QUIZ #2 STUDY GUIDE
Module 2, pt. 1: Inflammation and immunity alterations (Ch. 7, 8 and 9)
Video lecture
1st line of defence
- physical and mechanical barriers
- biochemical barriers
- normal microbiome
2nd line of defence
- inflammation
inflammation
- quick, nonspecific, localized most of the time
- goals; in order
- neutralize, limit cause of injury
- clean (phagocytosis)
- heal
response
- injury = vasodialation = release of cytokines (controls other immune cells) = endothelial cell contraction and leukocyte diapedesis (passage of blood cells through capillaries) = allow passage of leukocytes (including macrophages) in to site where injury happened = phagocytosis, removal, neutrolizing = activation of adaptive immunity
inflammatory and immune cells
- neutrophils
- neutralize destroy
- capture and destory invading bacteria or microorganisms by ingesting
- travel through blood stream and will know how to exit through the injury site
- body will react with inflammation
- monocytes
- later become macrophages (eats microorganisms) or dentritic cells (antigen presenting, informs to fight pathogens)when invading a germ or bacteria entered in body
- either kill it or alert other blood cells to help kill it
- experts on phagocytosis
- eosinophils
- allergies
- lymphocytes
- lymphocyte
inflammatory cells in action: neutrophils and macrophages
- cell injury activates tissue macrophages
- produces cytokines
- small proteins that sends a message to endothelial cells to sticky to white blood cells
- neutrophil will bind and migrate towards activated macrophages through chemotaxis
- macrophages to attract neutrophils and they'll know where to go
- between the neutrophils an macrophages, phagocytosis happens
- eat bacteria, in to phagosome
- recognition and attachment
- opsonization
- when phagocytosis is coded by antibodies of compliment proteins that will help macrophages phagocytosis better
- it tags pathogens so neutrophil and macrophages can find them easier
- without opsonization (immunocompromised), phagocytosis will still happen but just inefficently
- without complement proteins (liver disease), less efficient inflammation
- opsonization
the compliment system: helping the inflammatory cells
- compliment produces opsonization
- a bunch of proteins that are all produced by liver
- latent in plasma normally as long as we have healthy liver
- gets activated by bacteria, antibodies, pathogens
- when activated, cascade of activations
- induces chemotaxis, attract neutrophils in injury site
- polymerize, membrane attack complex: polimer of proteins binding to bacteria and opens a hole in the bacteria (destroys it)
chemical mediators of inflammation
- vasodilation
- prostaglandin
- produced during inflammation
- vasodilators
- inhibit with asprin
- histamine
- increases vascular permeability
- anti histamine for allergies induces vasoconstriction
- nitric oxide
- prostaglandin
- pain
- prostaglandin
- activates nociceptors
- aspirin is an analgesic blocks pain similar to inflammation
- prostaglandin
- fever
- systemic effect
- IL-1, IL-6, TNF and prostaglandis are produced
- can escape inflammatory site and in to bloodstream, up to brain stem
- brain stem is where thermoregulation is
- fever is good, other enzymes for metabolism thats not essential will slow down, give time for body to regroup
- wound healing
- relate to production of collagen and new blood vessels
- phagocytosis
- ways to increase
acute inflammatory response
- tissue injury = activation of macrophages = produces cytokines, inflammatory mediators = redness, swelling, pain
- can also activate blood vessels to make sure the cells needed arrive = vasodialators
chronic inflammatory response
- acute inflammation = resolution = termination of inflammation = homeostasis
- ineffective resolution/persistent injury = contiuation of inflammatory process = chronic inflammatory disease
- ex. arthritis, TB, tendinitis
chronic inflammatory response
- neutrophils will keep going = they ask for help from lymphocytes and fibroblasts = lymphocytes will try to isolate the acute inflammation happened = if not resolved, fibroblasts deposits collagen to the inflammatory site, seals it off = can sometimes lead to deformation of scars
phases wound healing
- clotting to stop bleeding
- inflammation to clean up the mess and neutralize (neutrophils, lymphocytes, macrophages)
- inflammation will decrease and heal through proliferation (rapid reproduction of cells)
- angiogenesis: formation of new blood vessels
- fibroblasts: produces collagen
