Critical Care
1. Objectives
Develop awareness of what patients endure during insertion, use, and removal of devices.
Recognize patient safety issues related to procedures (including post-transfer to med-surg units).
Provide patient education about expectations.
2. Arterial Line
Indications
Continuous BP monitoring.
Frequent arterial blood sampling.
Thumb - atrial and rest of fingers from the ulnar artery.
Pre-insertion
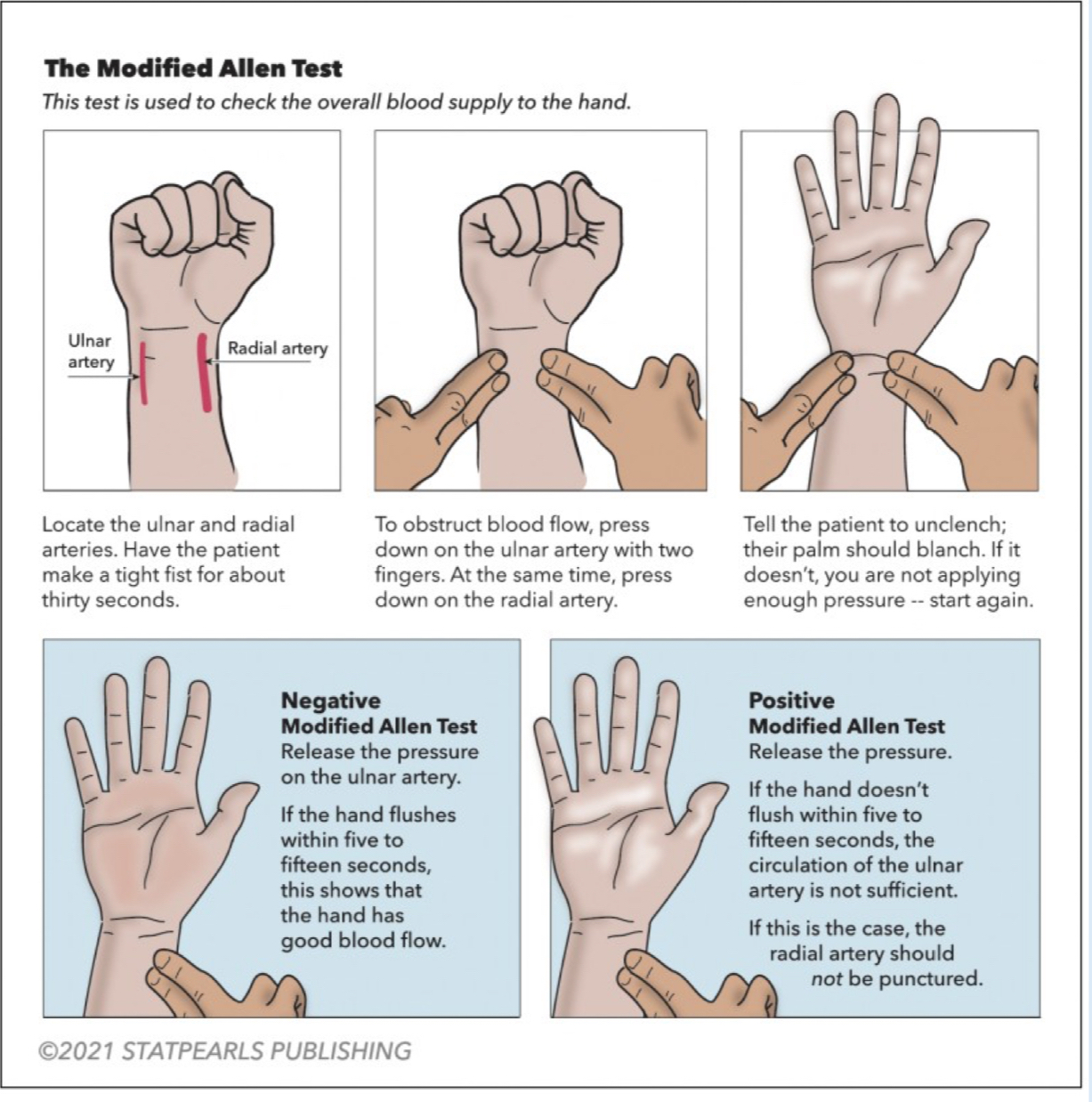
Perform Allen test (radial site).
