003 Week 3 & 4 study for Mini Exam 2
Week 3 & 4
Acute respiratory conditions
(1) Provide an overview of the structure and aging of the respiratory system
(2) Discuss the pathophysiology, and clinical manifestations of Asthma and other common acute respiratory conditions
(3) Discuss the risks and potential complications of common acute respiratory conditions
(1) Provide an overview of the structure and aging of the respiratory system
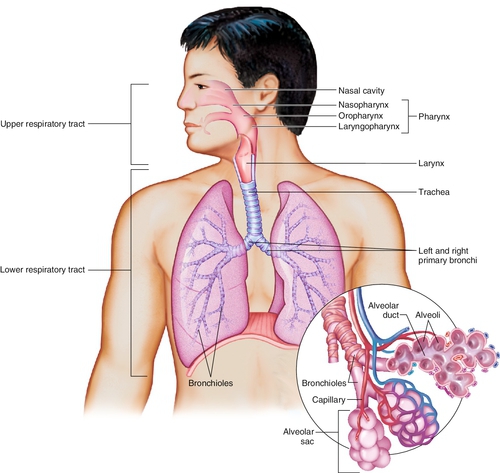
The respiratory system includes structures like:
nasal cavity
pharynx
larynx
trachea
bronchi
bronchioles
alveoli
capillaries for gas exchange
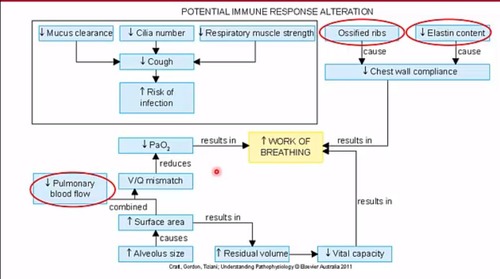
Aging can affect:
immune response
mucus clearance
cilia number
respiratory muscle strength
ribs
elastin content
cough
chest wall compliance
risk of infection
pulmonary function
gas exchange due to changes in these structures
These changes can lead to:
decreased lung functions
reduced vital capacity
increased risk of respiratory conditions like infections and asthma
(2) Discuss the pathophysiology, and clinical manifestations of Asthma and other common acute respiratory conditions
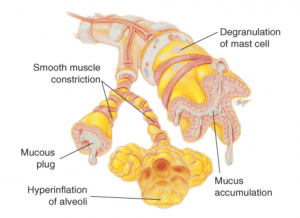
Asthma
it is characterised by intermittent or persistent airway obstruction due to factors like:
bronchial hyperresponsiveness
excess mucus production
atopy
air trapping
this leads to symptoms such as:
wheezing
SOB
chest tightness
coughing
anxiety
Pathophysiological symptoms such as:
edema
mucus
muscle spasms cause resistance to airflow
impairing expiration and leading to air trapping and alveolar hyperinflation
This results in:
uneven ventilation/perfusion
decreased pulmonary blood flow
impaired gas exchange
ultimately, hypoxemia & hypercapnia
Clinical manifestations include:
respiratory distress
increased respiratory rate
use of accessory muscles for breathing
decreased oxygen saturation levels
Asthma diagnosis involves:
history
physical examination
pulmonary function tests
laboratory studies
chest X-ray
Treatment includes:
monitoring lung function
controlling environmental triggers
pharmacologic therapy
patient education with an action plan
Pulmonary Embolism (PE)
occurs when a thrombus dislodges and occludes a pulmonary vessel, leading to decreased blood flow and hypoxia
it commonly arises from deep veins due to factors like:
venous stasis
hypercoagulability
vessel injuries
Symptoms include:
sudden chest pain
dyspnea
tachypnea
tachycardia
anxiety
The obstruction causes:
ventilation-perfusion imbalances
decreased PaO2
pulmonary infarction
HTN
decreased cardiac output
systemic hypotension
shock
PE can be life threatening and requires prompt medical intervention to prevent complications
Atelectasis
is the collapse of lung tissue due to various factors like lack of lung expansion or post-operative complications
there are 2 types:
Absorption
Compression
This condition can lead to:
decreased pulmonary blood flow
impaired gas exchange
respiratory failure
Clinical manifestations may include:
hypoxemia
hypercapnia
Mechanisms of air trapping in atelectasis involve:
issues with air movement during inspiration & expiration
mucus
bronchial plugs
muscle wall collapse
alveolar wall issues
These factors contribute to uneven ventilation/perfusion and decreased alveolar ventilation, which ca result in impaired gas exchange and respiratory failure
Pneumothorax
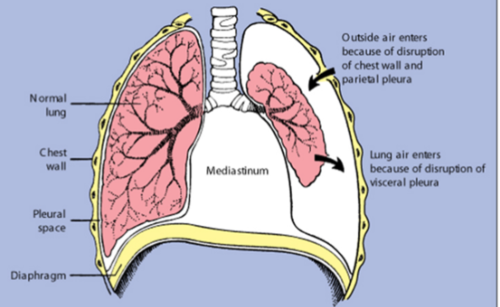
occurs when air enters the pleural space due to a rupture in the pleura
In traumatic cases, like injury, air enters through the chest wall and parietal pleura
This disrupts the pressure balance, leading to lung collapse
Clinical manifestations include:
sudden chest pain
dyspnea
tachypnea
