PT lecture - week 1, block 2.2
Spinal complaints - low back/neck pain
THIS LECTURE IS USELESS, GO ANALYZE THE GUIDELINE
Low back/neck pain → MSK - problem
READ KNGF GUIDELINE
Introduction
Global burden disease
look at the MB lecture for epidemiology, costs, prognostic factors
GP role → pick the ones that have a serious pathology
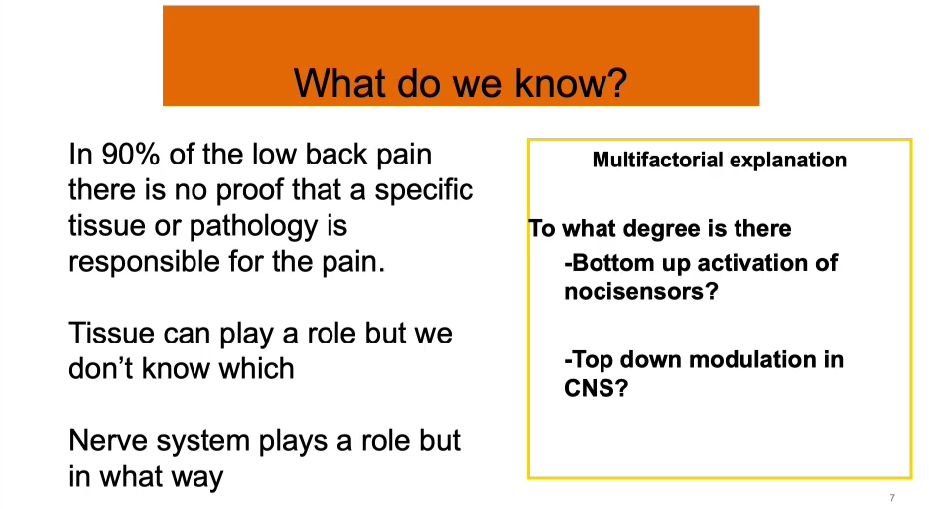
“non-specific complaints”
The majority of patients have “non-specific complaints“ → we say to patients “low back pain“
90%
multifactorial (MB lecture)
Episodic
Clinical presentation vary strongly
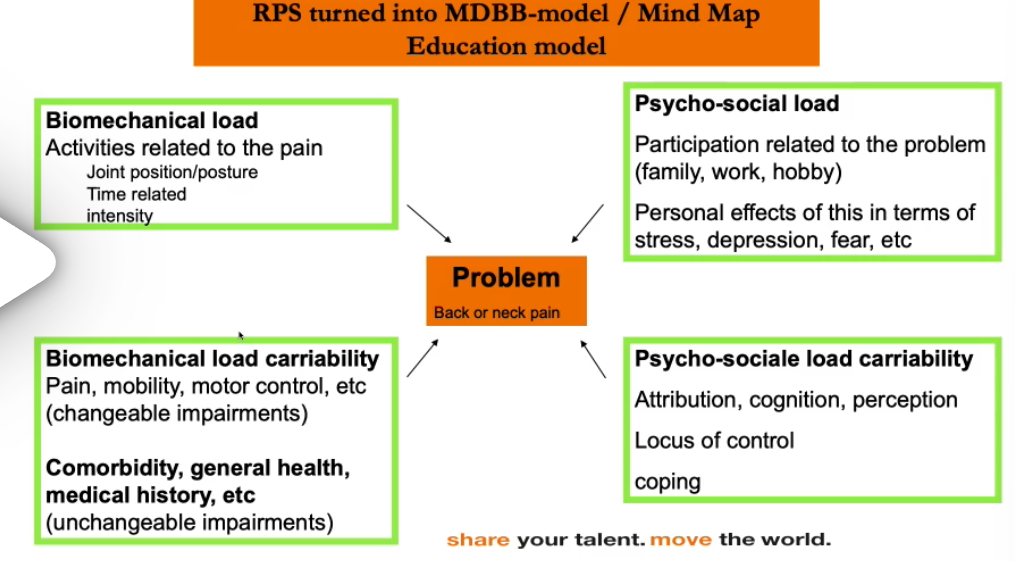
How do we look at the patient?
