Chapter 10: Dysphagia
Dysphagia
- Dysphagia - a difficulty in swallowing or an inability to swallow
- A swallowing problem affects a person’s ability to eat, which serves 2 primary purposes:
- Nutrition and hydration
- Pleasure
- Dysphagia impairs a person’s ability to participate in social gatherings or events
Examples of Dysphagia
- Aspiration - when food enters the airway
- Aspiration occurs because - weak or paralyzed pharyngeal and laryngeal muscles
Role of the SLP
Approximately 30% of SLP are involved in the management of swallowing
SLPs are a key component of a dysphagia team (ENT, OT, SLP, radiologist, PT, primary care physicians, nutritionist, nurses)
Communication and swallowing problems co-occur because these two activities share some common structures and functions

Stages of Swallowing
The Anticipatory Stage
- Occurs before the food reaches the mouth
- Sensory information
- “prepare to eat”
The Oral Stage
- Voluntary control
- Preparatory phase part of the oral stage, the bolus is being readied for the swallow
- Transport phase begins when the tongue pushes the bolus against the palate, moving it in a backward direction toward the pharynx
The Pharyngeal Stage
- Begins with the triggering of the pharyngeal swallow
- Purposes - to protect the airway, to direct the bolus toward the stomach
- Velum elevates and contracts to close off the velopharynx so that food cannot enter the nasal cavity
- Larynx and hyoid bone move upward and forward
- Larynx closes to prevent food from entering the airway
- Epiglottis comes over the larynx to provide additional airway protection
- When the swallow is triggered, pharyngeal peristalsis is initiated - contractions that move the bolus through the pharynx toward the esophagus
The Esophageal Stage
- Begins with the lowering and backward movement of the larynx and the resumption of breathing
- Upper esophageal sphincter contracts
- Bolus moves through the esophagus to the stomach in a series of peristaltic waves
Dysphagia in Adults
- Swallowing requires both cognitive and motor skills
- Causes of Swallowing Disorders
- Cerebrovascular Accident (CVA) - aka stroke
- Brain Stem Stroke
- TBI
- Dementia - cognitive issues/hold food in mouth
- Neuromuscular Disease - MS, ALS, PD, MG
- Cancer - surgery changes the anatomy, radiation causes tissues to become “stiff”
Symptoms of Dysphagia
- coughing or choking during swallowing
- change in voice or speech (sounds gurgle-y)
- repetitive swallows or progressive need to clear throat
- regurgitation, immediate or delayed (pharyngeal and nasal or esophageal and gastric)
- weakness; lack of control of head and neck musculature
- fullness/tightness in throat
- pain, localized or radiating (e.g., functional chest pain may occur in patients with somatic concerns, anxiety, or depression)
- odynophagia (pain on passage of bolus)
Management of Adult Dysphagia
- History
- Bedside evaluation
- Instrumental evaluation
- Determine treatment plan based on these results
- Team - SLP, OT, PT, nurses, nutritionists, radiologists, neurologists, gastroenterologists, pulmonologists
Assessment
Questions to be Determined
- Is the patient aware of the food on his plate, can he feed himself?
- Are the muscles of the tongue, lips, and jaw able to adequately prepare a bolus?
- Do the pharyngeal and laryngeal muscles have enough strength and movement to elevate the larynx to close off the airway and direct the bolus to the esophagus?
- Can the patient eat safely (with no aspiration) and maintain adequate nutrition?
History
- Collect relevant feeding, behavioral, and medical information
- Pre-existing conditions, medications
- Medically stable?
- Respiratory status
- Current cognitive functioning
Current Medical Status
- How the person is presently receiving nutrition
- IV
