SCHIZOPHRENIA-reviewer_say.docx
SCHIZOPHRENIA
Distorted and bizarre thoughts, perceptions, emotions, movements, and behavior. It cannot be defined as a single illness; rather, schizophrenia is thought of as a syndrome or a disease process with many different varieties and symptoms, much like the varieties of cancer.
Schizophrenia usually is diagnosed in late adolescence of early adulthood. Rarely does it manifest in childhood. The peak incidence of onset is 15 to 25 years of age for men and 25 to 35 years for women.
Schizophrenia: Some Facts and Statistics
- Onset and prevalence of schizophrenia worldwide
- About 0.2% to 1.5% (or about 1% population)
- Often develops in early adulthood
- Can emerge at any time
- Schizophrenia is generally chronic
- Most suffer with moderate-to-severe lifetime impairment
- Life expectancy is slightly less than average
- Schizophrenia affects males and females about equally
- Females tend to have a better long-term prognosis
- Onset differs between males and females
Schizophrenia has a strong genetic component
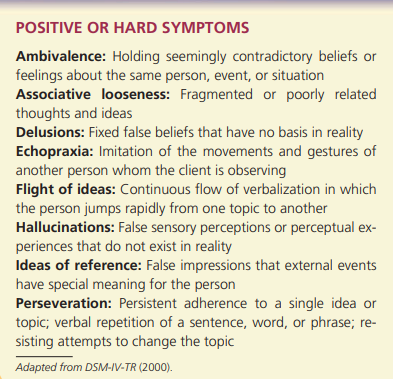
Positive symptoms
- Hallucinations, most often auditory
- Delusions of grandeur, persecution, etc.
- Disordered thought process
- Bizarre behaviors
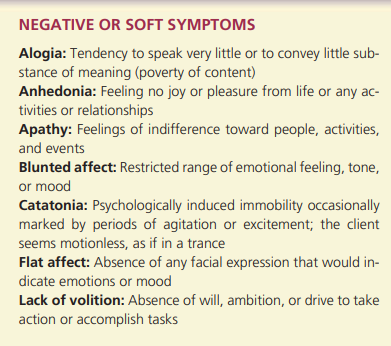
Negative symptoms
Social withdrawal
Flat affect (blunted emotional responses)
Anhedonia (loss of pleasurable feelings)
Reduced motivation, poor focus on tasks
Alogia (reduced speech output)
Catatonia (reduced movement)
Schizophrenia: The “Positive” Symptom cluster
- The positive symptoms
- Active manifestations of abnormal behavior.
- Distortions of normal behavior
- Delusions: The basic feature of psychosis
- Gross misinterpretations of reality
- Include delusions of grandeur or persecution
- Hallucinations: auditory and/or visual
- Experience of sensory events without environmental input
- Can involve all senses
- Findings from SPECT studies
Schizophrenia: The “Negative” Symptom cluster
- The negative symptoms
- Absence or insufficiency of normal behavior
- Spectrum of negative symptoms
- Avolition (or apathy): lack of initiation and persistence
- Alogia: relative absence of speech
- Anhedonia: lack of pleasure, or indifference
- Affective learning: little expressed emotion
- Asociality: isolation from public
Schizophrenia: The “Disorganized” Symptom cluster
- The disorganized symptoms
- Include severe and excess disruptions
- Speech, behavior, and emotion
- Nature of disorganized speech
- Cognitive slippage: illogical and incoherent speech
- Tangentiality: “Going off on a tangent”
- Loose associations: conversation in unrelated directions
- Nature of disorganized affect
- Inappropriate emotional behavior
- Nature of disorganized behavior
- Includes a variety of unusual behaviors
- Catatonia: Spectrum
- Wild agitation, waxy flexibility, immobility
Course of illness
- Course of schizophrenia
- Continuous without temporary improvement
- Episodic with progressive or stable deficit
- Episodic with complete or incomplete remission
- Typical stage of schizophrenia:
- Prodromal phase
- Active phase
- Residual phase
Subtypes of schizophrenia
- Paranoid type
- Intact cognitive skills and affect
- Do not show disorganized behavior
- Hallucinations and delusions: Grandeur or persecution
- The best prognosis of all types of schizophrenia
- Delusions of grandeur or persecution
- Hallucinations (especially auditory)
- Higher level of functioning between episodes
- May have stronger familial link than other types
- Disorganized type (Hebephrenic)
- Marked disruptions in speech and behavior
- Flat or inappropriate affect
- Hallucinations and delusions: tend to be fragmented
- Develops early, tends to be chronic, lacks remissions
- Disorganized speech and/or behavior
- Immature emotionality (inappropriate affect)
- Chronic and lacking in remissions
- Catatonic type
- Show unusual motor responses and odd mannerisms
- Examples include echolalia and echopraxia
- Tends to be severe and rare
- Alternating immobility and exited agitation
- Unusual motor responses (waxy flexibility, rigidity)
- Odd facial or body mannerisms (often mimicking others)
- rare
- Undifferentiated type (Atypical schizophrenia)
- Wastebasket category
