lecture 7: digestive system
Biomedicine: Human Sciences
Lecture 7: Digestive System Part One
1
© CNM: Human Sciences – Digestive System I. BQ / MC.
Learning Outcomes
In today’s topic you will learn:
About the structure and functions of the digestive system.
The key enzymes and hormones involved in digestion.
The types of dietary carbohydrates, fats / oils and proteins.
You are what you digest You are what you absorb
You are what you don’t excrete
Digestive System Components:
Components:
Mouth.
Pharynx.
Oesophagus.
Stomach.
Small intestine.
Large intestine (incl. rectum and anal canal).
Accessory organs:
Salivary glands.
Pancreas.
Liver.
Gall bladder and biliary tract.
Digestion Processes
Ingestion: | Oral intake of substances (into mouth). |
Secretion | Digestive juices — water, acid, emulsifiers, buffers and enzymes (saliva, gastric juices, pancreatic juices). |
Mixing and propulsion: | Contraction / relaxation in walls help mix and propel food through the GI tract. |
Digestion: | Mechanical and chemical processes break down ingested food and liquids into absorbable substances. |
Absorption: | Substances passing through walls in the alimentary canal into blood and lymph. |
Elimination: | Excretion of waste and indigestible materials. |
Gastrointestinal Tract (GIT) Layers
The entire GIT contains the same basic four-layer arrangement of tissues:
Mucosa
Submucosa
Muscularis
Serosa (peritoneum)
Mucosa: 1) Epithelium
The mouth, pharynx, oesophagus and anus contain epithelium for protection.
Stomach and intestines: columnar epithelium with:
Microvilli — ↑ surface area for absorption.
Goblet cells — secretion of mucus to lubricate food and protect against digestive juice erosion.
Enteroendocrine cells — specialised endocrine cells that secrete hormones (e.g. CCK) into blood.
Epithelial cells
renew every 5–
7 days
Mucosa: 2) Lamina Propria
The lamina propria consists of connective tissue containing many blood and lymphatic vessels that allow the absorption of nutrients.
The lamina propria contains MALT (mucosa- associated lymphoid tissue). This is a collection of immune cells (e.g., lymphocytes, macrophages, etc.).
MALT is found in many places in the body. In the GIT, we call this GALT (gut- associated lymphoid tissue).
MALT is especially prevalent in the tonsils, oesophagus, small intestine, appendix and large intestine.
GALT:
(Gut-Associated Lymphoid Tissue)
Mucosa: 3) Muscularis Mucosa
The muscularis mucosa is a very thin layer of smooth muscle.
This layer of muscle creates the villi (small folds) which increases the surface area for absorption and digestion.
Movement of this ensures that all absorptive cells are fully exposed to the GIT contents.
The submucosa is a connective tissue layer that lies between the mucosa and muscularis.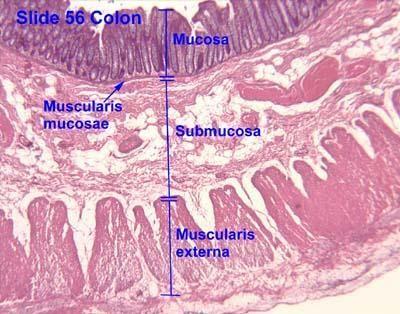
Contains blood and lymph vessels which receive absorbed food molecules.
Contains network of neurons called the submucosal plexus (brain of the gu’).
May contain glands and lymphatic tissue; e.g. Peyer’s patche’ in ileum.
The mouth, pharynx, upper oesophagus and anal sphincter contain skeletal muscle to allow voluntary swallowing and defecation.
The rest of the GIT is mostly smooth muscle, involuntary (autonomic). Contains two layers:
Inner circular muscle.
Outer longitudinal.
Involuntary smooth muscle contractions aids:
Mixing of food with digestive juices.
Propelling food (chyme / bolus) along the digestive tract (peristalsis).
Between the two muscle layers are neurons — myenteric plexus.
GIT Layers Summary:
Peritoneum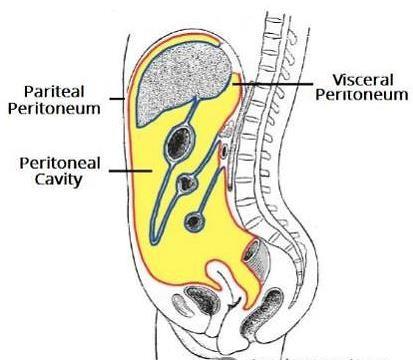

The peritoneum is the largest serous membrane in the body.
The peritoneum weaves between digestive organs and is supplied with many blood and lymph vessels. It provides a physical barrier to local spread of infection.
Consists of two layers:
Parietal — covers the wall of the abdomen and pelvic cavity.
Visceral — covers the organs.
The peritoneal cavity is the space between the two layers and contains a lubricating serous fluid.