- granulation tissue: the wound rebuilding itself from the bottom up. it also protects the surface from microbial invasion and more injury
- what someone wants to see clinically with wound healing
- remodelling
- epithelium closes again
- when not ideal, scar formation or contracts
wound repair by primary intention
- edges are closely re-approximated, most of the time intentional
- most of the time, minimal scarring
- ex. sutures = fibrin clot = neutrophils will clean up and neutrolize = fibrobalst will start rebuilding from the floor up
wound repair by secondary intention
- when the wound had to be left open rather than being stitched together
- usually leaves a scar
- ex. necrosis = angiogenesis (formation of new capillaries) = macrophages cleans up = formation of granulation tissue (red, full of blood vessels, pushes upwards) = fibroblasts deposits collagen but might not know where to stop producing collagen = might leave a scar/keloid
Adaptive immunity
- lymphoid tissues
- thymus shrinks through puberty
overview of immune response
- two types of immuno response
- cell mediated immunity
- b and t cells formed in thymus
- ready to detect a new antigen and differentiate that can help the immune response by remembering the antigen
- humoral or antibody mediated immunity
- produces in antibodies 5 different types
- produced by plasma cells
- differentiated B cells
- differentiate to plasma cells
- when exposed to antigen = B cells will look at the antigen and develop to plasma cells = plasma cells will produce antibodies specific to that antigen
- cell mediated immunity
humoral immunity response
- antibodies
- IgG and IgM are most common, look for it in the blood
- exposure to vaccine = body is not use to it = immune system develops IgG and IgM so body will be prepared for REAL exposure
- primary response: when we get vaccinated
- secondary response: being exposed to the real thing. its faster
- IgG is big, IgM is small = can cross the placenta, passive immunity to fetus in utero
- IgA
- found in membranes in many epithelium
- ex. crying, mucus, saliva, human milk
- this is another way to give passive immunity to baby
- IgE
- allergies
functions of antibodies
- why is it good?
- neutrolizes viruses
- neutrolizes toxins (even bacterial) ex. tetanus
- complement mediated killing activated by antibodies (immune complex)
- phagocytosis
cellular immunity
- cytotoxic T cells
- can kill cells
- ex. cancer cells, transplants
- helped by T helper (Th1)cells. motivates other cells, orchastrating alot of the immune system
- poroduces cytokines to make cytotoxic T cell be more efficient
Hypersensitivity
- anltered immonologic response to an antigen that results in disease or damage to the individual
- four types
1. IgE-mediated type 1
- allergies, anaphylaxis, athsma
- antigen detected by dendritic cells (antigen presenting cells) = presents itself to T helper cells = it stimulates formation og IgE antibodies, these antibodies bind to IgE receptors that are on top of mast cells (mast cells produce vasoactive mediators like histamine) = mucose secretion, smooth muscle spasm
- histamine blockers = no reaction
2. tissue specific type 2
- when specific cell gets targeted
- blood transfusion reactions, hymolytic disease of new borns
- wrong blood cells received = Igm and IgG will recognize its foreign = binds to it and activates the compliment = polymerizes and membrane attack complex (opens a hole in to the cell, osmoticlysis, destroying it)
3. Immune complexes mediated type 3
- immune complexes
- systemic lupus etithematosus, rheumatic fever, rheumatoid arthritis
- vascular plasma had immune complexes floating around = gets stuck in an organ by the organ trying to remove them = compliment will be activated = C5A will attract neutrophils = compliment activation inflammation
4. cell mediated type 4
- mediatedby the cytotoxic t cells, meant to kill other cells
- t cells get close to target cell = bind to it = produces perforin, opens the cell with a hole
- important with organ transplant
- not compatible organ = immune system develop cytotoxic t cells = destroys the organ
- transplant receivers need to me immunosuppressed
Module 2, pt. 2: AIDS
Immune deficiency: failure of immune or inflammatory response
- increased susceptibility to infections
- primary: genetic defect
- secondary: caused by another condition
opportunistic infections
- caused by non-pathogenic microorganisms, become pathogenic with immuno deficit human
- recurrent
- clinically atypical
primary immune deficiency
- rare, congenital
- ex. combined and antibody deficiency, immune dysregulation, phagocyte and innate immunity defects etc.