tissues
Biopsychosocial → ICF, MLCM
Understanding of pain is very important
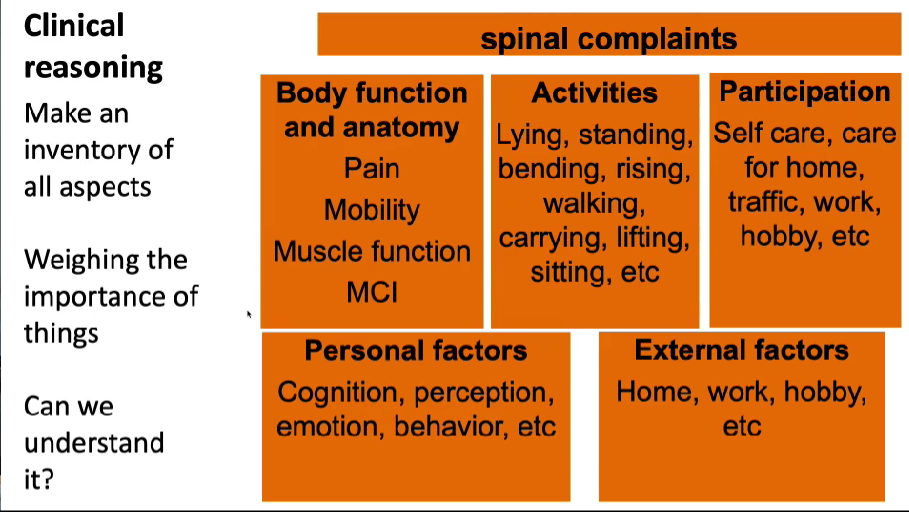
Clinical reasoning
We need to understand why they are in pain
We need to explain the pain to the patient
Guidelines → read it
appropriate care
less money for society
relevant research
In the guidelines, the patients are categorized based on
1) their prognostic factors
2) persisting pain complaints
The patient needs fitting care for their complaints
