismus- involuntary muscle spasm in response to penetration due to prior sexual trauma or fear of sex
anorgasmia (orgasmic dysfunction)- inability to achieve orgasm due to chronic illness (ex. diabetes, alcoholism, hormonal deficiencies)
rapid orgasm- after orgasm- little interest in sex (chain of events that could occur)
dyspareunia (painful intercourse)- women may have pain during arousal, orgasm, or initiation of intercourse due to ex. lack of lubrication
impaired fertility
infertility
inability to conceive after 1 year of unprotected sex with the same partner
fertility can be impaired by factors in the man, woman, or both
fertility tests
structural
hormonal
disorders of the male reproductive system
disorders of the urethra
urethritis
inflammation of the urethra usually, but not always, caused by a sexually transmitted disease
nonsexual origins can be due to urologic procedures, insertion of foreign objects, anatomical abnormalities, or trauma
urethral strictures
fibrotic narrowing of the urethra caused by scarring
commonly due to trauma or untreated or severe urethral infections
disorders of the penis
phimosis and paraphimosis in which penile prepuce (foreskin) is ‘too tight’
phimosis
the foreskin has a narrow opening
the inability to retract foreskin from the glans of the penis (distal to proximal)
paraphimosis
inability to replace or cover the glans with the foreskin (proximal to distal) leads to formation of constricting band around penis
frequently caused by poor hygiene or chronic infections
penile cancer
carcinoma of the penis is rare
mostly squamous cell carcinomas
disorders of the scrotum, testis, and epididymis
disorders of the scrotum
varicocele, hydrocele, and spermatocele are common disorders
varicocele
inflammation/dilation of veins in the spermatic cord
caused by inadequate or absent valves in the spermatic cord
varicocele reduces blood flow to the testicles and interferes with spermatogenesis
the blood flow/blood drainage is inefficient (it pools) which can interfere with temperature and the microenvironment
hydrocele
scrotal swelling due to collection of fluid within the tunica vaginalis
imbalance between fluid secretion and reabsorption
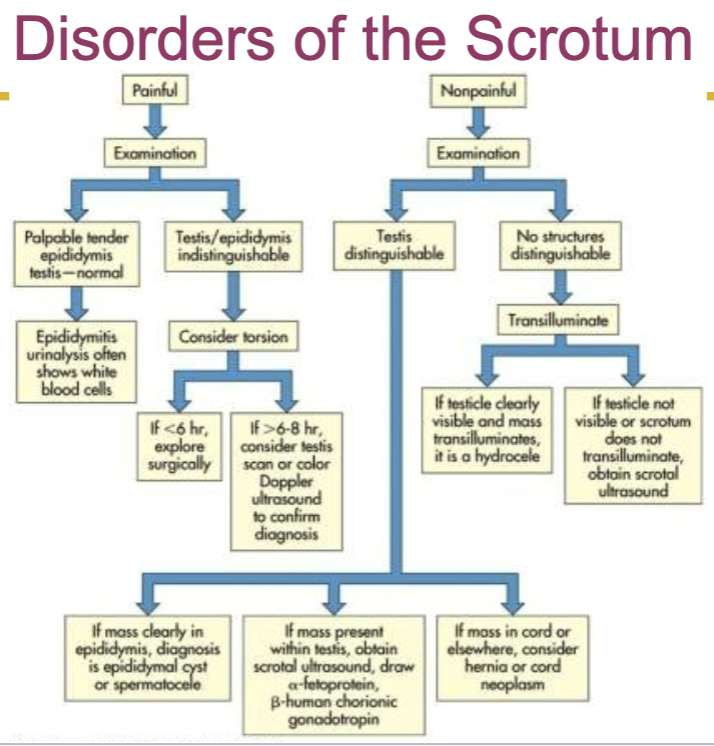
disorders of the testis
cryptorchidism
failure of one or more of the testes to descend from the abdominal cavity into the scrotum
ectopic testis
testis that has strayed from the normal pathway of descent
diagnosis in both cases is based on physical examination
treatment: hormone (gnrh, hcg) may initiate descent, if not, surgery
torsion of the testis
rotation of the testis
the rotation causes the twisting of the blood vessels in the spermatic cord
painful and swollen testis
condition may be spontaneous or follow physical exertion or trauma
if cannot be corrected manually, surgery must be performed
disorders of the epididymis
epididymitis
inflammation of the epididymis
common in sexually active young men
the pathogenic microorganism reaches the epididymis by ascending the vas deferens from an already infected bladder or urethra
pain is the main symptom
treatment include
antibiotics
symptom relief medication
disorders of the prostate gland
benign prostatic hyperplasia
enlargement of the prostate gland
symptoms associated with urethral compression
relationship to aging (80% of men before ag 80 will experience it)
evaluation
digital rectal exams
prostate specific antigen (psa) monitoring
prostitis
inflammation of the prostate
normal protective barriers
similar symptoms to bph
prostitis can be
acute bacterial
chronic bacterial
nonbacterial
cancer of the prostate
95% of prostate neoplasms are adenocarcinomas and demonstrate peripheral zone growth
prostatic cancer is asymptomatic until its advanced stages
symptoms are similar to bph
causes: dietary factors, hormones (ex. androgen), vasectomy, familial factors
male sexual dysfunction
in males, normal sexual response includes: erection, emission, and ejaculation
the causes of sexual dysfunction due to organic factors are
vascular
vascular disorders can prevent erection
endocrine
can reduce testosterone production
neurologic disorders
can interfere with sympathetic and parasympathetic innervations needed for erection
chronic diseases
renal failure and diabetes mellitus
penile diseases and penile trauma
iatrogenic factors
surgery and pharmaceuticals
impairment of sperm production and quality
spermatogenesis require hormone and growth factors
fsh, lh, and testosterone
androgen binding protein, inhibin b, and other peptides
adequate spermatogonia
sperm count >= million/mL
spem motility
antisperm antibodies
drugs and toxins in the semen
disorders of the breast
galactorrhea
persistent and sometimes excessive secretion of milky fluid from the breasts of a woman who is not pregnant or nursing
galactorrhea can also occur in men
women with galactorrhea also experience menstrual abnormalities
breast cancer
most common cancer in american women
leading cause of death from ages 40-44
second most common killer after lung cancer
reproductive factors
hormonal factors
environmental factors and lifestyle
radiation
diet
chemicals
physical activity
familial factors and tumor related genes
 Knowt
Knowt