Peritoneal Pathologies
Ascites |
| |
Peritonitis periton- = peritoneum -itis = inflammation |
|
The largest fold of the peritoneum.
Drapes over transverse colon and small intestine like an apron.
It’s a double sheet that folds back on itself (hence four layers).
Stores fat: Contains adipose tissue which can greatly expand with weight gain — the beer belly.
Has many lymph nodes containing macrophages and plasma cells (which produce antibodies) to combat infections of the GIT.
The lesser omentum is a peritoneal fold that suspends the stomach and duodenum from the liver.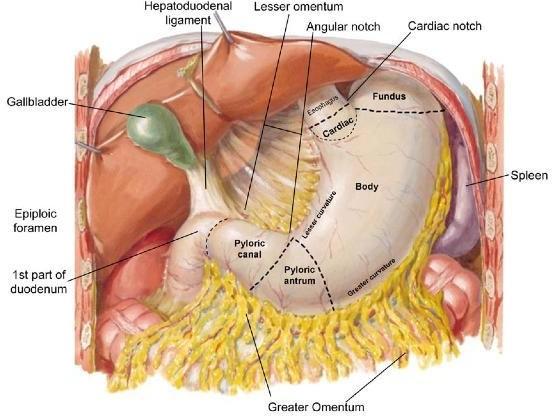
Pathway for blood vessels entering the liver.
The lesser omentum contains the hepatic portal vein, common hepatic artery, common bile duct and lymph nodes.
Enteric Nervous System
The enteric nervous system is the brain of the gut and extends from the oesophagus to the anus.
Contains 100 million neurons (more than the spinal cord).
Functions independently but regulated by the autonomic nervous system:
Parasympathetic (rest and digest) | Sympathetic (fight or flight) i.e. stress |
Increases muscular activity (peristalsis 🡪 myenteric plexus) | Decreases muscular activity (peristalsis 🡪 myenteric plexus) |
Increases glandular secretion (submucosal plexus) | Decreases glandular secretion (submucosal plexus) |
Arranged in two plexuses (networks):
Myenteric plexus:
This contains a network of sympathetic and parasympathetic nerve fibres between the circular and longitudinal muscles of the muscularis.
Controls strength and frequency of muscle contraction: gut motility.
Submucosal plexus:
Network of sympathetic and parasympathetic nerve fibres within the submucosa — controls digestive secretions and detects sensory information.
 Enteric Nervous System
Enteric Nervous System
Types of neurons:
Motor neurons (outgoing / action signal) in the myenteric plexus control peristalsis and in the submucosal plexus control secretions.
Sensory neurons (incoming signal) receive information about the mucosal environment: chemoreceptors and stretch receptors.
Interneurons connect the two plexuses.
The GIT is supplied with arterial blood from branches of the abdominal aorta, which include the mesenteric arteries.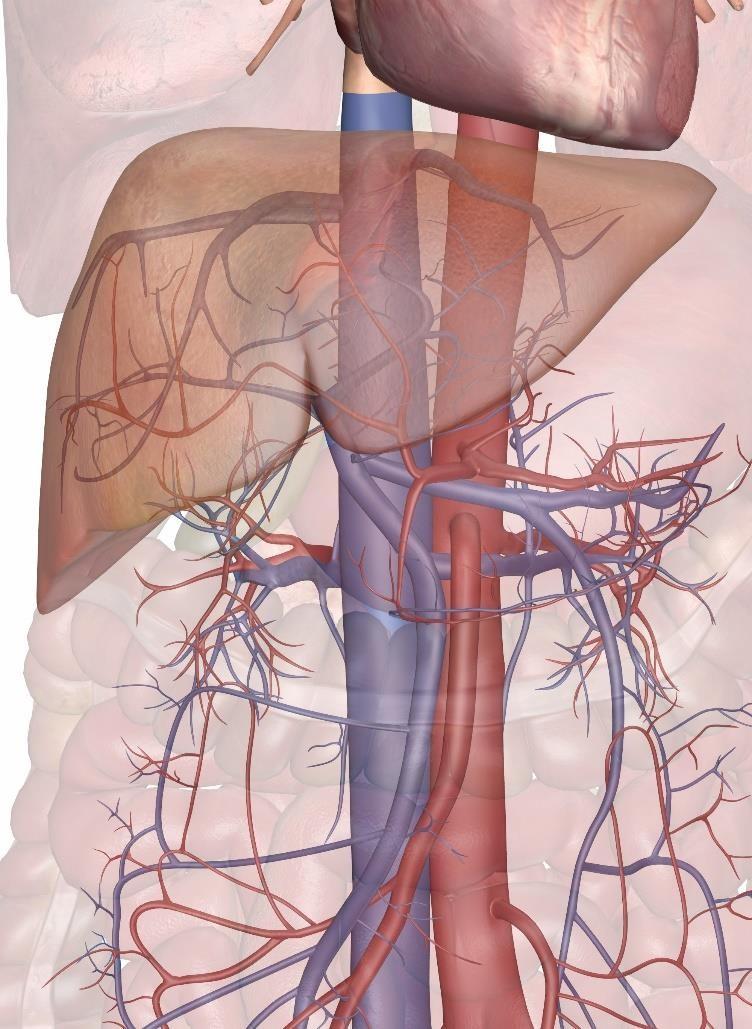
Nutrient-rich blood in the intestines is returned by veins via the liver (portal system) or directly from iliac veins.