There is not one kind of low back pain patient
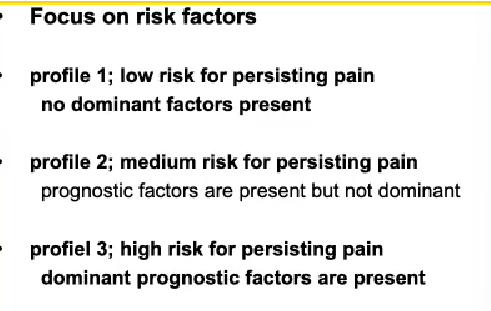
each profile has a specific plan
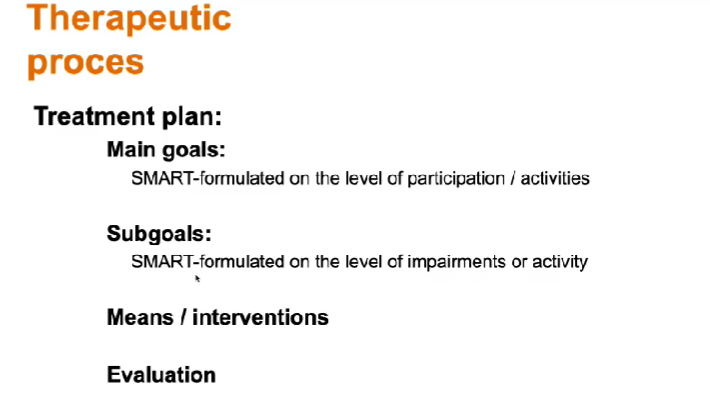
Time-related, goal-oriented, interventions, dosage, amount of treatments
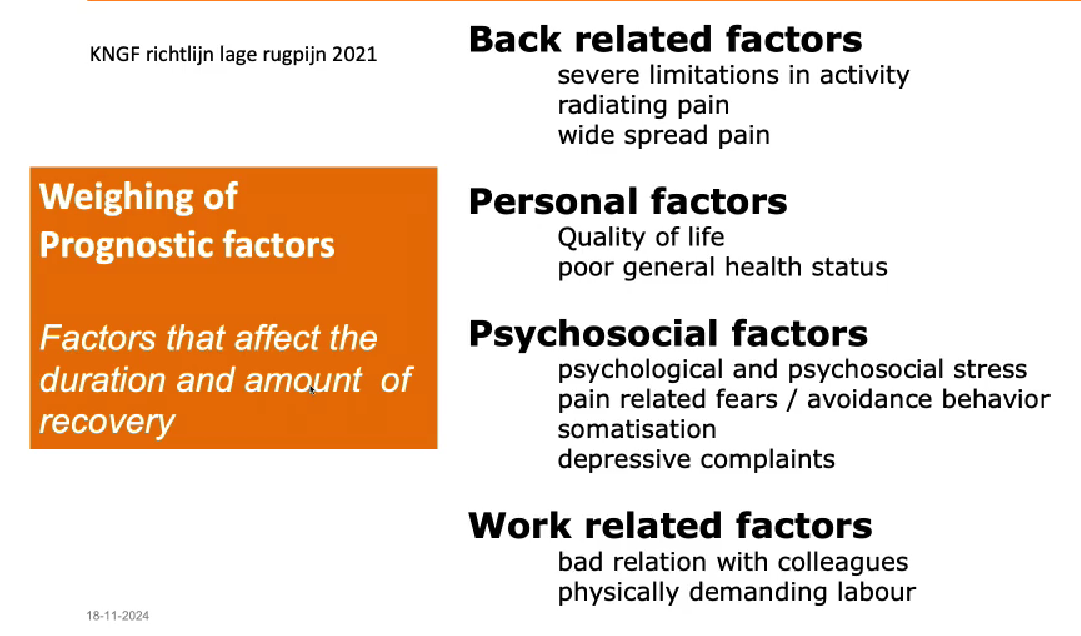
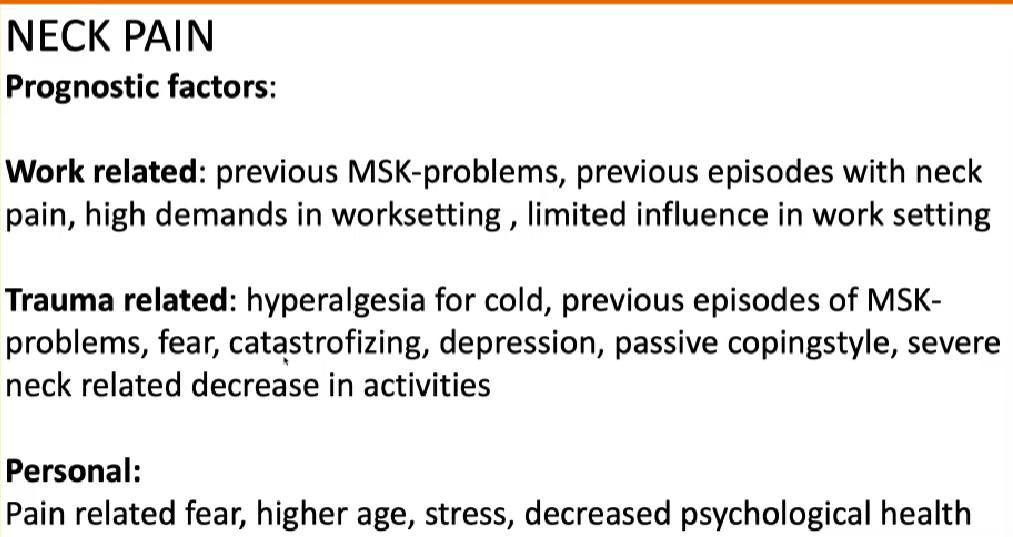
Prognostic factors
Profile 1
Management strategy of the normal course
informing, reassuring, advising
Be aware of the use of language
Gradual increase activities that promote recovery