Positioning
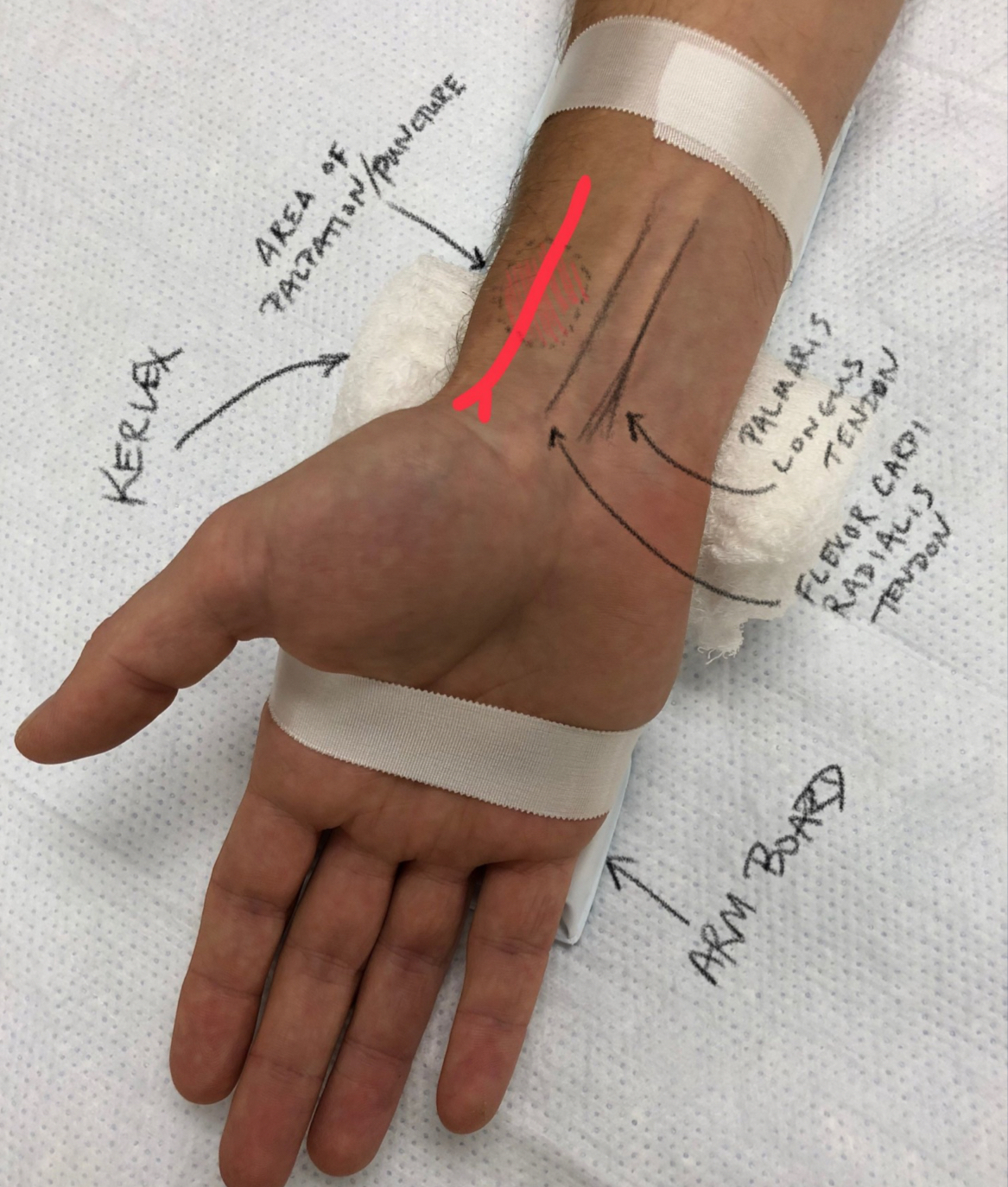
Align 1st thumb metacarpal with radius for easier insertion.
