STUDY GUIDE UMBILICAL CORD & AMNIOTIC FLUID
UMBILICAL CORD
2 arteries, 1 vein
it may be spiraled or helical.
All aspects of umbilical cord development are complete by 10 to 11 weeks gestation.
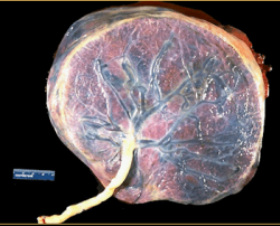
The normal umbilical cord is shown with its placental insertion site and is covered by a glistening layer of amnion.
51-61cm average length
arteries are longer than vein
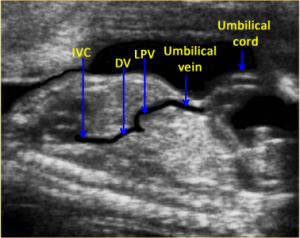
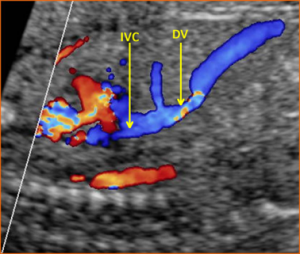
Single umbilical vein carries oxygenated blood into ductus venosus to be sent to IVC, then heart for recirculation
2 umbilical arteries carry deoxygenated blood back to placenta for oxygen exchange
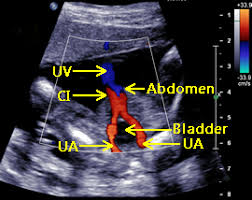
The umbilical arteries are branches of the fetal internal iliac arteries and bring deoxygenated blood from the fetus to the placenta.
Each artery courses around the fetal bladder and enters the umbilical cord at the abdominal CI (cord insertion site).
The umbilical vein brings oxygenated blood from the placenta to the fetus and enters the fetal liver at the abdominal cord insertion site.
About 50% of the umbilical venous blood is shunted through the ductus venosus to the inferior vena cava before entering the right atrium..
Normal arterial flow is low resistance with good diastolic flow
Increased resistance will cause decreased diastolic flow which indicates increased resistance to flow in the fetus
Wharton's jelly - surrounds vessels in cord for protection
Three vessels
Three areas to assess
Placental attachment
Free loop
Entry into the abdomen
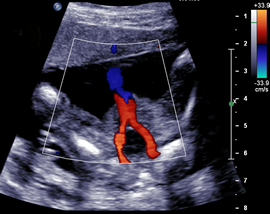
Above. Color power Doppler demonstrating both the placental cord insertion site and the abdominal cord insertion site. The umbilical cord (UC) diameter increases in size from 8 to 15 weeks. The UC diameter correlates with1 gestational age (GA), crown rump length (CRL), and biparietal diameter (BPD). By the end of the first trimester, there is normal blood flow in the mid-gut area.
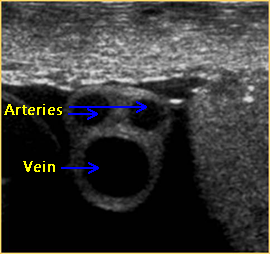
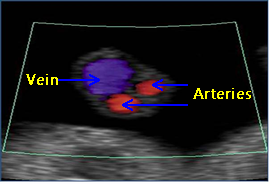
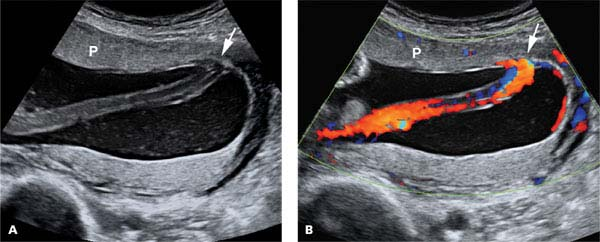
Above. 2-D gray scale demonstrating abdominal cord insertion site. At 18 to 23 weeks, the umbilical cord diameter measured at the insertion into the fetal abdominal wall correlates with2 gestational age (GA) and estimated fetal weight (EFW).
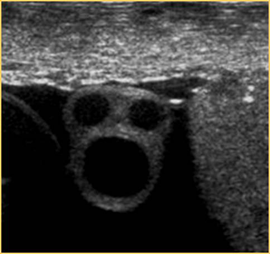
Above. 2-D gray scale. Transverse view of the fetal abdomen. Note UC (umbilical cord) insertion at the fetal abdomen with a view of the UV (umbilical vein) with its entry into the fetal liver. At 24-39 weeks, the umbilical cord cross sectional area measured at insertion into fetal abdominal wall correlates with3 gestational age (GA).