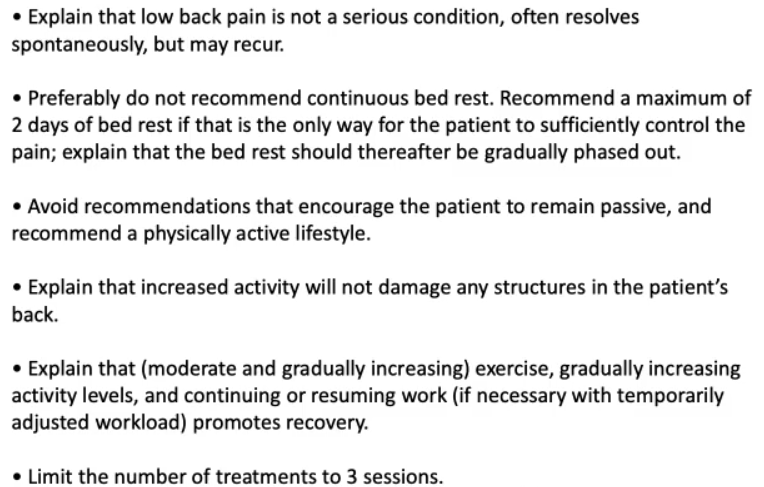
Decrease in pain between 10 - 12 weeks
window of opportunity of 3 months
After that pain becomes systematic
explain the natural course of pain, and make sure they understand they are in control
Profile 2
As in Profile 1, plus:
Design an exercise program that fits in with patients’ needs and your expertise and experience as a therapist
Limit the use of passive therapies
Focus on self-efficacy