The liver filters the blood and processes nutrients which then enter systemic circulation.
The portal vein drains the lower oesophagus, stomach, pancreas, small and large intestine, upper rectum and spleen.
The iliac veins drain the lower part of the rectum and anal canal.
You do not need to know the names of all blood vessels indicated in these images.
Name the FOUR basic layers of the GIT.
Where are the two nerve plexuses located?
What are the two layers of the peritoneum called? What resides between these layers?
Explain what is meant by ascites.
What is the function of the greater omentum?
What percentage of the immune system is located in the GIT?
What vein drains the intestines? Where does this blood vessel go?
What is meant by GALT?
Explain what is meant by peristalsis.
Explain what is meant by enteric.
Inner surfaces are lined with mucous membranes.
Hard palate — bony partition between oral and nasal cavities. Allows simultaneous chewing and breathing.
Soft palate — an arch of muscle.
Uvula — swings up and blocks the nasopharynx preventing food from entering the nasal cavity.
Tongue — voluntary skeletal muscle structure attached to the hyoid bone and mandible. The superior surface is covered with papillae, which contain taste buds.
Adults have 32 teeth (20 temporary).
Teeth have a crown, neck and root.
Dentin makes up the bulk of a tooth internally. Teeth are covered externally by enamel (the hardest tissue in the body).
Sit within the gum (gingiva) and periodontal membrane (a ligament that fixes to bone / connects teeth).
Function in mastication
(what chewing does not accomplish mechanically must be completed by the digestive tract chemically).
Saliva is produced by the parotid glands, submandibular glands and sublingual glands via a reflex controlled by the autonomic nervous system.
Parasympathetic NS stimulates continuous salivation (1–1.5L/day) which provides lubrication.
Saliva is swallowed and lubricates the oesophagus before eventually being reabsorbed.
During dehydration, salivation is stopped, which contributes to the sensation of thirst.
Sympathetic nervous stimulation (stress response) reduces salivation causing dryness of the mouth.
Touch, taste, smell, sight, sound can stimulate digestive salivation.
Water (99.5%).
Mineral salts (Na, K, Ca, Cl, bicarbonate, P).
Enzymes: Salivary amylase (parotid), lingual lipase, lysozymes (found in many body secretions, break down bacterial cell walls).
Mucus.
Immunoglobulins (IgA).
Blood clotting factors.
pH 6.35–6.85 (mildly acidic).
© CNM: Human Sciences – Digestive System I. BQ / MC. 28
Digestion — chemical breakdown of polysaccharides.
Lubricating and dissolving food.
Cleansing of oral cavity and teeth.
Defence — non-specific (IgA and lysozymes).
Taste.
Buffer — for acidic foods.
Waste removal — urea / uric acid from the body.
Oesophagus
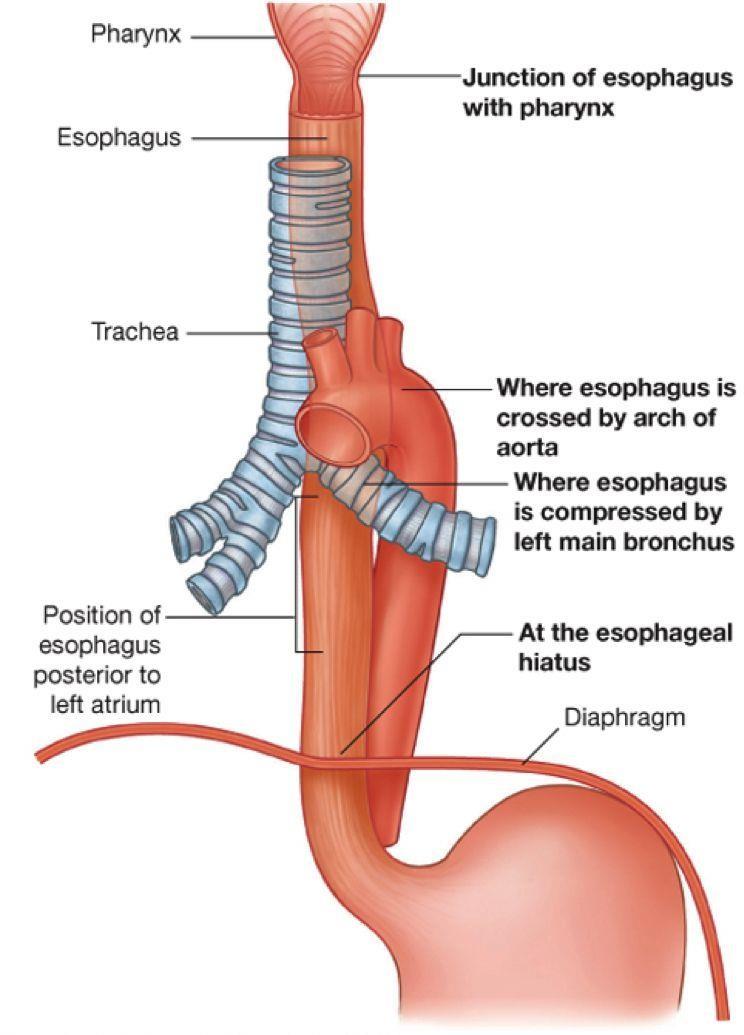
A 25cm long muscular tube, attached to the larynx. Posterior to trachea, passes through the diaphragm (T10).