Umbilical Cord Anomalies
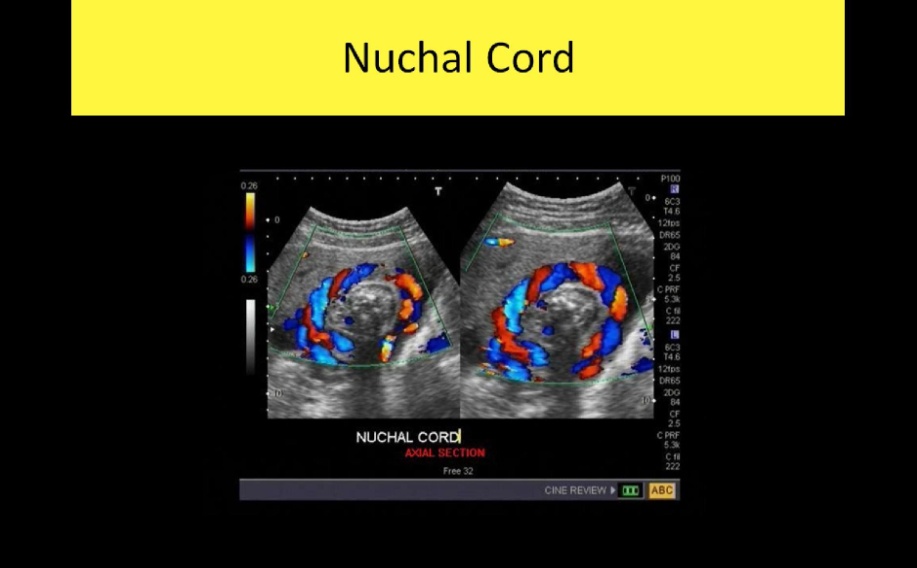
Nuchal Cords
A nuchal cord occurs when the umbilical cord becomes entangled at 360 degrees around the fetal neck
The prevalence of nuchal cords at birth is around 22% of all pregnancies with no significant statistical association between the presence of a nuchal cord and stillbirth
On the other hand, multiple loops of nuchal cord have been associated with abnormal fetal heart rate pattern during labor, low umbilical artery pH, an increased likelihood of Cesarean section or operative deliveries and an Apgar score < 7 at the 5th minute
Tight nuchal loops are associated with a low Apgar score but not with an increased admission to the neonatal intensive care unit (NICU).
Loose loops of nuchal cord are associated with a favorable in utero prognosis and perinatal outcome.
Vasa Previa
Vasa previa is a rare obstetrical pathology that affects 0.046% of all pregnancies, in which the fetal blood vessels are located within the membranes, not in their usual location protected by the umbilical cord or the placenta, and cover the internal cervical os
Vasa previa is classified into three types:
Type I, when there is one single placental lobe with a velamentous cord
Type II, when the unprotected fetal vessels connect two lobes of a succenturiate lobed or bilobed placenta, near the cervix
Type III, when the fetal vessel runs within the membranes, near the cervix, but is not associated with a velamentous cord insertion or bilobed placenta
Vasa previa has a resolution rate varying from 14% to 39% up to 28 weeks of gestational age, especially if diagnosed before 24 weeks of gestation, if not covering the internal cervical os and when not associated with placenta previa
These unprotected vessels are susceptible to rupture or compression, impairing fetal vascularization
Perinatal survival rate is dependent on appropriate prenatal diagnosis and improves from 72% versus 97% when vasa previa is detected antenatally
Transvaginal ultrasound and color Doppler ultrasound are the gold standard diagnostic modalities however, due to the low incidence of this condition, there are no population screening protocols, and the screening approach is indicated only in high-risk patients, such as low-lying placenta/placenta previa, velamentous cord insertion, ART and multiple gestations
Elective Cesarean section should be planned around 35 weeks and not after 37 week’s gestation
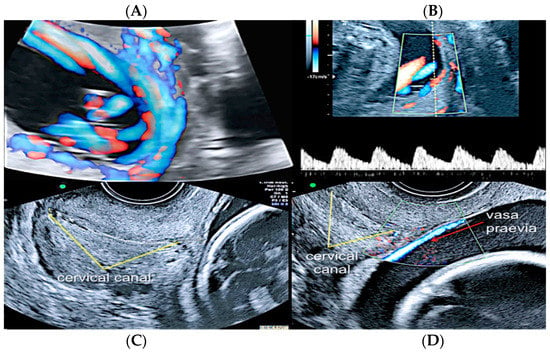
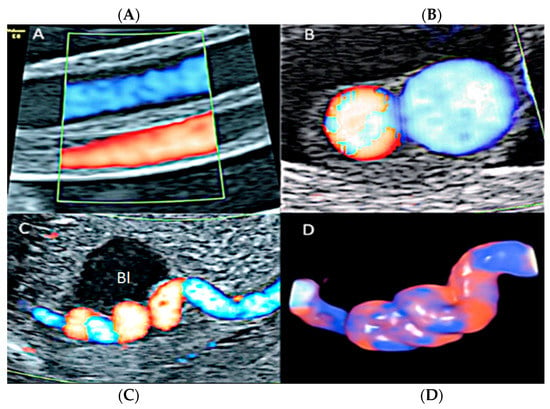
Second trimester transvaginal scan and three-dimensional ultrasound with “glass-body” rendering (A), Doppler ultrasound (B) and two-dimensional ultrasound showing the anatomical relationship between the cervical canal (yellow lines) (C) and the presence of vasa previa (red arrow) (D).