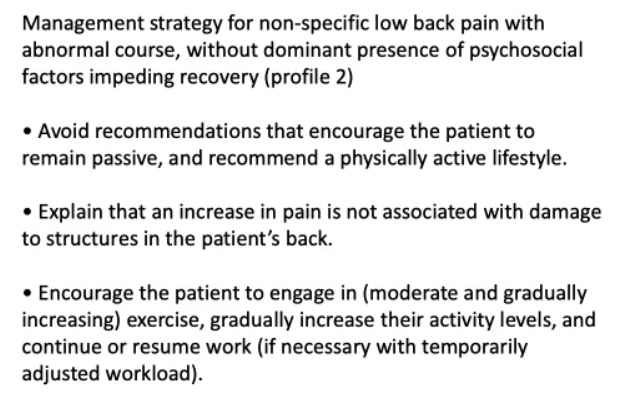
more pain doesn’t equal more damage
Profile 3
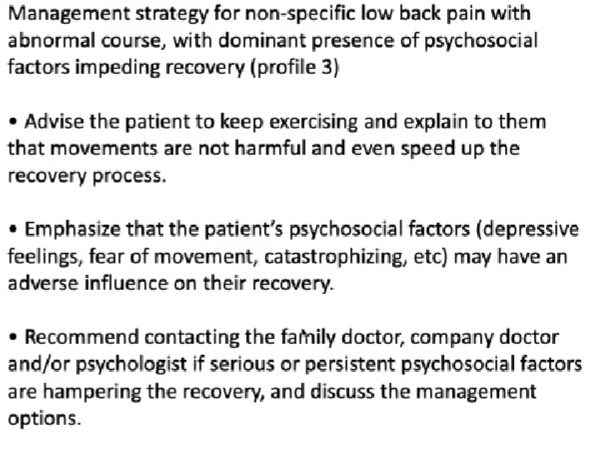
Pain education → discuss the factors that might hinder the recovery
change the perception of pain
people are scared to make more damage because they feel more pain
Self-management
Advise to stay active → gradual increase in activities
Graded activity program → time contingent
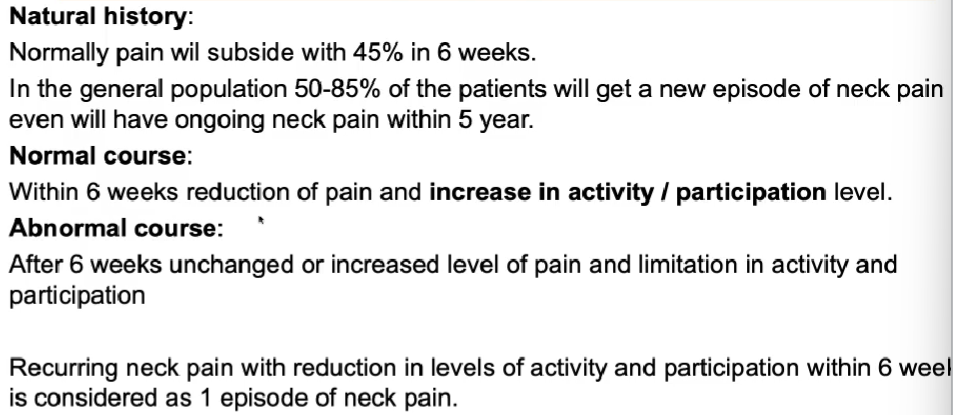
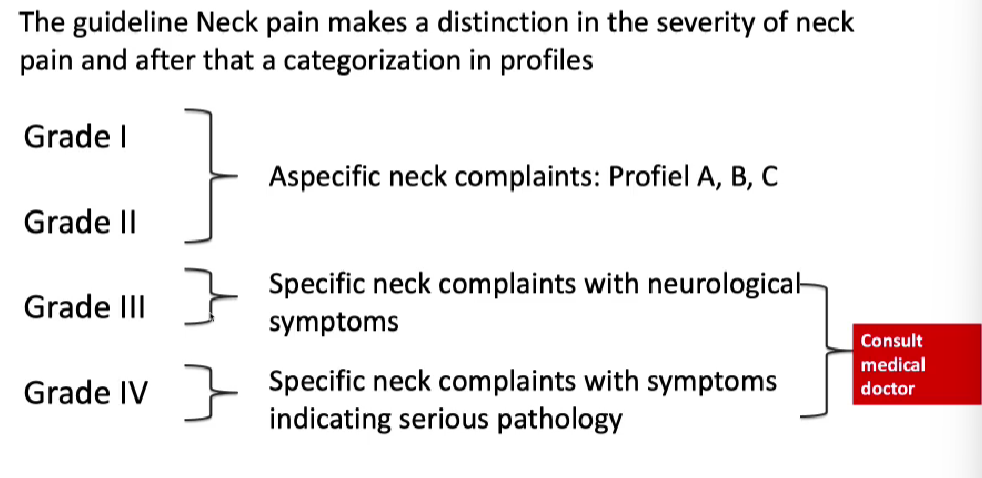