tachycardia
anxiety
Treatment involves:
removing air from the pleural space to re-expand the lung
Pleural effusion
is the accumulation of excess fluid in the pleural space
it can be caused by various conditions like infections, heart failure, or cancer
The pathophysiology involves an imbalance between fluid production and absorption in the pleural space, leading to fluid buildup
This can case symptoms such as:
chest pain
difficulty breathing (dyspnea)
rapid breathing (tachypnea)
fast heart rate (tachycardia)
Diagnosis is usually done through imagine tests like X-rays or ultrasounds
Treatment may involve:
addressing the underlying cause
draining the fluid
medication
Aspiration
occurs when foreign substances are inhale into the respiratory tract
it can lead to:
inflammation
infection
respiratory distress
Pathophysiology involves the entry of substances like food or liquids into the airways, causing irritation, inflammation, and potential blockage
Clinical manifestations include:
coughing
wheezing
chest pain
SOB
in severe cases, aspiration pneumonia
Aspiration can lead to serious complications like lung abscess or respiratory failure if not managed promptly
Treatment involves:
supportive care
antibiotics for infections
bronchoscopy to remove the aspirated material
Pneumonia
is an infection that inflames the air sacs in one or both lungs
it can be caused by bacteria, viruses, or fungi
The pathophysiology involves the invasion of the lung tissue by the infectious agent, leading to an inflammatory response
This response causes the air sacs to fill with pus and other liquid, making it difficult to breathe
Types of pneumonia:
Community-acquired pneumonia
Streptococcus pneumoniae
Mycoplasma pneumoniae
Influenza, Legionella
Hospital-acquired (nosocomial) pneumonia
Staphylococcus aureus by fungi, protozoans
Clinical manifestations include:
cough
fever
chills
difficulty breathing
In severe cases, pneumonia can lead to complications such as respiratory failure
Risk factors for pneumonia include:
age
underlying lung disease
smoking
malnutrition
Treatment usually involves:
antibiotics for bacterial pneumonia
antiviral medications for viral pneumonia
supportive care to relieve symptoms
Bronchiolitis
is a common lower respiratory tract infections, often seen in children under 2 years old
it is mainly caused by the respiratory syncytial virus (RSV)
Clinical manifestations include symptoms like:
runny nose (rhinorrhoea)
cough
poor feeding
labored breathing (dyspnea)
Bronchiolitis is highly contagious
The pathophysiology involves inflammations and obstruction of the small airways in the lungs, leading to symptoms and potential complications
Croup (Acute laryngotracheobronchitis)
is an acute condition affecting the upper airway, commonly seen in children aged 6 months to 5 years
it is often caused by viruses like:
parainfluenza
infleunza A
RSV
The microorganism enters the upper airway, triggering an inflammatory response that leads to swelling and oedema in the upper airway
This swelling can cause upper airway obstruction, resulting in symptoms like a seal-like barking cough
The inflammation and oedema increase resistance to airflow, leading to increased negative pressure in the chest and potential collapse of the upper airway
Clinical manifestations of croup include a:
barking cough, which is distinctive, and the condition is usually self-limiting but may require glucocorticoids to reduce inflammation if severe
(3) Discuss the risks and potential complications of common acute respiratory conditions
Review of the Respiratory System
(1) Review the structure and function of the Respiratory system, related to breathing and respiration and perfusion.