Lined with epithelium, lubricated with mucus.
The superior / middle oesophagus contains skeletal muscle and the lower contains smooth.
Food travels to the stomach via muscular contractions (peristalsis).
Epiglottis — a flap of elastic cartilage which prevents food entering the trachea.
The lower oesophageal sphincter acts as a seal on the stomach to prevent reflux of stomach contents into the oesophagus.
The stomach is a J-shaped organ with four main regions: cardia, fundus, body,
pyloric with lesser and greater curvatures.
Same layers as the rest of the GIT, but with three layers of muscle (rather than two) churning and mixing food with gastric juice.
Two sphincters: cardiac and pyloric.
Neural feedback: (enteric nervous system)
Food distends the stomach stimulating stretch receptors in its walls.
Chemoreceptors monitor pH changes.
Activate submucosal plexus causing waves of peristalsis and gastric juice flow.
The stomach secretes 2–3L of highly acidic (pH 2–3) gastric juice and mucus a day.
The mucus produced by goblet cells in the stomach provides a barrier against the acidity present within the stomach.
The stomach contains simple columnar epithelial cells. These have a fast turnover (replacing the lining every three days).
These contain three types of exocrine cells:
Substances secreted | Functions | |
Parietal cells | Intrinsic factor (IF). |
|
Hydrochloric acid (HCl). Secretes H+ and Cl- separately; combining in the stomach. |
| |
Chief cells | Pepsinogen. Gastric lipase. |
|
Goblet cells | Mucus. |
|
Functions:
Mixing chamber — churns up food.
Holding reservoir — storage.
Defence — non-specific defence from gastric acidity.
Absorption (limited) — water, alcohol, drugs, i.e. aspirin.
Digestion — mechanical but also chemical digestion of proteins and lipids.
Iron — made more soluble with stomach acid.
Satiation — tells you to stop eating.
Hormones:
Ghrelin — stimulates hunger.
Gastrin (produced by G cells) — responds to stomach distension. Stimulates gastric juice secretion and gastric motility.
Accessory structure:
Pancreas

The pancreas is an accessory digestive organ of the digestive system that has both exocrine and endocrine functions.
Exocrine Function | Endocrine Function |
|
|
|
|
Pancreatic Enzymes
Pancreatic enzymes are imperative for digestion.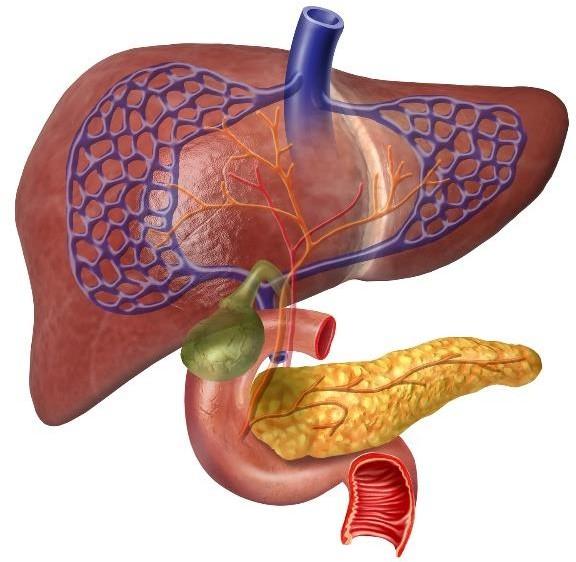

Pancreatic enzymes are secreted by the pancreas into the lumen of the duodenum. Proteases are secreted in their inactive form.
Pancreatic Enzyme: | Function: |
Pancreatic amylase | Breaks down starches into sugars |
Pancreatic lipase | Lipid / fat digestion. |
Trypsin | Protein digestion |
Chymotrypsin | Protein digestion |
Ribonuclease | Digest RNA |
Deoxyribonuclease | Digest DNA |
Pancreas
The pancreas is approximately 15cm long and retroperitoneal. It is connected to the duodenum via the pancreatic duct.