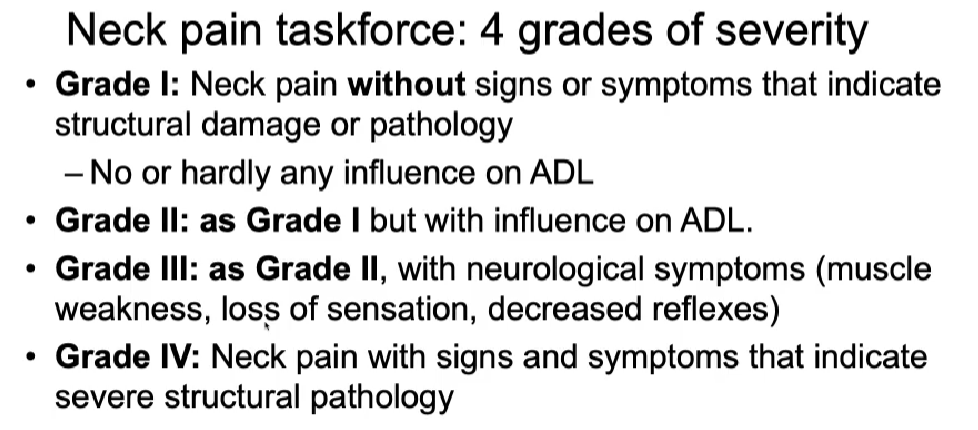
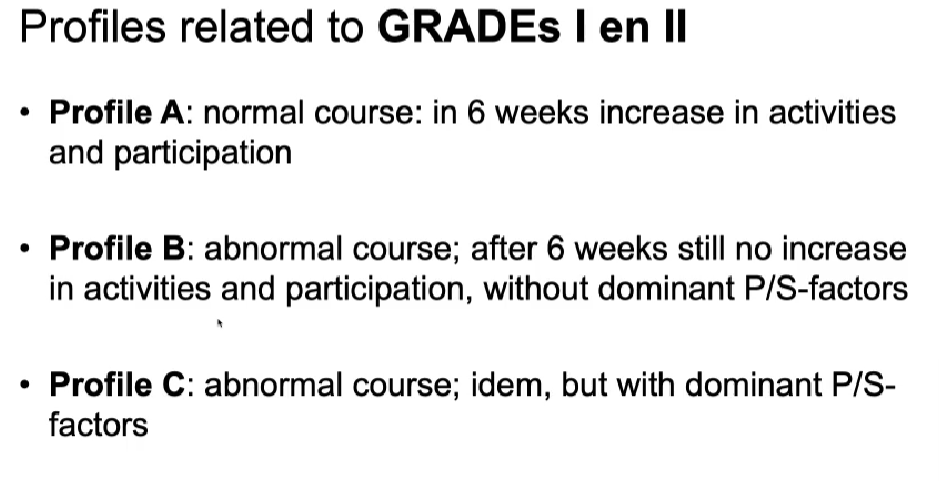
Guideline Neck pain
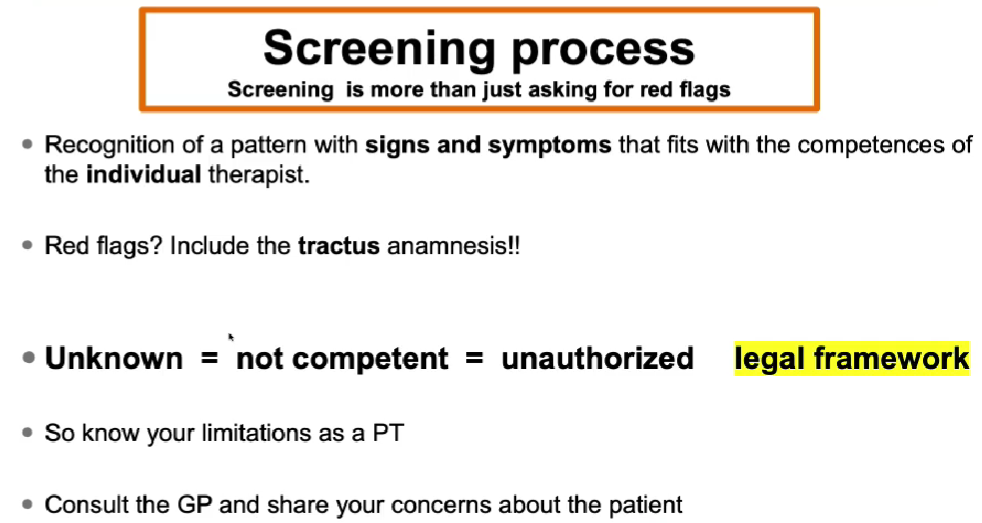
Red flag
Abnormal course If the neck pain keeps increasing → send to GP
DAP
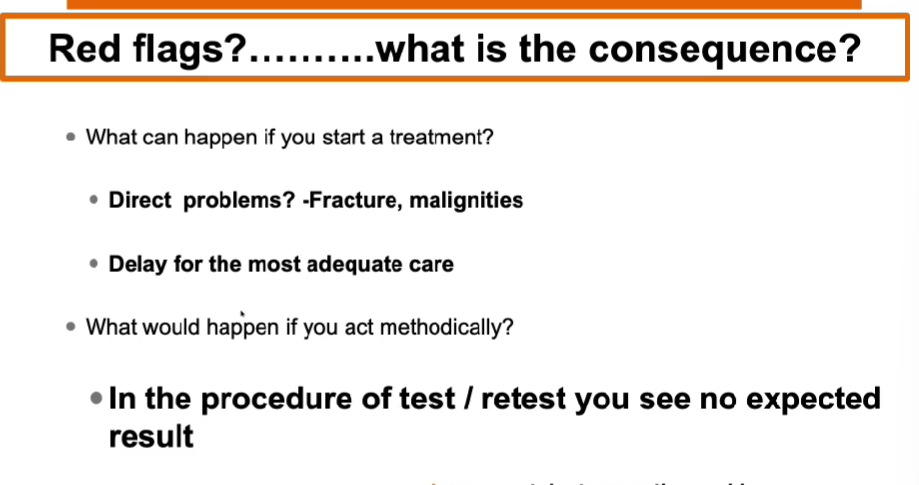
Responsibility
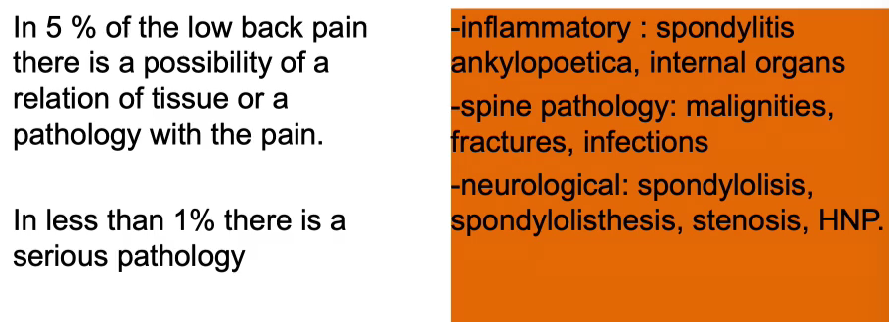
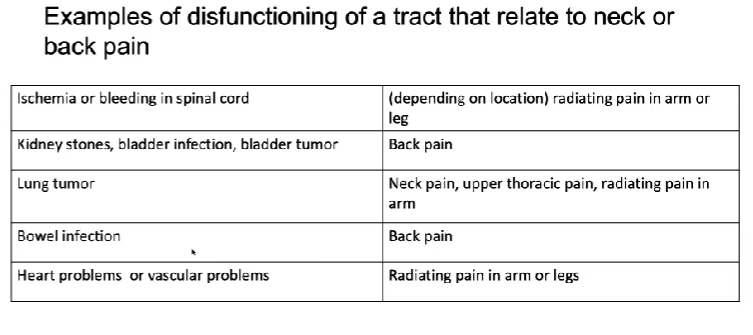
Identify serious pathology ( non-specific) spinal complaints
Only 1 % of all patients
Limit the delay in adequate care!