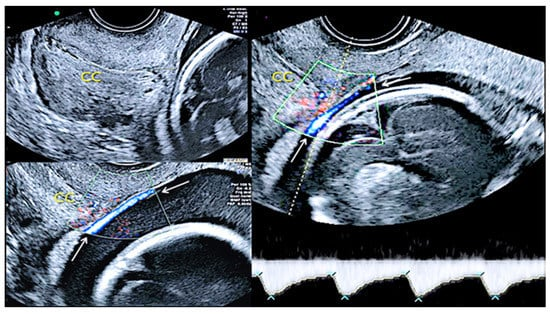
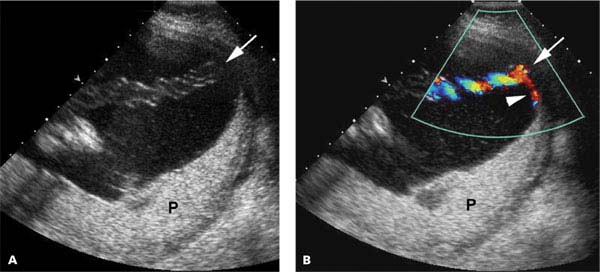
Pregnancy at 24 weeks’ gestation. Two-dimensional ultrasound, color and pulse wave (PW) spectral Doppler ultrasound allowed the detection of an arterial vessel close to the internal cervical os (vasa previa Type III, white arrows (Legend: CC: cervical canal).
Velamentous Umbilical Cord Insertion
Velamentous cord insertion is one of the abnormal cord insertion types, in which the vessels run through the amnion and chorion, unprotected by Wharton’s jelly, before reaching the placental plate
This abnormality is present in 1.5% of singleton pregnancies
Associated with several unfavorable perinatal outcomes, such as fetal growth restriction, placenta previa, placental abruption, fetal heart abnormalities during labor, emergency Cesarean section, preterm labor, low Apgar scores, admission to the NICU and neonatal death, as the velamentous vessels can be compressed during uterine contractions and fetal movements
The risk factors associated with this condition include bilobate/succenturiate placenta, ART, multiple gestation and a prior history of abnormal placental cord insertion
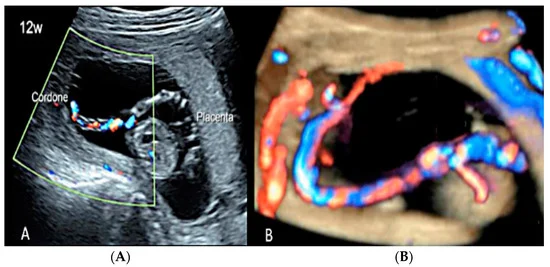
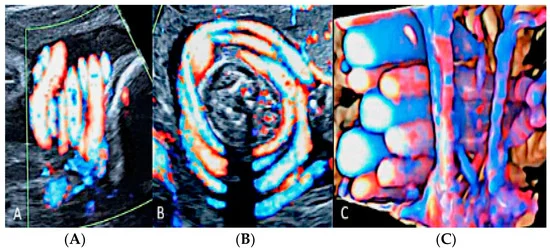
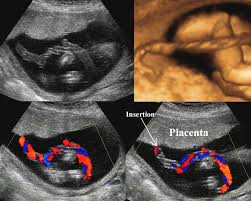
(A,B) First trimester (12 weeks) scan showing in two-dimensional- and three-dimensional color Doppler ultrasound a velamentous cord insertion (Cordone: umbilical cord).
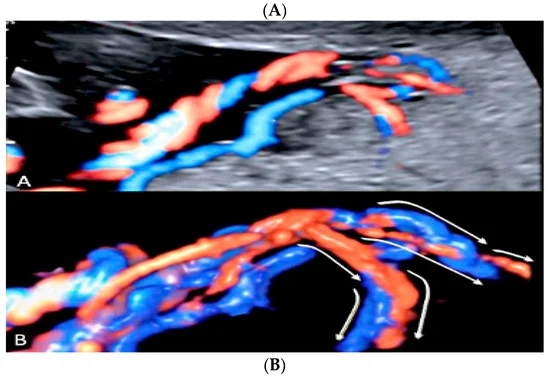
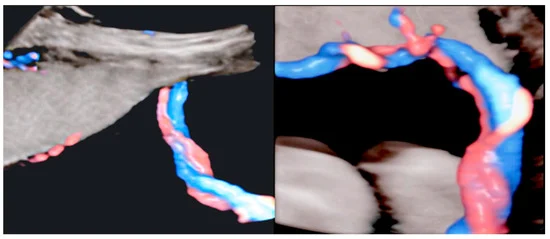
Pregnancy at 19 week’s gestation (same case of the previous figure). Two-dimensional color Doppler ultrasound (A) and four-dimensional color Doppler STIC volume (B) diagnosed velamentous cord insertion.
Velamentous cord insertion into the placental membranes (A) with direction of blood flow indicated by curved arrows and pathologic correlation (arrows) (B).