Kerlix/washcloth support.
Post-insertion Assessment
Aspirate blood easily.
Check distal perfusion (fingers or toes).
Monitor insertion site for bleeding/hematoma.
Dressing intact.
Immobilization board (avoid excessive tightness).
Use & Management
Transducer placement.
Flushing with heparinized saline.
NO medications via arterial line.
Routine dressing change q7 days (with Biopatch if no drainage).
Complications
Compromised blood flow → notify provider immediately.
Arterial spasm, poor distal perfusion, thromboembolism.
Hematoma during insertion/removal.
Removal
Slide catheter out, apply firm pressure 5 minutes.
If not hemostatic, repeat another 5 minutes.
Apply pressure dressing for 24 hrs.
3. Central Venous Catheter (CVC)
Indications
Pharmacotherapy, volume resuscitation, nutritional support, pressure monitoring.
Insertion
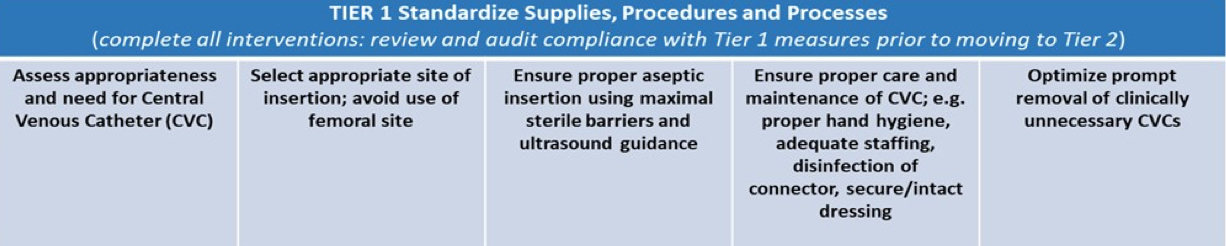
Follows CVC bundle (infection control):
Sedation/pain management.
Seldinger technique used:
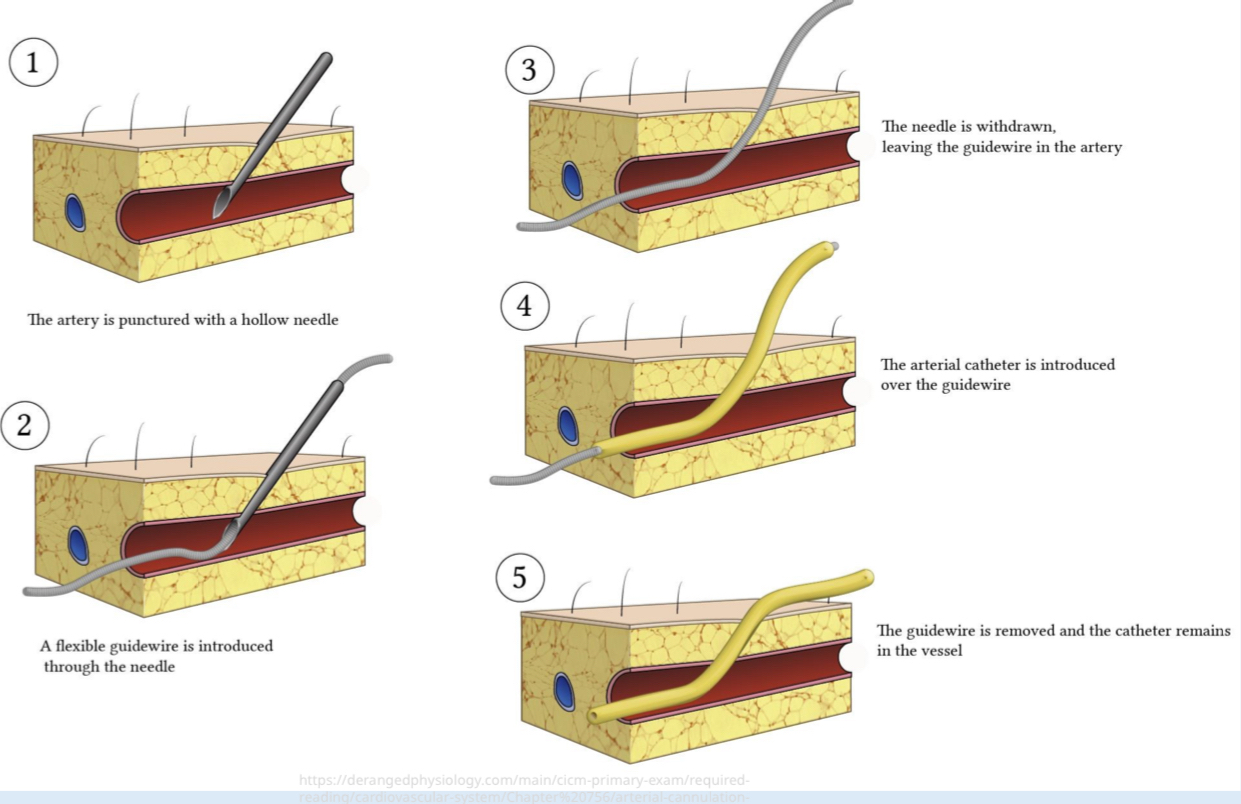
Post-insertion Assessment
Aspirate/flush ports.
Check transducer/waveform if monitoring pressure.
Auscultate breath sounds (subclavian/ IJ risk for pneumothorax, hemothorax).
Back pain = pneumothorax (also superclavical risk of infection)
Use & Management
Dedicated port for TPN.
Ensure blood return from all lumens.
Thrombolytic therapy if no return.
Administer blood products.
Routine flushing (push–pause–push).
Dressing changes weekly/PRN.
Removal
Clean gloves acceptable.
Instruct patient: Valsalva maneuver.
Pull out completely and apply pressure.