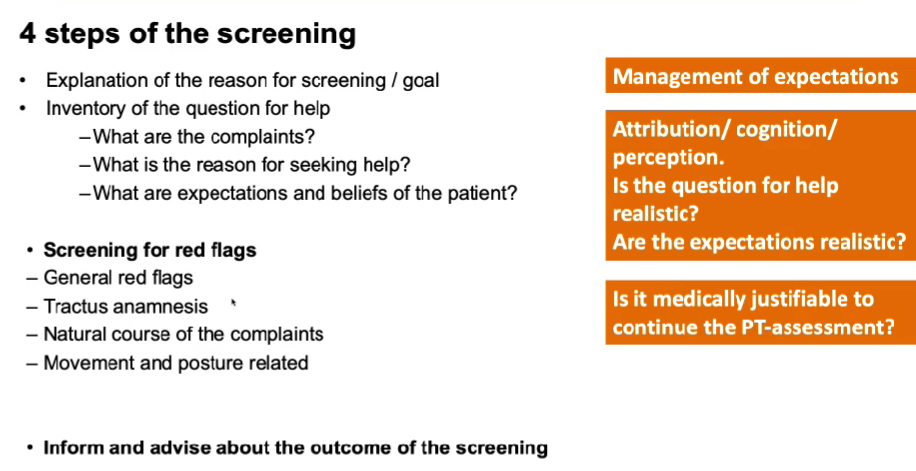
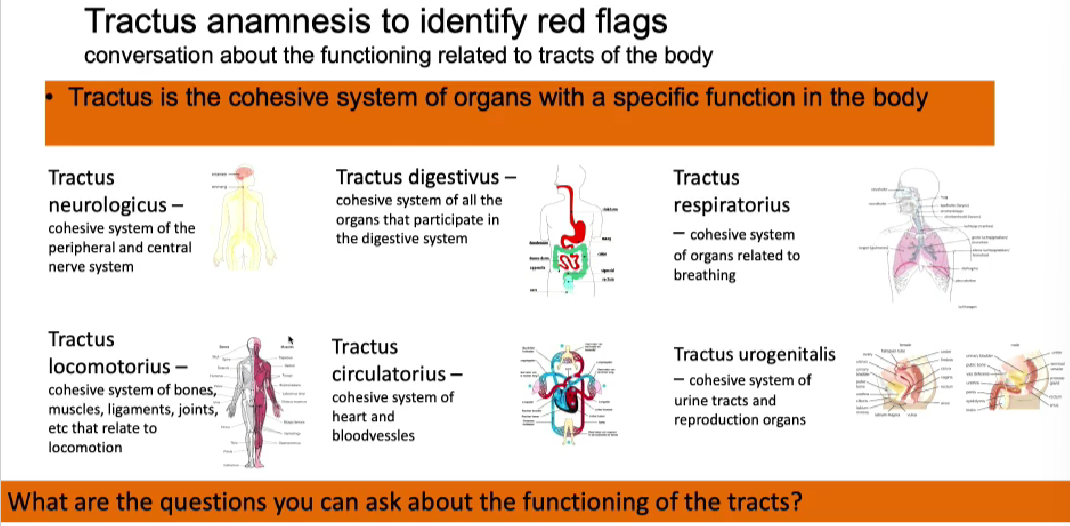
From this tract, check the ones that might be involved with neck pain
tractus respiratorius → if you are physically active, does the pain get worse
Tractus circulatorius → do you have excessive increase in respiration, do you have pain in the shoulder blades, pain in the left arm
Tractus neurologicus
Tractus locomotorius
Tractus digestivus
Tractus urogenitalis → do you have problems urinating, bowel, problem with intercourse
Dizzy? could puke? → 991
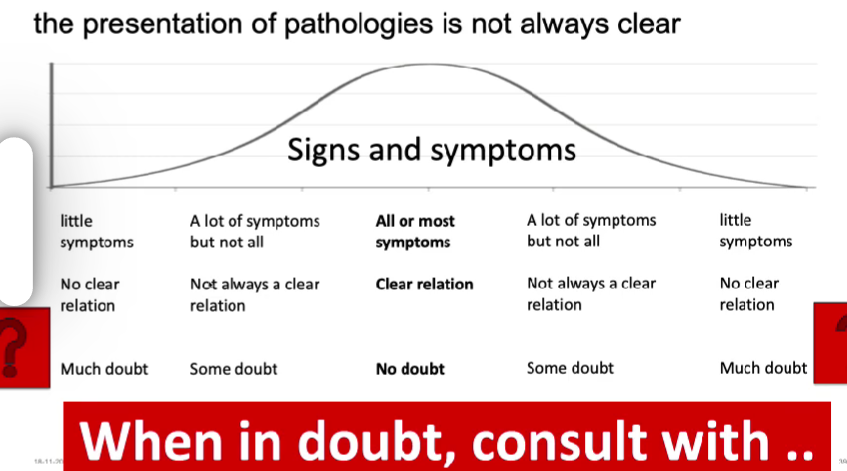