Accessory structure:
Gallbladder
The gallbladder is a pear-shaped sac in the liver, measuring 7–10 cm in length.
Bile ducts project from the gallbladder and liver, meeting at the common bile duct.
Bile ducts collect bile produced by hepatocytes which pools in the gallbladder.
Bile enters the small intestine via the common bile duct.
When the individual has ingested fat, the gall bladder contracts to eject bile down the common bile duct and into the duodenum.
Gallbladder
The gallbladder ejects bile, which is an agent that emulsifies fats.
Emulsification breaks the lipids into smaller molecules. This increases the surface area for lipid enzymes (lipase) to work.
Bile is composed of bile salts, cholesterol and bilirubin.
pH 7.6–8.6 (mildly basic).
90–95% of bile is absorbed and transported back to the liver from the ileum: Enterohepatic circulation.
Small Intestine
After food combines with stomach secretions, the resulting chyme is pushed through the pyloric sphincter into the small intestine.
Most digestion and absorption occurs in the small intestine.
A long structure (6.5 m) with villi to maximise surface area.
Contains a variety of cells; e.g. goblet (mucous), endocrine, absorptive.
Three regions:
Duodenum — emulsification and most digestion occurs here (30cm).
Jejunum — most absorption occurs here (2.5m).
Ileum — vitamin B12 is absorbed (3.5m).
Where are nutrients absorbed?
© CNM: Human Sciences – Digestive System I. BQ. 42
Villi are finger-like projections with blood capillaries and lacteals (lymphatic capillaries).
Absorbed nutrients enter the blood; fatty acids enter the lymph.
Microvilli (brush border) are projections of absorptive cell membranes.
Brush border enzymes:
Enzymes attached to the intestinal lining (not free in the lumen). Include maltase, sucrase, lactase. Hence enzymatic digestion occurs
on absorptive cell surface. Release
when cells slough off.
Brush border enzymes are imperative for absorption.
The enzymes are attached to the lining of the intestine (not free in the lumen)
Brush Border Enzyme | Function |
Maltase, sucrase and lactase | Break down sugars into glucose, fructose, galactose, etc. |
Dipeptidase | Break down proteins into amino acids. |
Nucleosidases and phosphatases | Digest RNA and DNA. |
Small Intestine Hormones:
Cholecystokinin (CCK)
Cholecystokinin (CCK) is a peptide hormone that is secreted by enteroendrocrine cells
in the duodenum (small intestine).
CCK is released in response to high fat or protein chyme entering the duodenum.
CCK performs the following functions:
Stimulates the pancreas to secrete pancreatic enzymes (and hence digest fat / protein / carbohydrates).
Increases hepatic production of bile and stimulates contraction of the gall bladder (bile 🡪 fat digestion).
Mediates satiety (feeling of fullness).
© CNM: Human Sciences – Digestive System I. BQ. 46
Small Intestine
Functions:
Movement / peristalsis of food.
Digestion.
Absorption of nutrients and water.
Hunger / satiety.
Immunity — Peyer's patches and bacterial microflora.
90% of absorption occurs in small intestine.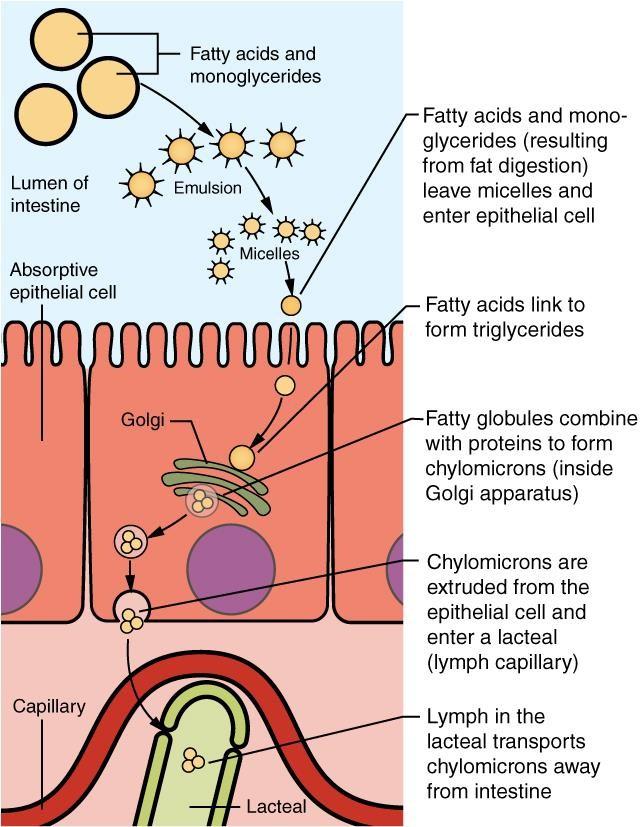
Carbohydrates and amino acids are transported into capillaries:
Monosaccharides: Active / passive transport.