- Major symptoms of schizophrenia
- Fail to meet criteria for another type
- Symptoms of several types that taken together do not neatly fall into one specific category
- Residual type
- One past episode of schizophrenia
- Continue to display less extreme residual symptoms
- Person has had at least one schizophrenic episode but no longer shows major symptoms
- Still shows “leftover” symptoms (social withdrawal, bizarre thoughts, inactivity, flat effect)
DSM-IV diagnostic criteria for schizophrenia
- Two of the following for most of 1 month:
- Delusions
- Hallucinations
- Disorganized speech
- Grossly disorganized or catatonic behavior
- Negative symptoms
- Marked social or occupational dysfunction
- Duration of at least 6 months of persistent symptoms
- Symptoms of schizoaffective & mood disorder are ruled out
- Substance abuse & medical conditions are ruled out as etiological
Causes of schizophrenia: Findings from genetic research
- Family studies
- Inherit a tendency for schizophrenia
- Do not inherit specific forms of schizophrenia
- Risk increases with genetic relatedness
- Twin studies
- Monozygotic twins: risk for schizophrenia in 48%
- Fraternal (dizygotic) twins: risk drops to 17%
- Adoption studies: risk for schizophrenia remains high
- Cases where a biological parent has schizophrenia
- Summary of genetic research
- Risk for schizophrenia increases with genetic relatedness
- Risk is transmitted independently of diagnosis
- Strong genetic component does not explain everything
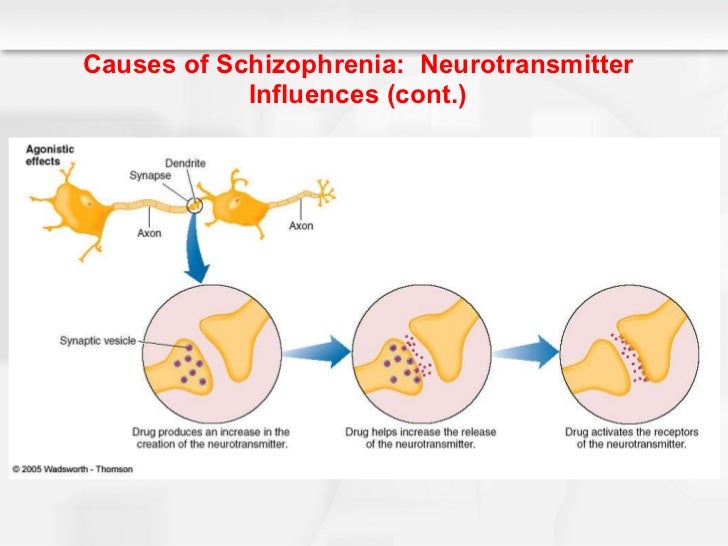
Causes of schizophrenia: Neurotransmitter influences
The Dopamine Hypothesis
Drugs that increase dopamine (agonists)
- Result in schizophrenic-like behavior
Drugs that decrease dopamine (antagonists)
- Reduce schizophrenic-like behavior
Examples: neuroleptics, L-Dopa for Parkinson’s disease
Current theories: emphasize many neurotransmitters (serotonin, GABA,& Glutamate) also have a role
Causes of schizophrenia: Other neurobiological influences
- Structural and Functional abnormalities in brain
- Enlarged ventricles and reduced tissue volume
- Hypo frontality: less active frontal lobes
- A major dopamine pathway
- Viral infections during early prenatal development
- Findings are inconclusive
- Structural and functional brain abnormalities
Not unique to schizophrenia
Causes of schizophrenia: Psychological and social influences
- The role of stress
- May activate underlying vulnerability
- May also increase risk of relapse
- Family interactions
- Families: show ineffective communication patterns
- High expressed emotion: associated with relapse
- The role of Psychological factors
- Exert only a minimal effect in producing schizophrenia
Treatment of schizophrenia
- The acute schizophrenic patients will respond usually to antipsychotic medication
- Development of antipsychotic (neuroleptic medications
- Often the first line treatment for schizophrenia
- Began in 1950s
- Most reduce or eliminate positive symptoms
- Acute and permanent side effects; (extrapyramidal and Parkinson-like side effects, Tardive dyskinesia)
- Compliance with medication is often a problem
- According to current consensus we use in the first line therapy the newer atypical antipsychotics, because their use in not complicated by appearance of extrapyramidal side-effects, or these are much lower than with classical antipsychotics
- Conventional antipsychotics – (classical neuroleptics)
- Chlorpromazine
- Clopenthixole
- Levopromazine
- Thioridazine
- Droperidole
- Flupentixol
- Fluphenazine
- Haloperidol
- Perphenazine
- Pimozide
- Prochlorperazine
- Trifluoperazine
- Depot antipsychotics: (Fluphenazine deconate-Modecate)
- Flupenthixol
- Zuclopenthixole
- Atypical antipsychotics – (new neuroleptics);
- Amisulpiride
- Clozapine
- Olanzapine
- Quetiapine
- Risperidone
- Sertindole
- Sulpiride
Psychosocial Treatment of schizophrenia
- Psychosocial approaches:
- Behavioral (i.e., token economies) on inpatient units
- Community care program
- Social and living skills training
- Behavioral family therapy
- Vocational rehabilitation
Electroconvulsive Therapy (ECT) is also used in the treatment of schizophrenia, but may be useful when catatonia or prominent affective symptoms are present.