4. Intraosseous (IO) Line
Indications
Vascular access when IV inaccessible.
Used in cardiac arrest, trauma.
Insertion
Drill-assisted or manual bone marrow needle.
Locations
Long bones (marrow vasculature doesn’t collapse).
Checking Placement
Aspirate marrow (like CVL).
Contraindications
Local infection, nearby fracture.
Use
Bolus meds (with flush).
Blood products.
IV fluids and drips.
Patients with shock, time is valuable. No time for IV
Adenosine can’t administered. It wouldn’t be as effective.
5. Endotracheal Intubation
Indications
Acute respiratory failure.
Altered LOC.
Airway protection for procedures.
Insertion
Position: supine, “sniffing” position.
Preoxygenation.
Sedation/pain meds/movemen; administration of 2+ meds.
Sellick maneuver.
Monitor VS (oximeter tone).
Equipment check (laryngoscope or fiber optic).
Post-insertion
Assess breath sounds (lungs & stomach).
Confirm placement (ETCO₂, CXR).
Expect transient tachycardia/HTN.
If not resolved, MORE SEDATION/PAIN meds needed
Verify lip depth measurement.
Ventilator settings, ABG after 20–30 min.
Management
Ensure patency & securement.
Sedation/pain management.
“Sedation holiday.”
Helps us know when they are not sedated, what they can do on their own (their strength and how successful they will be without help)
Extubation
Stop NMB, reduce sedation.
Have re-intubation supplies ready.
High Fowler’s, suction airway.
Care team roles:
RT performs extubation.
RN supports patient comfort.
All assess status (WOB, SpO₂, ABG, breath sounds, stridor).
Stridor - vocal cords (coup); inflammation from the tube.