Marginal Umbilical Cord Insertion
Marginal umbilical cord insertion is another anomaly, in which the umbilical cord is inserted into the placental margin within 2.0 cm
It is present in 6.3% of singleton pregnancies and presents much lower chances of complications than velamentous cord insertion

Furcate Umbilical Cord Insertion
Furcate umbilical cord insertion is a condition where the umbilical vessels separate before they insert into the placental plate and lose their Wharton’s jelly
It is present in 0.1% of pregnancies and is considered a variant not well distinguished from velamentous cord insertion
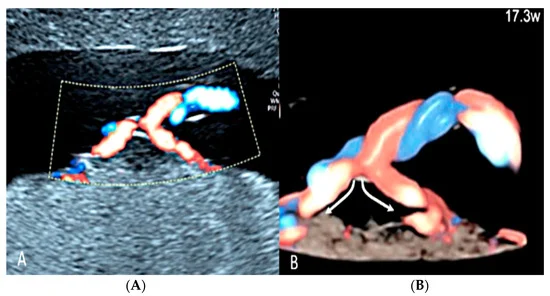
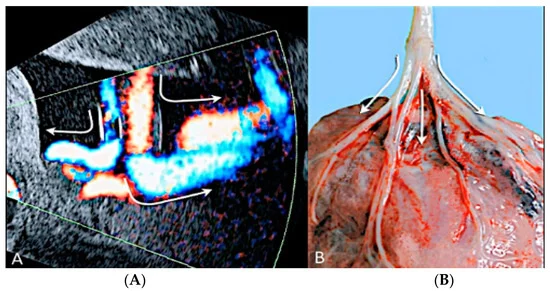
Furcate umbilical cord insertion using two-dimensional ultrasound (A) and three-dimensional ultrasound (B) with HD-Flow™ Doppler: the dichotomic direction of the umbilical blood flow is clearly demonstrated at 17.3 week’s gestation (arrows).
Umbilical Cord Entanglement
Umbilical cord entanglement is a condition exclusively of monoamniotic twin pregnancies and occurs because both umbilical cords insert close to each other in the single placenta
The entangled cords can cause vascular damage for one or both fetuses and lead to fetal demise
Diagnosis can be made through the visualization of a branch pattern on color Doppler ultrasound at the level of the entanglement, and an end systolic notch seen on the umbilical artery waveform reflects vascular compression or narrowing
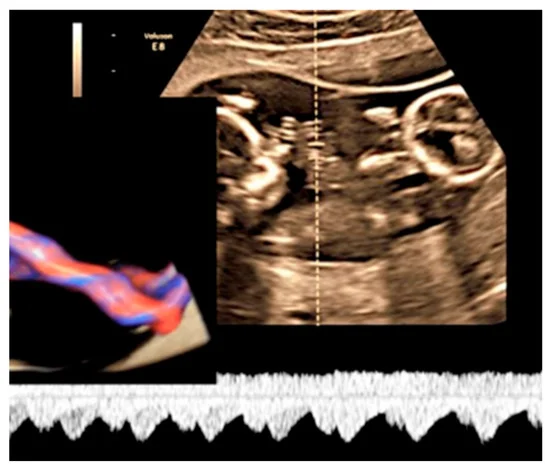
MCMA twin pregnancy. Cord entanglement can also be detected with the “galloping horse sign” that involves identifying two distinct waves signals with different heart rates obtained by sampling an apparently unique umbilical cord with pulse wave (PW) spectral Doppler ultrasound
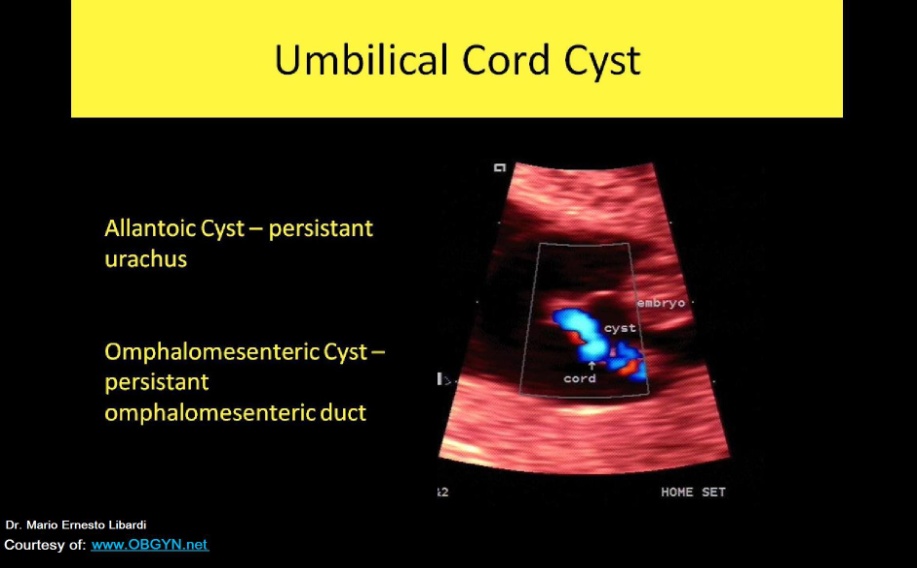
Umbilical Cord Cyst
Umbilical Cord Cyst:
Allantoic: persistent urachus forms cystic structure within cord
Omphalomesenteric: persistent omphalomesenteric duct form cystic structure within cord
Usually causes no related complications if blood flow unaffected
Umbilical cord cysts can be classified as true cysts and pseudocysts.