Prognosis
- Good prognosis
- Old age of onset
- Female
- Married
- No family history
- Good premorbid personality
- High IQ
- Precipitants
- Positive symptoms
- Treatment compliance
- Good support
- Acute onset
- Presence of mood component
- Poor prognosis
- Young age of onset
- Male
- Unmarried
- Family history
- Personality problems
- Low IQ
- No obvious precipitants
- Negative symptoms
- Poor treatment compliance
- Low support
- Insidious onset
- No mood component
Summary of schizophrenia
- Schizophrenia – spectrum of Dysfunctions
- Affecting cognitive, emotional and behavioral domains
- Positive, negative, and disorganized symptoms clusters
- DSM-IV and DSM-IV-TR
- Five subtypes of schizophrenia
- Includes other disorders with psychotic features
- Several Bio-Psycho-Social variables are involved
- Successful treatment rarely includes complete recovery
PSYCHOTIC DISORDER
| Onset | Symptoms | Course | Duration | |
|---|---|---|---|---|
| Schizophrenia | Usually insidious | Many | Chronic | >6 mo. |
| Delusional disorder | Varies (Usually insidious) | Delusions only | Chronic | >1 mo. |
| Brief psychotic disorder | Sudden | varies | Limited | <1mo. |
Other psychotic disorders
- Schizophreniform Disorder
- Schizophrenic symptoms for a few months (less than 6 months)
- Associated with good premorbid functioning
- Most resume normal lives
- The same treatments recommended for schizophrenia may also be utilized here
- Brief psychotic disorder
- One or more positive symptoms of schizophrenia
- Usually precipitated by extreme stress or trauma
- Experience a psychosis which, while lasting at least a day, undergoes a full, complete and spontaneous remission within one month
- Tends to remit on its own
- Delusional disorder
- Delusions that are contrary to reality
- Lack other positive and negative symptoms
- Types of delusions include:
Erotomanic, Grandiose, Jealouse, Prosecutory, Somatic
- Appears to purse a chronic, waxing and waning course
- Patients with paranoia rarely seek tx with a psychiatrist on their own initiative
- Better prognosis than schizophrenia
- Shared psychotic disorder (Folie à Deux)
- Delusion from one person manifest in another person
- The most common relationships are among parents and children, spouses and siblings
- Separation from the dominant person and immersion into normal social interaction.
- Schizoaffective disorder
- Symptoms of schizophrenia and a mood disorder
- Both disorders are independent of one another
- Such persons do not tend to get better on their own
- Long-term outcome of patients is not good as that for patients with a mood disorder, yet not as grave as that for patients with schizophrenia.
--------------------------
- Schizotypal disorder
- Characterized by eccentric behavior and by deviations of thinking and affectivity, which are similar to that occurring in schizophrenia, but without psychotic features and expressed symptoms of schizophrenia of any type.
- May affect a less severe form of schizophrenia
- Postpartum psychosis (puerperal psychosis)
- Rare disorder, occurring in perhaps less than 1 or 2 per 1000 deliveries
- It is more common in primiparous than in multiparous women
- Many of these patients never experience another psychotic illness unless they again become pregnant
- Symptoms generally appear abruptly within about 3 days to several weeks after delivery
- Hospitalization is generally indicated