secondary immune deficiencies
- common, acquired
- ex. pregnancy, againg, psychological stress, trauma, dietary insufficiencies etc.,
HIV
- HIV: human immunodeficiency virus
- attacks bodys immune system, can lead to AIDS when not treated
- destroys CD4 T cells
- important molecules
- RNA, reverse transcriptase (gives it pathogenicity, replicates in body), proteins (gp 120, gp41)
- life cycle
- attaches to cells (proteins important) = lock to cell is protein CD4 = reverse transcription = integration of provirous (generic material of a virus) into host genome (haploid sets of chromosomes in microorganism) = synthesis of HIV proteins = assembly of virion core
- T helper CD4 positive cells as main HIV target
- perosn with HIV has less T helper cells = immunodeficient
- pathogenesis of HIV
- HIV infects dentritic cells and Th in lymph nodes = burst of viremia (pressence of virus in blood) = infected Th cells circulate the blood = cytotoxic kill infected Th in circulation and in the gut = Th cells in get are also infected = reactivation of HIV replicaiton = HIV viral toxicity destroys bone marrow precursor cells = HIV infects memory cells (latency)
- clinical progression of HIV
- 1-6 weeks, plasma viremia rises
- viral replication neutralizes, latent (delay)
- clinical goal is to keep someone latent, delay replication as much as possible
- replication starts again when symptoms of AIDS begin
- CD4 contiues to decrease
- how to know if HIV positive
- looking for antibodies as they appear later and become stable
- viruses aren’t present in latency so you cant find it
- antibodies dont develop immediately
AIDS: Acquired immunodeficiency syndrome
- caused by HIV, late stage of the infection
- when CD4 is sevearly depleated
- clinical manifestation
- 9000/mm3 WBC count (normal is 4000-11000)
- opportunistic infections
- protoza, fungi, bacteria, viruses
- cancer
- kaposi sarcoma (most common)
- brain lymphoma
- cervical cancer
- fever means immune system is not severely altered since theres a response
Module 2, pt. 3: Infection
examples of emerging infections
- COVID from SARS-CoV-2
- “MAD COW” from prion
infection: key terms concepts
- pathogenicity: ability of an agent to produce disease by causing harm
- opportunism: benign microorganisms becomes pathogenic because of decreased human resistance
- virulence: capacity of a pathogen to cause severe disease
- ex. ebola, cause death very fast
- agent-host: microorganisms pathogenicity combines with hose defence mechanism
- combine with host defence mechanism
- ex. covid after being vaccinated can cause mild disease since human defence mechanism is strong
- zoonosis: infections harbored in animals and spread to humans
- ex. rabies
clinical stages of infection
- incubation period: between exposure to onset of symptoms
- virus has entered but no symptoms yet
- prodomal stage: non specific infectious symptoms
- invation period: specific signs and symptoms
- person can feel weak and fever then develop a more severe and specific
- convalescence: resolution and recovery
- immune and inflam. sys. succeed
pathogenesis of fever and acute phase response
- infection = fever first symptoms
- pyrogen turns up temperature of the body, to the hypothalamus
- TNF, IL1, IL6, IFN, PGE2
- elevating temp. cause febrile response
- slows downbody so gives body enough time and activate other things for the recovery will be faster
- c reactive protein (CRP) is used as indicator that acute phase response is on
- non specific
process of an infection
- colonization
- contact and entry
- invasion
- invade or evade
- multiplication