True cysts are present in 3.4% of first trimester pregnancies and 20% of those persist into the second trimester
They are usually located close to fetal insertion of the cord and vary between 4–6 mm in diameter.
They are associated with a 20% increase in the prevalence of aneuploidy and structural anomalies
Pseudocysts (Wharton’s jelly cysts) are more frequent than true cysts and tend to be located close to the fetal heart insertion site of the umbilical cord
They are formed by localized edema and the liquefaction of the Wharton’s jelly and have no epithelial lining
These cysts are associated with fetal trisomy and other congenital anomalies, including exomphalos, vertebral defects, imperforate anus and tracheoesophageal fistula
Sonographic assessment shows a cystic mass along the cord without internal flow on color Doppler ultrasound
If another fetal anomaly is seen together with umbilical cord cyst, karyotyping is indicated.
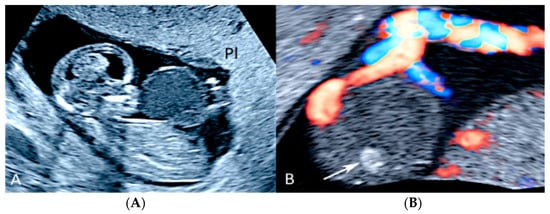
Pregnancy at 12 week’s gestation. Two-dimensional ultrasound: sagittal scan of the fetus showing a cyst filled with finely corpuscular material at the level of the cord insertion on fetal abdomen (A). Color Doppler ultrasound highlights the cord’s splayed vessels due to a hemorrhagic cyst with a clot inside it (arrow) (B). (Legend: Pl: placenta).
Single Umbilical Artery
A single umbilical artery (SUA) has a prevalence of 1.0% of all pregnancies, with greater frequency of an absent left umbilical artery than absent right umbilical artery
Fetuses with isolated SUA have a general favorable in utero prognosis while those with other associated congenital anomalies are at higher risk of chromosomal abnormalities, pregnancy complication, mortality and morbidity in the neonatal period
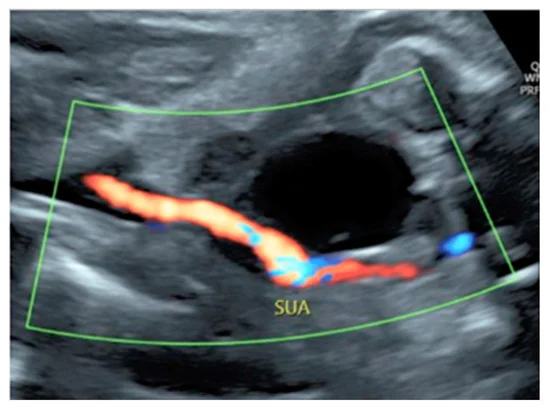
Sonographic diagnosis can be made on an axial view of the umbilical cord, with only two vessels seen on grey-scale, or by visualizing only one artery next to the bladder on the fetal pelvis using color Doppler ultrasound
Single umbilical artery present within the cord
Most common cord abnormality
Can present as a solitary abnormality
Can be associated with:
GU anomalies
CNS anomalies
Omphalocele
Cardiac anomalies
Trisomy 13 and 18
Umbilical Cord Varix
Umbilical cord varix is a rare condition in which there is a focal dilatation larger than 9.0 mm in the intrahepatic or extrahepatic portion of the umbilical vein
It is associated with a 5.8% risk of chromosomal aneuploidy, especially trisomy 21, and a 19% risk of additional ultrasound anomalies
At ultrasound examination, a cystic structure is seen in the fetal abdomen, showing differential diagnosis to normal fetal gallbladder and fetal stomach mesenteric or omental cysts and umbilical artery aneurisms
Doppler ultrasound evaluation is essential for a correct diagnosis
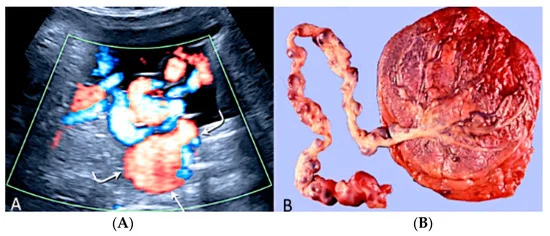
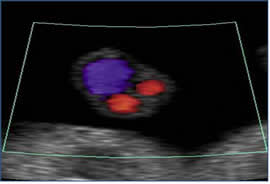
Doppler ultrasound (A) demonstrating an umbilical cord varix (curved arrows) with pathology confirmation after birth
Umbilical Vessel Thrombosis
Risk factors for umbilical vessel thrombosis include the hyper coiling of the umbilical cord and deficient Wharton’s jelly
Umbilical artery thrombosis is a rare event and is associated with intrauterine growth restriction, fetal organ infarcts and stillbirth
Umbilical vein thrombosis is also a rare event and is associated with worse perinatal outcomes when compared to umbilical artery thrombosis, as there is only one vein in the umbilical cord to deliver oxygenated blood from the mother to the fetus
Generally, the diagnosis is made after birth, but sonographic diagnosis is possible by visualizing an echogenic core representing the thrombus, associated with turbulent flow on color Doppler with a dilated umbilical segment, when the vein is not completely occluded, or by not finding two blood flows within the umbilical arteries.