Amino acids: Active transport.
Fatty acids, glycerol, cholesterol and fat- soluble vitamins (A,D,E,K) are:
Emulsified by bile.
Enter intestinal cells by simple diffusion.
Packaged into chylomicrons; absorbed into lacteals.
Travel through the lymphatic system and enter the blood in the subclavian vein.
Vitamin B12 is absorbed in the terminal ileum (needs intrinsic factor for absorption).
Vitamins, mineral salts and water enter blood capillaries and are sent to the liver (hepatic first pass).
Bile salts are reabsorbed and recycled from the ileum.
A section of mucosa in the jejunum — showing villi
Fluid Movement
All water absorption in the GI tract occurs via osmosis from the lumen into absorptive cells and into blood capillaries.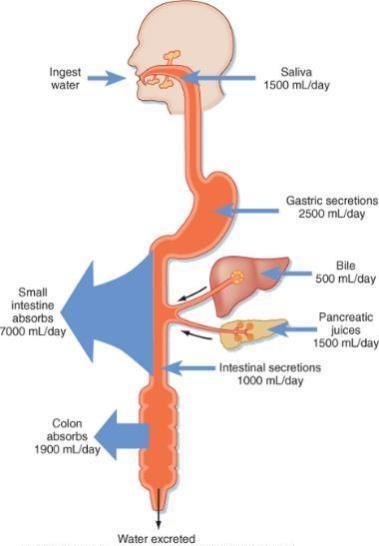
Osmosis is bi-directional — therefore, absorption of water depends on electrolyte, monosaccharide and amino acid
levels to maintain an osmotic balance / concentration gradient with the blood.
© CNM: Human Sciences – Digestive System I. BQ. 50
The large intestine is the terminal portion of the GIT, where the final stages of digestion, absorption, some vitamin synthesis (through bacterial activity)
and stool formation occurs.
The ileocaecal valve allows one-way flow
of materials from the small to large intestine.
This valve can become faulty, allowing large intestine microbes to overpopulate in the small intestine (SIBO).
Mucus is produced but no enzymes.
Absorption of water / minerals / vitamins / some drugs.
© CNM: Human Sciences – Digestive System I. BQ.
Four regions:
Caecum — appendix is attached — a twisted tube about 8cm in
length. Part of our immune system: Contains macrophages, lymphocytes, bacteria.
Colon — ascending, transverse, descending regions.
Rectum.
Anal canal — mucous membrane folds. Contains an internal and external anal sphincter.
The large intestine hosts a rich community of microbes: 100,000,000,000,000 (1x1014).
Mostly symbiotic, but pathogenic species may flourish according to local pH, poor nutrition, digestive processes further upstream and antibiotic use.
The final stages of nutrient extraction occur in the colon through microbial fermentation.
Bacteria ferment fibre to produce short chain fatty acids (SCFAs) which support GI tight junctions.
Bacterial fermentation of remaining carbohydrates produces hydrogen, CO2 and methane (flatulence).
Fermentation of residual amino acids to various compounds (including hydrogen sulphide) which contribute to faecal odour.
Some toxic products of bacterial fermentation are re-absorbed and transported to the liver where they are excreted in urine.
Bilirubin is decomposed into simpler molecules; these pigments contribute to the colour of faeces.
Produce some vitamins (B12 and vitamin K2) and fatty acids.
Faeces are 30–50% bacteria.
Mass peristaltic movements push faecal matter into the rectum from the sigmoid colon.
The resulting distension of the rectal wall stimulates stretch receptors and the defecation reflex. This includes sensory impulses to the sacral part of the spinal cord.
Motor impulses travel down parasympathetic nerves back to the rectum and anus.
Rectal muscles (with abdominal muscles and diaphragm) contract, increasing abdominal pressure that opens the internal sphincter.
The external anal sphincter is voluntarily relaxed.
Name the FOUR parts of the large intestine.
What does the large intestine absorb?
What are the functions of intestinal symbiotic microbes?
What body system will fatty acids be absorbed into after entering cells of the gut wall?
What is meant by defecation?
What is the role of cholecystokinin?
What is a brush border enzyme? Name two of them.
What is the function of villi?
What are the functions of the small intestine?
What substance is needed for B12 absorption? What produces this substance?
The liver is the heaviest gland of the body and second largest organ (skin being the largest).
Uses 27% of our resting metabolism.
It filters 1.4 litres of blood every minute.
The hepatic artery brings oxygenated blood from the heart.
Kupffer cells are phagocytic cells which remove foreign bodies from the blood (they are a type of white blood cell that specialise in engulfing microbes).
The portal vein brings in nutrient- (and toxin-) rich blood from the GIT.