- once they invade, they grow
- viral replication
- dissemination
- when it speads
biofilm
- bacteria can stay and hide and grow and disseminate in other areas
- mucus basically houses bacteria
- encourages recurrent infections
- ex. bronchial disease
classes of infectious microorganisms
- bacterial infections
- no nucleus but nucletic acid
- shape is cocci (round), bacilli (elongated), spirochetes (spiral)
- gram positive vs gram negative
- depending on cell wall
- lipopolysaccharides LPS: lipids with alot of sugar residues
- present in outer membranes of gram negative bacteria
- very toxic
- activated macrophages easily
- endotoxins, not released when bacteria is alive but when theyre dead
- bacteria can grow aerobic or anaerobic
- anaerobic are more aggressive
- bacteriaemia
- bacteria in blood
- septicemia
- when bacteria causes infection’
- some bacterias can resist phagocytosis
- can remain latent
stains
- gram positive is purple
- gram negative is pink
staphylococcus aurerus
- gram positive bacteria, non pathogenic but sometimes, it can become pathogenic
- depending on where it is and how affected the skin is, can cause different diseases
- produces exotoxins
- its on the skin latent (nonpathogenic). when theres a wound, it can go in (pathogenic)
- the same bacteria either cause different diseases depending on where it is, resistance of host and if it produces exotixins or not
effects of pathogenicity by endotoxins from gram negative
- they have LPS in outer membrane of cell wall
- LPS activates macrophages, produces activation of cytokines
- depending on quantity
- low: cause local inflammation
- moderate: fever
- high: activate macrophages everywhere at the same time = inflammatory response everywhere (lungs, all blood vessels) = septic shock
fungal infections
- “mycoses”
- superficial
- nonpathogenic, nonaggressive microorganisms
- frequently opportunistic
- 2 types
- molds
- yeats: single cells
candidiasis
- superficial mycoses
- doesnt cause disease
- but immunosuppressent can cause mucosal infections
- can be trated with anti micotic
parasitic infections
- protoza (uni cellular) vs helminths (multicellular)
- hosts: person that will develop the disease
- vector: one who houses the host
- life cycle: toxoplasmosis
malaria: parasitic disease
- affects red blood cells
- vector is mosquito
- neutralize mosquito
viral infections
- obligatory intracellular microorganisms (really small)
- tissue specific
- cause disease by getting in to the cell
- respiratiry virus can get in to the airways
- hepatitis can get in to liver cells
- herpes virus can get in to neurons
- HIV can get in to T cells
- RNA or DNA and
- (the one who hold the “key” to get in to specific cells)
stages of viral entrance during infection of cell
- come with capsid with the fusion proteins (keys) = receptor mediated endocytosis = uncoats capsid = it goes in to nucleic acid = replicate and use the synthetic machinery of the cell to asssemble the virus = synthesize viral proteins = form new particles = the new particles and exit and the cycle continues
antigenic shifts in influenza virus
- viruses have a way to mutate that causes antigenic shifts
- viruses will have slightly altered genes and antigens, because of this they shift alot
- different variants for covid
- can be detected every year
Module 2, pt. 4: Coronoavirus
SARS: severe acute respiratory syndrome
MERS: middle east respiratory syndrome
CODIC-19: coronavirus disease 2019
Covid pathophysiology
- block spike from binding to ace2
- spike protein becomes most important because it is the protein that allows virus to get in to cells but also for immunity