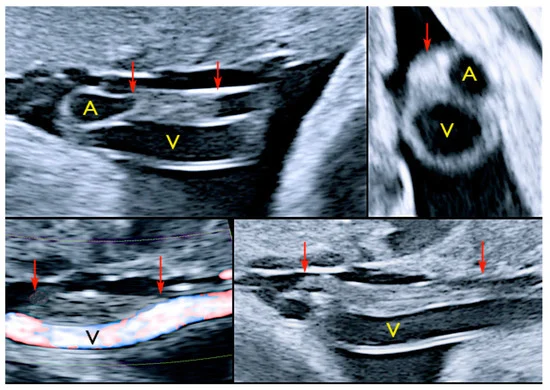
Pregnancy at 32-, 34- and 35-week’s gestation. Two-dimensional ultrasound in longitudinal and axial scan of the umbilical cord. A moderate echogenicity corresponds to segmental thrombosis of an umbilical artery. The thrombosis zone is indicated by red arrows and the progressive extension is further delimited by arrows
Umbilical cord hemangioma
The hemangioma is the most common tumor of the umbilical cord, although it is exceedingly rare.
These masses, unlike allantoic cysts, appear as solid hyperechoic masses and are more often located near the cord insertion site into the placenta.
AMNIOTIC FLUID
1st trimester
Production poorly understood
Multiple sources (maternal: placenta and membranes)
2nd & 3rd trimesters
Fetal urine major contributor, from 16 weeks’ onwards (and lungs)
Assessment of AFV is assessment of fetal well being
Abnormal amniotic fluid volume
Increased – polyhydramnios
Decreased – oligohydramnios
No fluid – anhydramnios
Amniotic fluid appears sonographically as anechoic fluid surrounding the fetus.
Echogenic debris in the amniotic fluid may be vernix or meconium, with meconium being the least likely to be observed during an otherwise normal examination.