(2) Introduce tests relating to measurement of ventilation
(3) Gain an overview of the development of the respiratory system in the unborn.
(4) Consider the effects of aging on the respiratory system
(1) Review the structure and function of the Respiratory system, related to breathing and respiration and perfusion.
The respiratory system consists of the lungs, airways, and muscles involved in breathing
Air is inhaled through the nose or mouth, travels down the trachea, and enters the lungs through bronchial tubes
In the lungs, oxygen is exchanged for carbon dioxide in tiny air sacs called alveoli
This process is known as respiration
Perfusion, the process of oxygenated blood being delivered to tissues, os facilitated by the respiratory system through the exchange of gases in the alveoli
the diaphragm and intercostal muscles play a crucial role in breathing by expanding and contracting the chest cavity to allow air in and out of the lungs
Overall, the respiratory system ensures the intake of oxygen and removal of carbon dioxide, supporting the body’s metabolic functions
(2) Introduce tests relating to measurement of ventilation
The tests relating to the measurement of ventilation include:
Tidal Volume (TV)
which measures the volume of air breathed in and out during quiet breathing
Vital Capacity (VC)
is the maximum air amount inhaled and exhaled with forced breathing
Forced Vital Capacity
measures the maximum air exhaled forcefully
Forced Expiratory Volume in 1 second (FEV1)
measures the maximum air exhaled in one second
Residual Volume (RV)
is the air volume left in the lungs after forceful exhalation
Total Lung Capacity (TLC)
is the total air amount in maximally expanded lungs, calculated as the sum of RV and VC
These tests provide valuable information about lung function and can help diagnose respiratory conditions
(3) Gain an overview of the development of the respiratory system in the unborn.
The development of the respiratory system in the unborn goes through 5 stages:
Embryonic stage (0-7 weeks)
Psuedogladular stage (7-16 weeks)
Canalicular stage (16-25 weeks)
Saccular stage (25-36 weeks)
Alveolar stage (36 weeks - 6-8 years)
During these stages, the lungs undergo significant growth and maturation, with the alveolar stage being the final stage where the alveoli, responsible fir gas exchange, continue to develop postnatally.