- Mrna teaches cells to produce spike proteins and create antibodies
- worried about variants that change the spike protein = vaccinated people are no longer immune
- ill continue this later im too lazy rn
Module 2, pt. 5: stress and disease
stress response key terms
stressors
- physiologic and psychogenic
- general adaptation syndrome (GAS)
- allows adaption to stressors, non specific
- ex of signs: tachycardia, more alert
- acute vs chronic
- GAS stages
- alarm
- resistance or adaptation
- most common
- exhaustion
general adaptation syndrome
- alarm phase
- when body senses the stressor
- generates flight or fight response
- resistance phase
- stress remains, body adaps
- remains on guard
- recovery phase
- stress is removed
- body functions return to normal
- homeostasis
- exhaustion phase
- stress continues
- bodys resources to the combat is depleted
- immune sys. compramaised
- stress related illness can occur
good side of the stress spectrum
- spike in good/short term stress
- turns to bad stress when long term (chronic)
- lifestyle factors
- psychosocial buffers
- activities
- goal
- optimize good stress
- maximize resting zone
- minimize bad stress
- results
- productive immunity
- increase physical performance
- increases health
allostasis: process of achieving homeostasis
- chronic social and envi. stress
- physiological stressors
- major life events and trauma
- depends ofn differences in vulnerability and behavioural response: adaptive or maladaptive
- result of this is achieving allostasis
diversity of responses to stress
- repeating stressor builds endurance
- repeating stressor can also lead to less adaptation
- stress might also get prolonged
- inadequate response
physiology of the acute stress response
- alarm reaction
- neural (fast)
- sympathetic response/fight or flight response
- centered in brain stem
- fight or flight response facilitated by the connection of the brain step to the adrenal medulla = release catecholamines, epinephrine and norepinephrine = generates response
- hormonal (slow)
- pituitary gland
- hypothalamus = releases CRH (corticol releasing hormone) = anterior pituitary gland produces ACTH (adrenocorticotropic hormone) = this will go to the adrenal cortex = adrenal cortex will produce cortisol (glucocorticoids)
- we need the slow one because corticoids morbilizes glucose
- fight or flight response needs glucose
- neural (fast)
sympathetic nervous system response
- sympathetic activation (vasomotor tone) = adrenal medulla activation = increased strength
- sympathetic activation (vasomotor tone) = contraction of arteriolar smooth muscle = vasoconstriction = increased peripheral resistance = increased blood pressure
hormonal structures involved in response to stressors
- slower but more regulated, always have a feedback loop
- (explained above)
cortisol response
- metabolic response
- more cortisol, more mobilization of glucose = increased energy
- increased glucocegenesis, glycogenolysis, proteolysis, lipolysis
- cardiovascular effects
- increased myocardial contractility, cardiac output, bp
drug role of adrenal gland in the stress response
- adrenal is involved in both hormonal and neural
- medulla produces epinephrine that will increase HR and produce fight or flight response
- adrenal cortex is also stimulated to release more glucose and produce mor cortisol
- some conditions where adrenal gland is damaged meaning theres no stress results
- neurological condition where brain stem is damaged, no stress results
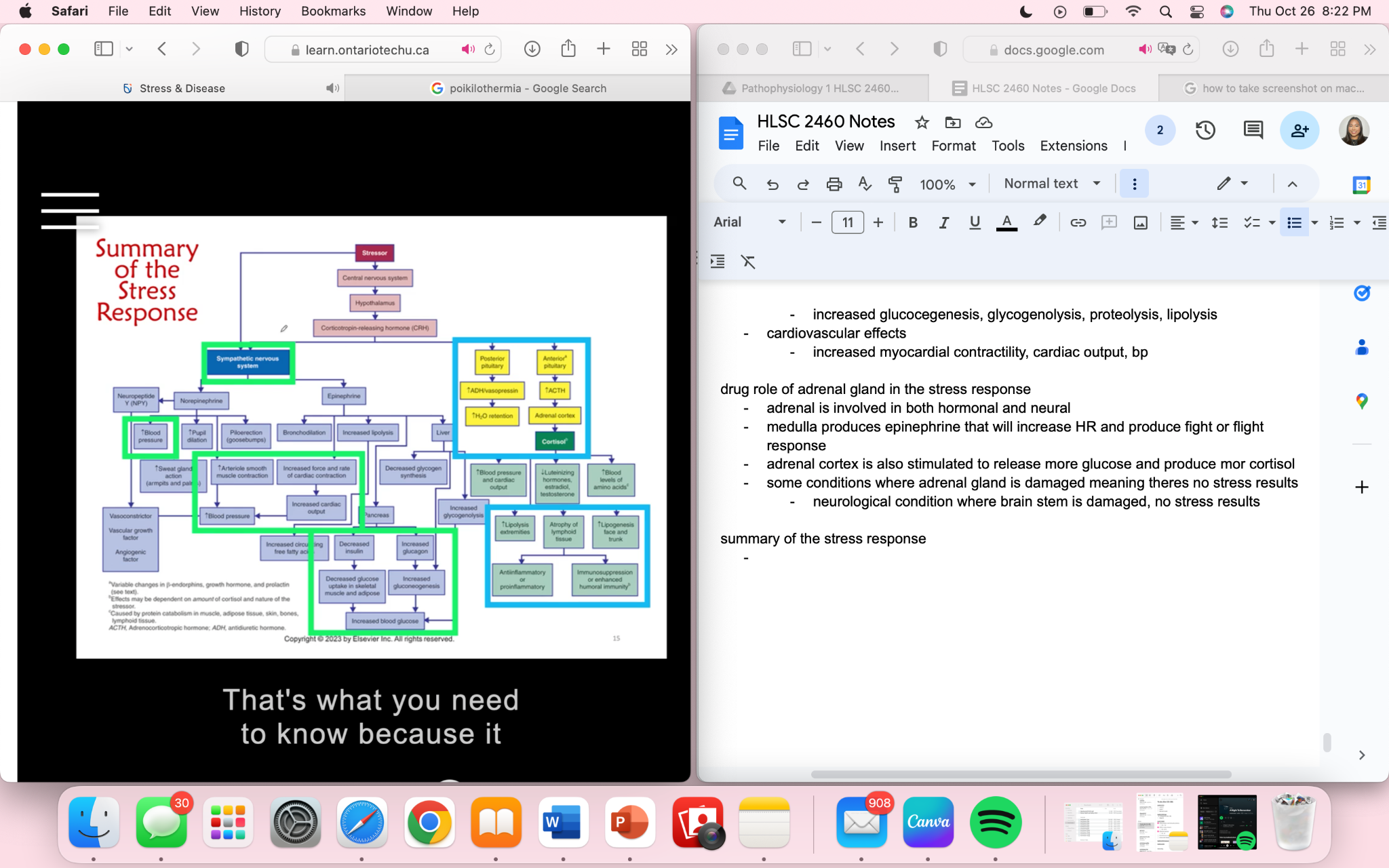
summary of the stress response