EPINEPHRINE NEBULIZER
Hoarseness is normal, will go away in a couple of days
6. Chest Tubes
Indications
Remove fluid (hemothorax, effusion, empyema).
Remove air (pneumothorax).
Remove both air & fluid.
Types
Trocar
Pigtail
Silastic
Insertion
Requires sedation, local anesthesia, possibly systemic pain management analgesia/anxiolytic.
Sterile technique.
Hat and mask for everyone; sterile gown for providers only
Placement guided by anatomical landmarks.
Post-insertion
Monitor breath sounds, SpO₂, WOB, RR, drainage.
CXR confirmation.
Document drainage characteristics, suction setting, water seal bubbling, dressing status.
Collection Device
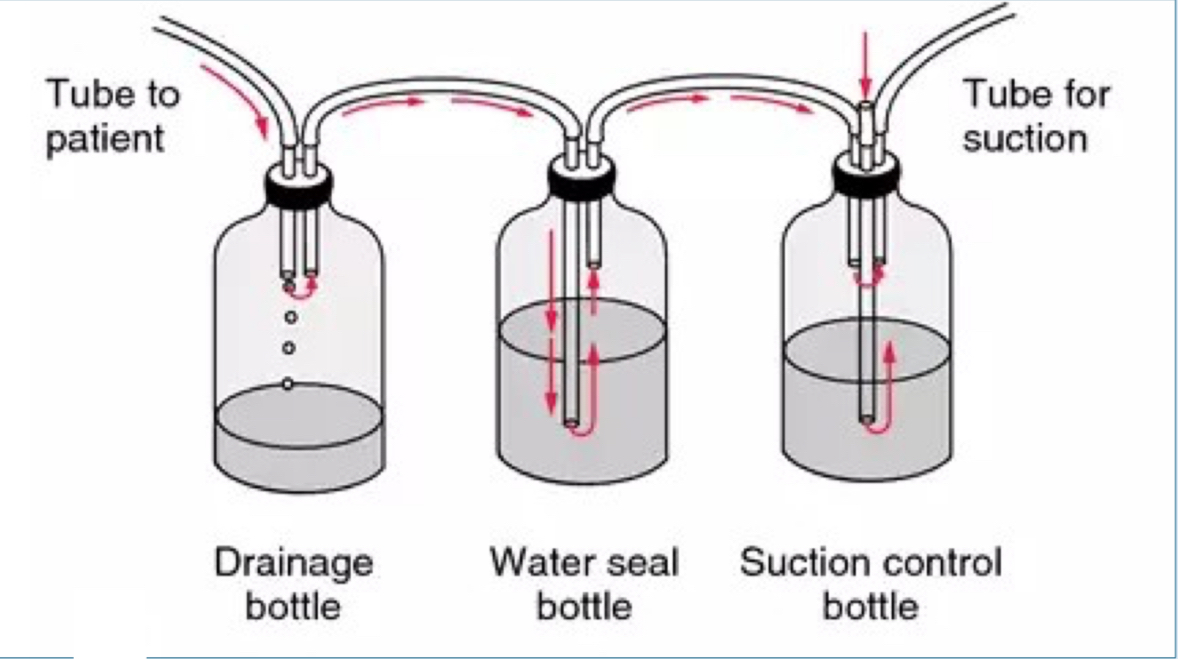
3-chamber system: suction regulator, water seal, drainage.
If its a hemothorax, no bubbling
If its a pneumothorax, yes to bubbling until sealed off
Transport
Can use collection system without suction OR Heimlich valve.
Never clamp chest tube!
7. Dialysis/Pheresis Catheter
Indications
Bedside RRT, plasma exchange.
Insertion
Same as CVC.
Post-insertion
Same assessments as CVC.
Ports clamped & packed with high-concentration heparin.
Use
For RRT or plasmapheresis only.
8. Cardioversion/Defibrillation
Indications
Shockable rhythm with symptoms.
Procedure
Chest pad or esophageal electrode placement.
Sedation/pain control.
Monitoring
Team safety, airway maintenance, patient monitoring.