This process is crucial for the unborn to be able to breathe independently after birth
(4) Consider the effects of aging on the respiratory system
Aging affects the respiratory system in various ways
With age, there is a reduction in elastic fibers in the lungs, decreased respiratory muscle strength, and reduced cilia activity
Additionally, there is a decrease in cough efficiency, making older individuals more vulnerable to respiratory infections
The ribs can calcify, the vertebrae can develop osteoporosis, and the alveoli can become “baggy”, leading to decreased lung function
These changes can result in diminished ventilatory response to hypoxia and hypercapnia, making older individuals more susceptible to ventilatory failure or pnuemonia
Nerves triggering coughing become less sensitive, further compromising the respiratory defense mechanisms
Acid/Base Regulation
(1) Review the basics – acids and bases (alkali)
(2) Discuss the role of hydrogen ion concentration in cellular function and dysfunction
(3) Describe how buffering systems help prevent significant fluctuations in pH
(4) Differentiate between respiratory and metabolic acid-base disorders by causes and mechanisms of compensations
(1) Review the basics – acids and bases (alkali)
Acids
are substances that donate protons (H+) when dissolved in water
they can be identified by their sour taste, ability to turn blue litmus paper red, and their corrosive nature
Examples of acids include:
hydrochloric acid (HCl) found in the stomach
Citric acid in citrus fruits
Acetic acid in vinegar
Acids plays a crucial role in various chemical reactions and are essential in many biological processes
Bases
also known as alkalis, are substances that receive protons (H+)
they can neutralize acids by accepting hydrogen ions
Examples of bases include:
metal hydroxides like sodium hydroxide (NaOH) & Potassium hydroxide (KOH)
in the context of cellular function, bases help maintain the pH balance by counteracting the acidic effects of hydrogen ions
This balance is crucial for various cellular processes to function optimally
(2) Discuss the role of hydrogen ion concentration in cellular function and dysfunction
Hydrogen ion concentration plays a crucial role in cellular function and dysfunction
In cellular function,
hydrogen ions are involved in maintaining the normal pH level within cells, which is vital for various cellular to function optimally
for example,
enzymes, which are essential for biochemical reactions in cells, have an optimal pH range for their activity, and any significant deviation in hydrogen ion concentration can affect their function
In cellular dysfunction,
an imbalance in hydrogen ion concentration can lead to acid-base disorders, disrupting cellular activities
For instance,
acidosis, which is characterised by increased hydrogen ion concentration, can interfere with normal cellular functions and lead to serious conditions like hyperkalemia
Therefore, maintaining the balance of hydrogen ions is crucial for proper cellular function and overall health
(3) Describe how buffering systems help prevent significant fluctuations in pH
Buffering systems help prevent significant fluctuations in pH by quickly neutralizing excess acids or bases in the body
The plasma buffer system, respiratory system, and kidneys work together to maintain pH homeostasis
For example,
the respiratory system responds rapidly to pH changes by adjusting CO2 levels
the kidneys, although slower to react, can continue buffering for extended periods by excreting H+ ions and regulating bicarbonate levels
By working in tandem, these systems ensure that pH remains within the normal range, preventing acidosis or alkalosis
(4) Differentiate between respiratory and metabolic acid-base disorders by causes and mechanisms of compensations
Respiratory base disorders are caused by changes in carbon dioxide levels, leading to acidosis (elevated pCO2) alkalosis (low pCO2) due to hypoventilation or hyperventilation, respectively.
Metabolic base disorders result from changes in bicarbonate levels, causing acidosis (reduced HCO3-) or alkalosis elevation of HCO3-) due to non-carbonic acid accumulation or excessive loss of metabolic acids
Compensatory mechanisms involve the kidneys and lungs regulating bicarbonate and carbon dioxide levels to restore pH balance
Respiratory acidosis
is caused by elevated pCO2 due to alveolar hypoventilation, leading to a decrease in pH
The compensation mechanism involves the kidneys retaining bicarbonate (HCO3-) to help normalize pH levels
Metabolic acidosis
is characterised by reduced HCO3- levels or an increase in non-carbonic acids, lowering pH
the compensation mechanism for metabolic acidosis involves the respiratory system increasing ventilation to eliminate carbon dioxide, this raising pH levels
Trauma & Abuse
(1) Understand the impact of adverse childhood events on the individual, whanau and community.
(2) Identify anatomical and pathophysiological changes in child trauma.
(3) Discuss impact of adverse childhood events on adult life
(4) Describe neuroplasticity of the brain
(1) Understand the impact of adverse childhood events on the individual, whanau and community.
Adverse childhood events can have profound impacts on individuals, families (whanau), and communities
Individuals may exhibit behavioural reactions like:
anger
avoidance
anxiety
low confidence
Families can experience:
stress
gried
feelings of failure
Communities may see:
increased violence
aggression
lack of trust
These events can lead to a rang of emotional, psychological, and social challenges that affect the overall well-being of individuals, families, and communities
The long-term effects can include relationships, and even societal problems like crime and substance abuse
It is crucial to address these impacts through support systems, therapy, and community interventions to mitigate and lasting consequences of adverse childhood events
(2) Identify anatomical and pathophysiological changes in child trauma.