Hepatic first pass: All blood from the GIT is transported to the liver (via the portal vein) to be filtered / metabolised before entering systemic circulation.
Blood from the portal vein and hepatic artery mix in the sinusoids (columns between hepatocytes).
The filtrate enters the central vein which enters the hepatic vein and into the systemic circulation.
The liver is estimated to have over 500 functions.
Cleansing blood of microbes.
Detoxification — metabolising drugs, toxins, alcohol.
Bile production and secretion.
Haemolysis (Kupffer cells)
Synthesis of plasma proteins — blood clotting and coagulation factors.
Hormone homeostasis — deactivating all hormones.
Metabolism of glucose (glycogen), fats (hepatocytes store triglycerides) and amino acids.
Heat production — thermogenesis.
Synthesis — vitamin A (from beta carotene), CoQ10 and activation of vitamin D.
Storage — vitamins (A,D,E,K, B12), iron, copper, glycogen.
• Carbohydrate:
- Excess glucose is converted to glycogen for storage.
- Glycogen to glucose as required.
• Fat:
- Metabolises fat from storage as required.
- Synthesises cholesterol and triglycerides.
• Protein:
- Converts essential amino acids into non-essential amino acids.
- Removes nitrogen groups from amino acids to form urea to be excreted.
- Breaks down nucleotides to form uric acid to be excreted.
Hepatocytes convert toxins into non-toxic metabolites which can then be excreted from the body.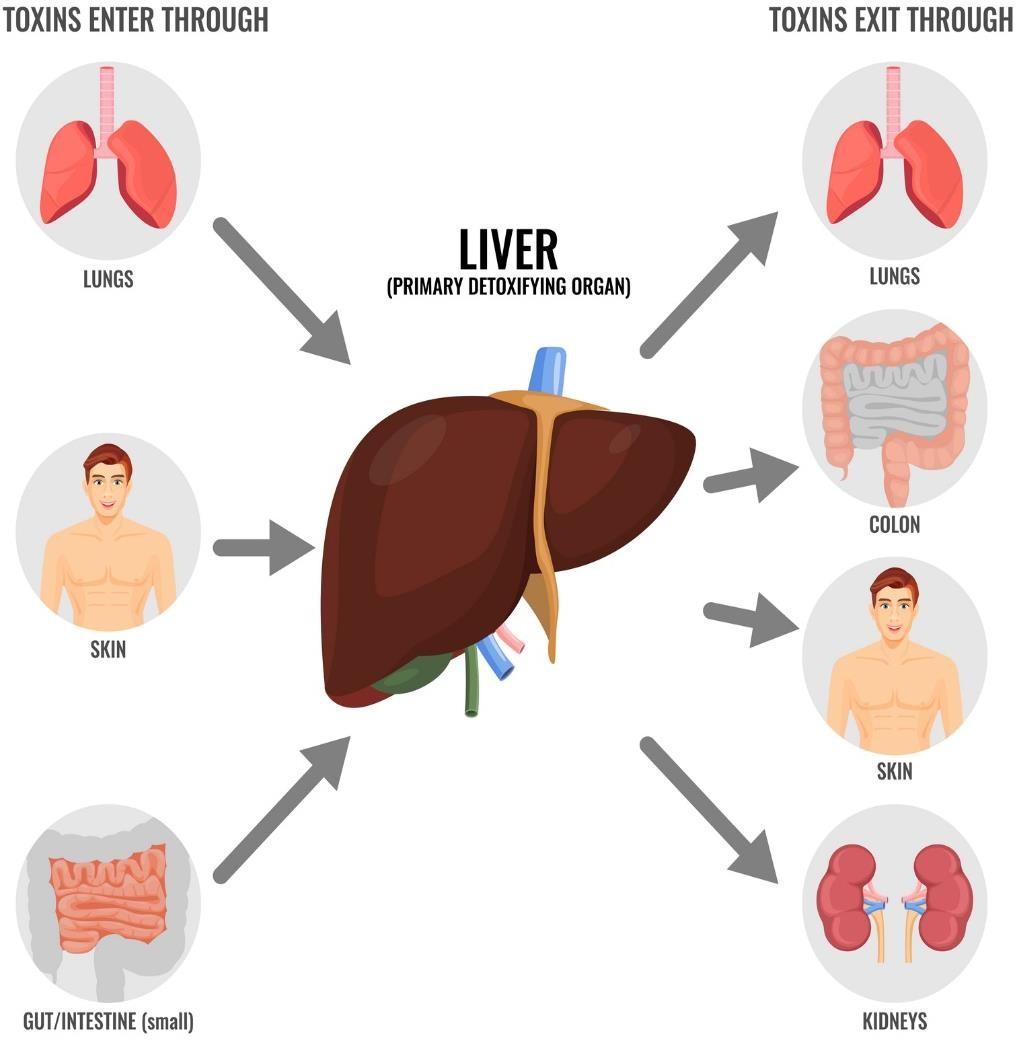
A healthy liver deals with thousands of toxins each day. These include airborne and food-borne pollutants, drugs, etc.