- NG tube - placed in the nose and goes to the stomach
- G tube - tube surgically placed directly into the stomach
- People can still aspirate on an NG or G tube if they have reflux
Bedside Clinical Assessment
- Meets with the patient and assesses his/her ability to take food off the plate, prepare the bolus, and safely swallow
- Oral Mech Exam, assesses ability to follow directions, level of alertness
- Directly observe the oral phase
- Unable to view the pharyngeal phase, but can watch for signs:
- Neck along with placement of 2 fingers under the chin to determine whether there is upward and forward laryngeal movement
- Listening for coughing, which would mean the bolus went down the wrong way
- There could be a silent aspirator - they aspirate but do not cough
- Listening for a “gurgly” sound after swallowing which might indicate that part of the bolus is on the vocal folds
- Pharyngeal stage of the swallow can not be diagnosed by the bedside evaluation
- When pharyngeal stage problems are suspected, the SLP can conduct an additional assessment procedures
Instrumental Assessment of Dysphagia
- An instrumental assessment is used to gain a better understanding of pharyngeal stage functioning
Modified Barium Swallow Study (MBS/MBSS): this procedure is a fluoroscopic image that is recorded on videotape
- SLP and radiologist perform this procedure together
- SLP places barium coated food and liquids into the patient’s mouth
- Radiologists takes a moving picture
- Pharyngeal stage functioning can be visualized
Endoscopy (FEES)
- Flexible scope is inserted through the nose and positioned just above the epiglottis
- Patient is given food mixed with dye
- Patient east the examiner observes the pharyngeal structures and functions
Treatment Planning
- Team determines treatment
- Plans often include:
- Positioning - chin tuck
- Environmental modifications - eat in a quiet environment (need more cognitive status to follow strategies)
- Adaptive feeding equipment - Provale cup, Safe straw
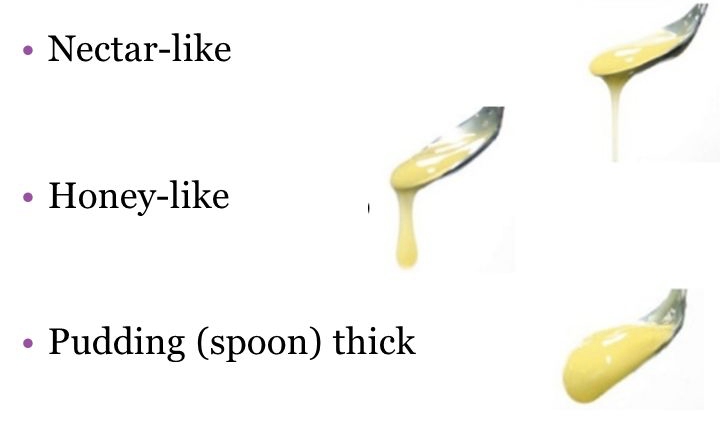
- Bolus modification
- Swallowing techniques - ex. effortful swallow - concentrate on tensing all of the throat during swallows
- Chin Tuck - Decreases airway diameter
- Safe Straw - Limits sip size
- Provale Cup - Limits sip size
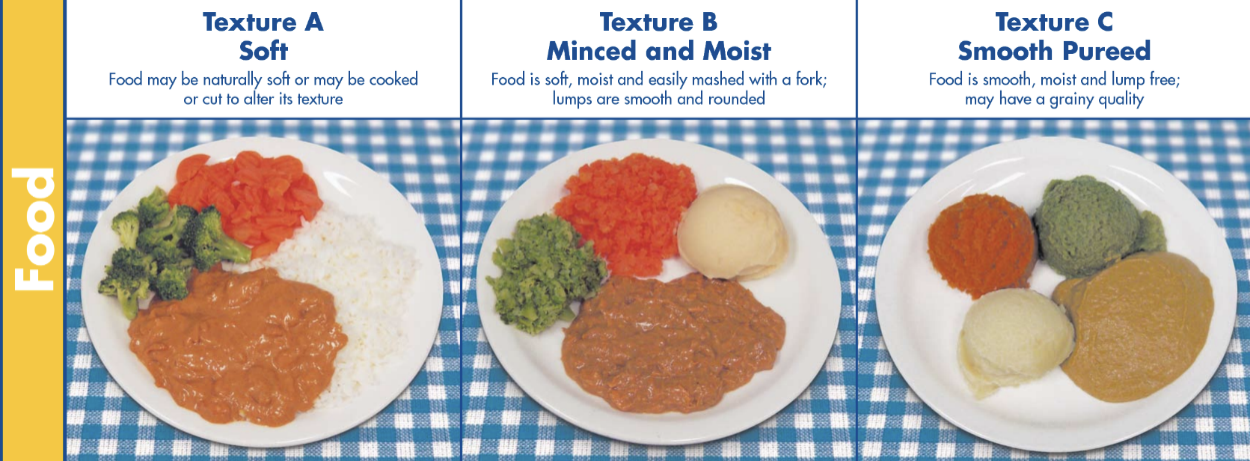
Examples of Modified Diets
Dysphagia in Children
- Pediatric dysphagia: the SLP treats children who have yet to acquire normal eating skills
- Various etiologies have prevented the development of normal swallowing patterns
- Respiratory: suck/swallow/breathe
- Sensory deficits: food textures
- Cleft Lip/Palate
- Goal of dysphagia assessment and treatment with children is to - Aid in the development of skills needed to keep the child safe and well nourished
- Prematurity
- Ability to suck/swallow develops prenatally
- Premature baby may not have the ability to suck milk from a nipple
- Weak facial muscles, underdeveloped lungs
- Uncoordinated suck/swallow, weak suck, breathing disruptions
- CP
- Wide range depending upon the degree of motor deficit
- Often see increase in muscle tone, decrease in ROM
- Cognitive deficits
- Child with CP is often a slow, inefficient eater with a high risk for aspiration
Pediatric Dysphagia Evaluation
- Review Medical and Feeding History and Current Feeding Methods
- Bedside Clinical Assessment
- Instrumental Assessment
- Conduct the MBS in the child’s current seating system
- Use food textures that are similar to what the child currently eats
- Use the child’s own utensils- bottle, special cup, spoon, etc.
Pediatric Treatment Planning
First goal - Child meet current nutritional needs while remaining safe so the child can grow and remain healthy
Second goal - Normalizing the child’s eating and swallowing skills
- Dietician, SLP, Physical Therapist