Childhood trauma can lead to anatomical and pathophysiological changes in the brain
For example, prolonged exposure to stress hormones like cortisol can impact the development of brain regions involved in emotional regulation and memory, such as the amygdala and hippocampus
These changes can result in alterations in brain structure and function, affecting a child’s ability to cope with stress and regulate emotions
Additionally, trauma can disrupt the formation of neural connections and impact neurotransmitter systems, leading to long-term changes in brain circuitry and functioning
These alterations may contribute to symptoms of anxiety, depression, and other mental health issues commonly seen in individuals who have experienced childhood trauma
(3) Discuss impact of adverse childhood events on adult life
Adverse childhood events can have a significant impact on adult life
Individuals who experience ACEs are at a higher risk of mental and physical illnesses, as well as engaging in dysfunctional behaviours in adulthood
These experiences can lead to difficulties in regulating emotions, forming healthy relationships, and coping with stress
The trauma from childhood can manifest in various ways in adulthood, such as:
increased anxiety
depression
substance abuse
even physical health issues like heart disease or diabetes
Additionally, ACEs can affect cognitive function and decision-making abilities, leading to challenges in work, relationships, and overall well-being
Overall, the impact of adverse childhood events on adult life is profound and can have long-lasting consequences on an individual’s mental, emotional, and physical health
(4) Describe neuroplasticity of the brain
Neuroplasticity refers to the brain’s ability to reorganize itself by forming new neural connections throughout life
this process allows the brain to adapt to new experiences, learn new information, and recover from injuries
involves changes in brain structure, such as global volumetric changes, limbic circuitry, frontal regions, cerebellum, and structural connectivity
It is influenced by both genetics and environmental factors, shaping brain development
For example, trauma can impact brain development by affecting the reptillian brain, limbic system, and neocortex, leading to challenges in cognition, emotional regulation, and survival instincts
Overall, neuroplasticity plays a crucial role in how the brain responds to various stimuli and experiences, highlighting its dynamic and adaptive nature
High Risk Behaviours
(1) Describe the neuroscience of high risk behaviours
(2) Discuss possible pathophysiology of suicide and risk factors
(3) Discuss possible pathophysiology of self harm and risk factors
(1) Describe the neuroscience of high risk behaviours
High-risk behaviours involve actions that can lead to harm or negative consequences
In terms of neuroscience, these behaviours are often linked to the brain’s reward system.
when engaging in high-risk behaviours, the brain’s reward pathways, particularly the release of dopamine, can be activated
This activation reinforces the behaviours, making it more likely to be repeated despite the potential negative outcomes
Additionally, factors like genetics, environment, and past experiences can influence an individual’s propensity for engaging in high-risk behaviours by affecting brain function and decision-making processes
These behaviours can become ingrained due to neuroplasticity, where the brain adapts and changes in response to repeated behaviours
(2) Discuss possible pathophysiology of suicide and risk factors
The possible pathophysiology of suicide involves factors like low levels of brain-derived neurotrophic factor (BDNF) and serotonin,
Low BDNF levels are lined to suicide, major depression, PTSD, schizophrenia, and OCD
Post-mortem studies show reduced BDNF in the hippocampus and prefrontal cortex
Serotonin, a neurotransmitter, is believed to be low in those who die by suicide, with evidence of reduced breakdown product levels in the cerebral spinal fluid
Risk factors for suicide include:
history of depression
anxiety
previous suicide attempts
PTSD
family history
genetic vulnerability
ethnicity
age
poverty
psychosis
knowing someone who died by suicide
These factors, along with demographic, distal, proximal factors, and suicidal ideation, contribute to the complex pathophysiology of suicide
(3) Discuss possible pathophysiology of self harm and risk factors
Self-harm, or Non-Suicidal Self-Injury (NSSI), can be influenced by various risk factors