Don’t hesitate to contact the GP
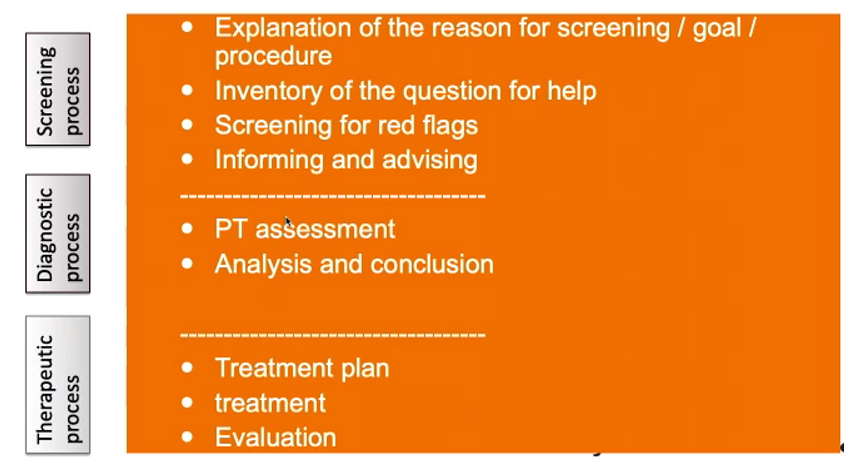
After screening, as usual:
anamnesis (SCEBS)
Physical examination → inspection, totally/local, functional
Palpation
Rom
specific testing
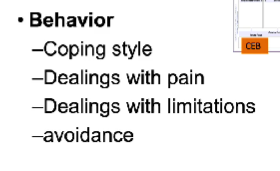
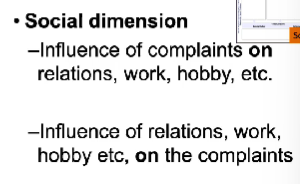
SCEBS
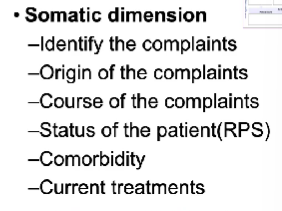
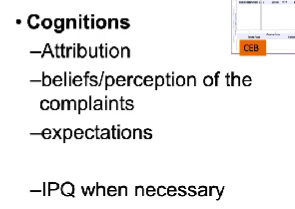
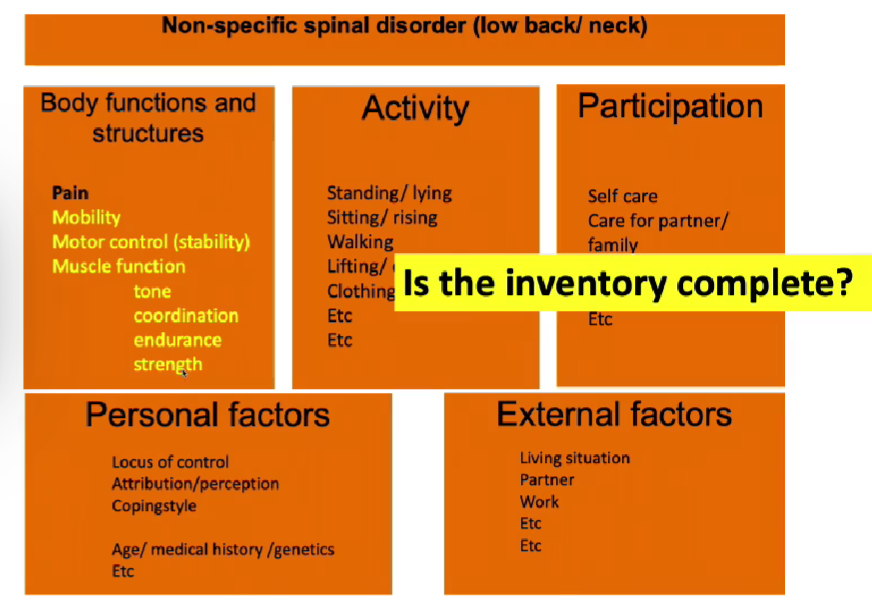
can I estimate the profile?
What are the prognostic factors?
What further info is necessary?
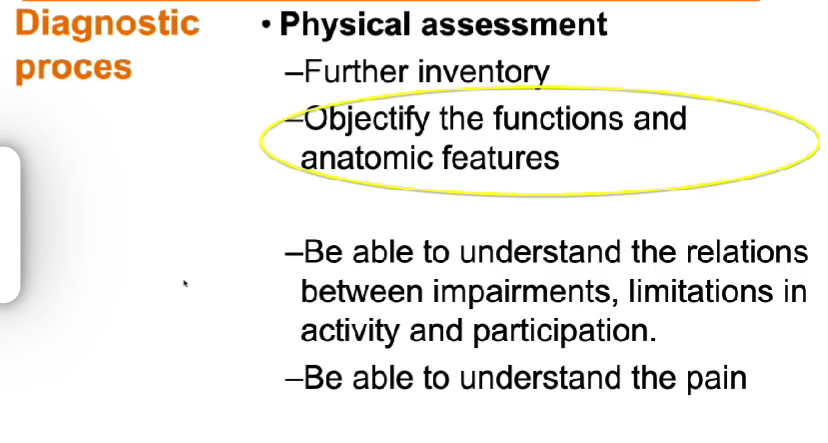
Can we understand the pain mechanism?
RPS