Amniotic fluid has several important functions,
protecting the fetus from trauma
temperature regulation
musculoskeletal maturity
normal lung
gastrointestinal development
The fluid that is seen in early gestation is thought to arise from water and various other materials passing freely through the membranes amnion and chorion surrounding the embryo.
In the second half of the pregnancy, the fetal kidneys and lungs produce most of the amniotic fluid, with urine being the greatest contributor
3 methods of assessment
SUBJECTIVE
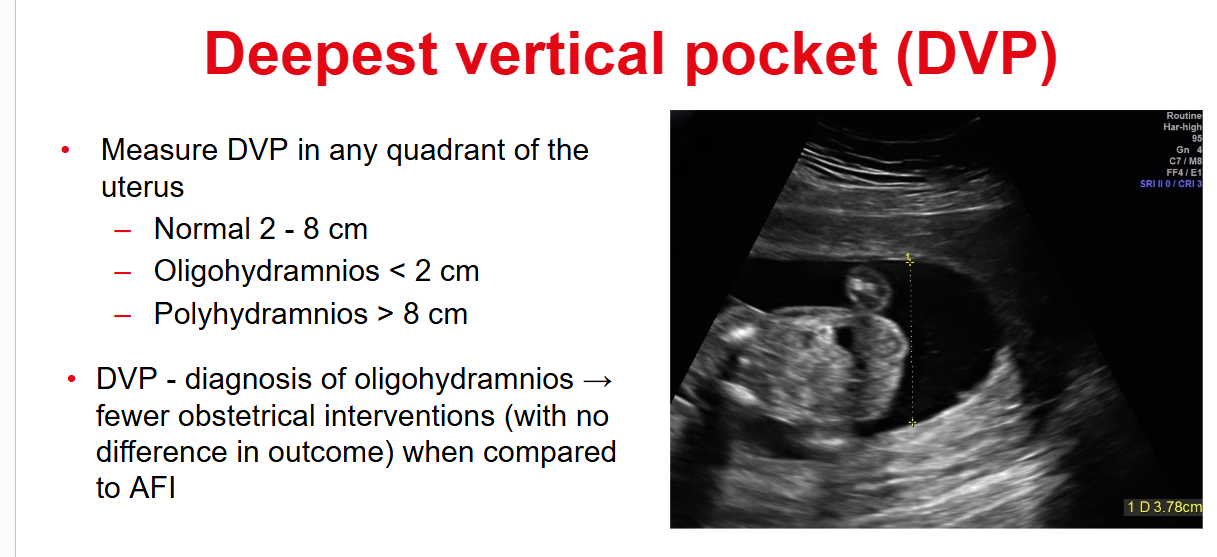
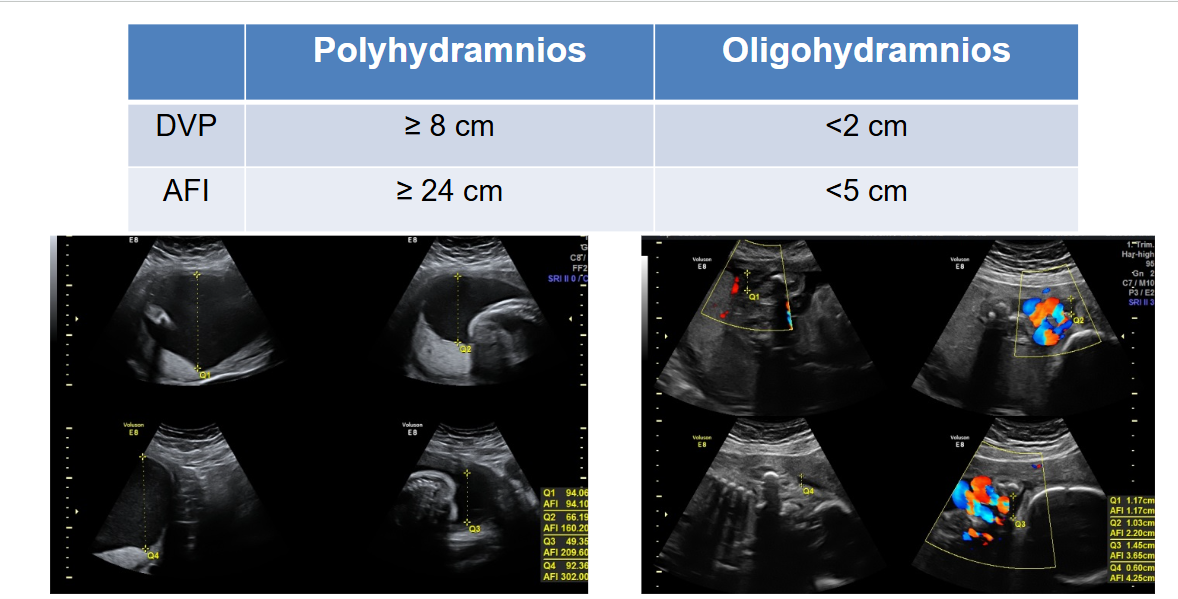
SINGLE DEEPEST VERTICAL POOL- The maximum vertical pocket, also referred to as the deepest vertical pocket, may be used. This pocket should contain no fetal parts or umbilical cord and measure at least 2 cm, with a normal range between 2 and 8 cm.
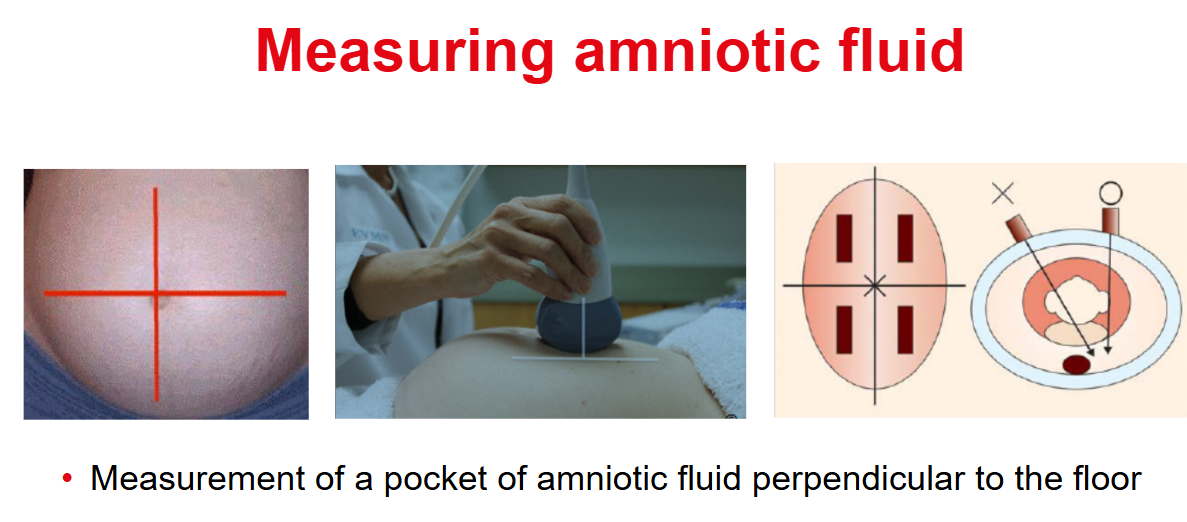
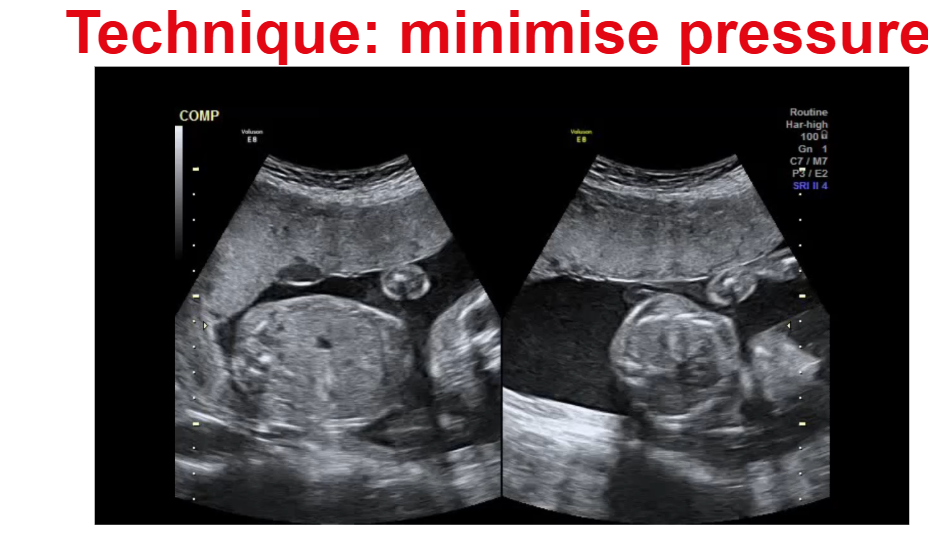
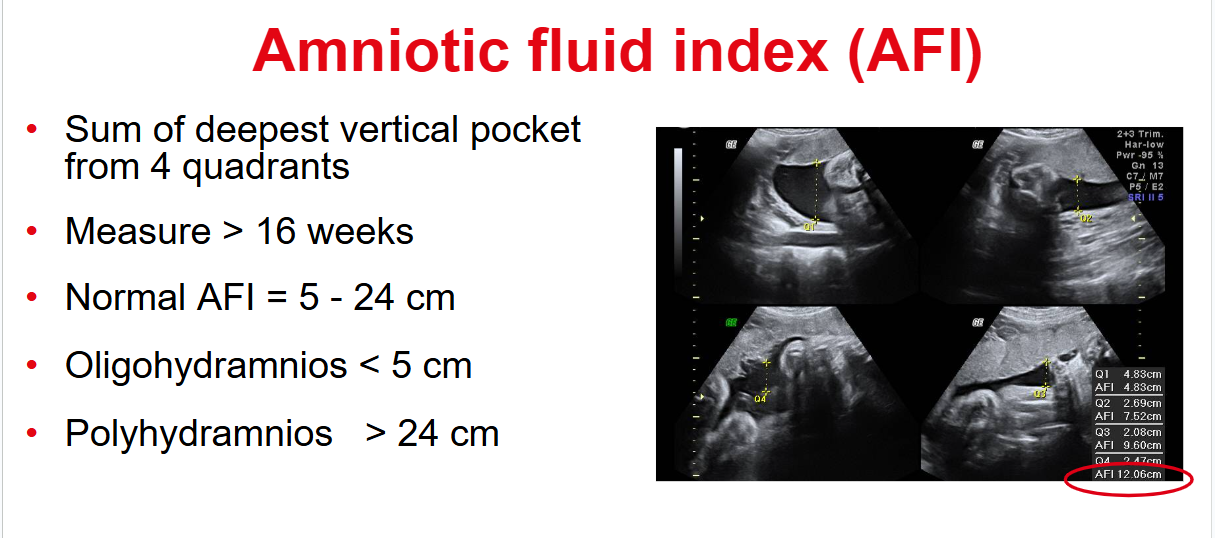
AFI - AMNIOTIC FLUID INDEX -The most widely accepted means of evaluating the volume of amniotic fluid is the amniotic fluid index (AFI). The AFI is measured using the anteroposterior dimensions obtained from the four quadrants of the amniotic sac and adding them together. Once more, these measurements should not include fetal parts or umbilical cord. Color Doppler can be used to ensure that no cord is included. For the measurement, the transducer must be placed perpendicular to the floor. The “normal” amount of fluid varies with gestation. Normal is 5-24 cm.
An excessive amount of amniotic fluid is termed polyhydramnios
Deficient amount is termed oligohydramnios
When an abnormality is noted in the amount of amniotic fluid, a thorough evaluation of the fetal genitourinary system and gastrointestinal system for abnormalities should be conducted, although other systems may be the reason for the imbalance
Because the fetal kidneys produce a significant amount of amniotic fluid, when oligohydramnios is observed, abnormalities of the urinary system should be initially suspected.
Amniotic fluid is also constantly being swallowed by the developing fetus and absorbed by the gastrointestinal tract. Therefore, when polyhydramnios is present, abnormalities of the fetal gastrointestinal system should be primarily suspected.
|