Highly energy dependent (ATP) and nutrient dependent.
Induced by toxicants, drugs, phytonutrients: Enzymes made on the spot.
Liver Detoxification

Two major classifications of chemical compounds:
Hydrophilic: Excreted in urine or bile.
Lipophilic: Must be chemically altered into hydrophilic compounds to facilitate elimination
Transforming lipophilic compounds is done in two phases: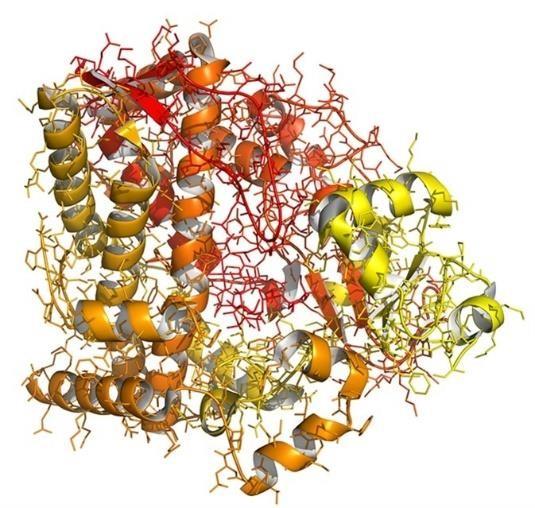
Involves CYP450 family of enzymes (a class of more than 50 enzymes).
These enzymes are particularly important in metabolising toxins and medications.
The enzymes are mostly found in liver cells but are also found in the small intestine, lungs, placenta and kidneys.
Converts water-insoluble toxins into water soluble substances to be excreted by the kidneys
Converts toxins to more reactive substances which can be metabolised in Phase II.
Conjugation reactions — molecules are attached to the toxins to neutralise them making them stable (non-reactive) and water-soluble to be excreted.
Various enzymes are involved to induce many chemical reactions.
How would you write the specific location of abdominal symptoms on your notes? How would you describe the location of a patient’s symptoms to another healthcare professional?
The abdomen can be divided into nine anatomical quadrants that helps us to be specific about locations.
The locations are divided into three main lines:
Right and left hypochondrium, epigastric region
Right and left flank, umbilical region
Right and left groin, pubic region
© CNM: Human Sciences – Digestive System I. BQ. 65
Dietary Molecules:
Dietary Carbohydrates
Monosaccharides saccharide = sugar |
|
|
Disaccharides |
|
+ glucose.
|
Polysaccharides |
|
|
Functions: Energy source (connective tissues, cell-to-cell recognition).
Cellulose and Glycogen
Cellulose is the structural material of plants
— found in plant cell walls.
Humans lack the correct enzymes to break the unique bonds between glucose molecules in cellulose, so we cannot digest it.
Instead, cellulose acts as fibre which assists
with the movement of materials through the intestines.
Dietary Lipids

Triglycerides tri- = three -glyceryl = glycerol |
unsaturated. | |
Phospholipids |
| |
Cholesterol |
|
Dietary Lipids
Functions: Energy, insulation, cell membranes, hormone production, protection of organs.
Consider that the fatty acids we ingest are ultimately incorporated into the cell membranes (phospholipid bilayer) of all cells.
The presence of a double bond means that two different molecular configurations are possible.
A cis configuration is when the H atoms are on the same side of the double bond.
A trans configuration is when the H atoms are on separate sides of the double bond.
In nature, nearly all fats have a cis structure. Our body recognises these and can use them.
When we try to create these fats in laboratories / industry, they position the H atoms on opposite sides where they have more space.
These fats are called trans fats and are associated with heart
disease. Look out for hydrogenated vegetable oil on food labels.
Proteins
Proteins are long molecules of amino acids, making up 15% of the total body mass.
Amino acid chains create a 3D structure of each protein, which is essential for them to function.
Proteins must first be denatured before protease enzymes are able to efficiently cleave the amino acids apart. Body temperature regulation allows proteins to keep a 3D shape.
Amino acids are absorbed in the small intestine.
Functions: Immunity (immunoglobulins, antibodies,), structures (muscles, collagen),
Protein structure:
72
Enzymes
Enzymes are biological catalysts which speed up chemical reactions up to thousands of times.
Enzymes
are proteins
They are highly specific regarding what substrate they react with (lock and key).
Enzyme names are usually based on the substrate they react with, and end in –ase; e.g. lactase. However, some enzymes involved in protein digestion end with –in; e.g, pepsin.
Enzymes are not changed or consumed in a chemical reaction — they can perform the same reaction many times.
Proteins are easily denatured by pH and temperature changes.
Questions:
Which of these fatty acids is cis and which is trans?
Where are cis and trans fats found?
What are the health implications of eating trans fats?