The possible pathophysiology involves a complex interplay of psychological and biological factors
Individuals may engage in self-harm as a maladaptive coping mechanism to deal with emotional distress, trauma, or mental health issues like anxiety and depression
Isolation, being bullied, and adverse childhood experiences (ACEs) can also contribute to self-harm behaviour
The presence of previous NSSI and exposure to NSSI in peers can normalize and reinforce self-harm tendencies
Additionally, underlying mental health conditions can increase the likelihood of engaging in self-harm as a way to regulate emotions or numb psychological pain
Overall, self-harm can be a manifestation of deeper emotional struggles and a cry for help
Pharmacology in Mental Health
(1) Be able to explain one commonly prescribed medication from each major class of mental health medications
Anxiolytics (Anti-anxiety, Sedatives, Hypnotics)
Alprazolam (Xanax) is benzodiazepine used to treat anxiety disorders
Anti-psychotics (Typical and Atypical)
Aripiprazole (Abilify) is an atypical antipsychotic used to treat schizophrenia and bipolar disorder
Anti-depressants
Sertraline (Zoloft) used to treat depression and anxiety disorders
Stimulants
Methylphenidate (Ritalin) is a common stimulant used to treat attention deficit hyperactivity disorder (ADHD)
(2) Describe the effects on the CNS, indications for use, and Adverse effects and associated risks for:
Anxiolytics (Anti-anxiety, Sedatives, Hypnotics)
Anxiolytics like Benzodiazepine (Diazepam/Valium) act of GABA receptors in the CNS, causing sedation and reducing anxiety by affecting the amygdala in the limbic system
They are used for anxiety and panic disorders, and in alcohol withdrawal
Adverse effects include:
fatigue
drowsiness
muscle weakness
risk of dependence
requiring a long withdrawal period
They are contraindicated in conditions like COPD and liver disease due to potential complications
These medications have CNS depressant effects, are indicated for anxiety-related conditions, and carry risks for side effects and dependency
Anti-psychotics (Typical and Atypical)
Atypical anti-psychotics like Quetiapine (Seroquel) act on CNS receptors for Dopamine and Serotonin, providing a calming effect
they are used for acute and chronic psychosis, schizophrenia and bipolar disorder
Adverse effects include:
increased suicide risk
hypotension
metabolic syndrome exacerbation
dizziness
weight gain
Typical anti-psychotics like Haloperidol (Serenace) at on multiple CNS neurotransmitter receptors, especially Dopamine, leading to extrapyramidal effects
they are indicated for psychosis, schizophrenia, and alcoholic delusions
Adverse effects include:
extrapyramidal effects (movement disorders)
dizziness
constipation
confusion
drowsiness
Anti-depressants
like Fluoxetine (Prozac)
the CNS effects involve inhibiting the reuptake of serotonin, leading to increased serotonin levels in the synaptic space, which helps regulate mood
Indications for use include treating:
depression
anxiety
bulimia nervosa
OCD
premenstrual dysphoric disorder
panic disorder
PTSD
Adverse effects and associated risks may include:
initial increased risk of suicidal thoughts
weight loss
nausea
vomitting
headaches
rashes
dizziness
Stimulants
like amphetamines and methylphenidate
have CNS effects by stimulating neuron activity in excitatory pathways, affecting parts of the brain like the cerebral cortex and limbic region
These drugs are indicated for ADHD treatment
However, they come with adverse effects and risk such as potential:
addiction
insomnia
headache
irritability
nausea
Prolonged use can lead to:
mood changes
depression
agitation
psychosis
These drugs act on neurotransmitters like dopamine & norepinephrine, impacting:
focus
attention
impulse control in individuals with ADHD
(3) Be able to describe the difference between a chemical name, generic name and brand name
The chemical name refers to the exact molecular structure of a drug, providing detailed information about it composition
The generic name is the official name of the drug, usually derived from its chemical name and recognised by health professionals world wide
The brand name is the trademarked name given by the pharmaceutical company marketing the drug
It is unique to that specific company and is used for marketing purposes
For example,
the chemical name for Aspirin is Acetylsalicylic acid, the generic name is Aspirin, and the brand name could be Bayer Aspirin