Nervous System & Mental Health
Nervous System - Enormous network of nerve fibers traversing the human body.
Functions as both the central operator and central intelligence for the body.
Regulates body functions and provides an internal method of communication between the brain and other organs. And between the organism and the environment.
The brain also regulates subconscious bodily functions, such as respiratory rate, body temperature, and peristalsis of the intestines.
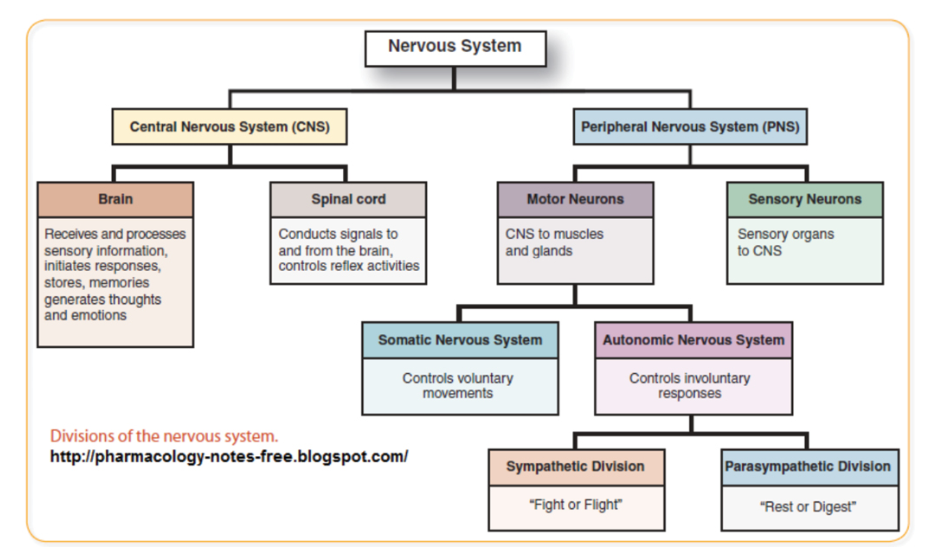
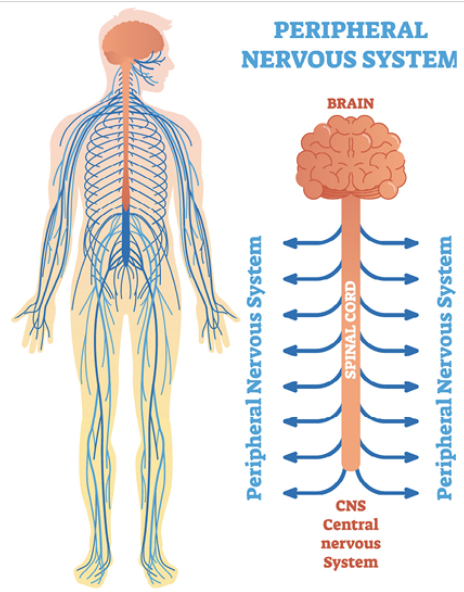
Composed of 2 parts:
Central Nervous System (CNS)
Brain and spinal cord
Command center
Peripheral Nervous System (PNS)
Cranial and spinal nerves
Serves as the communication lines linking all parts of the body to the CNS
Somatic Nervous System - voluntary body movements
Autonomic Nervous System - involuntary body movements
Body System:
Cerebell/o - cerebellum
Cerebr/o - cerebrum
Cortic/o - cerebral cortex
Encephal/o - brain
Gangli/o & ganglion/o - ganglion
Gli/o - neuroglia
-lalia - babble or speech
-lepsy - seizure
-lexia - reading
-mania - obsessive or excited state
Medull/o - medulla oblongata, spinal cord
Mening/o & meninge/o - meninges
Myel/o - spinal cord
Narc/o - unconsciousness or stupor
Neur/o, Neur/I - nervous system, tissues, or nerves
-paresis - weakness
-phasia - speech
-phobia - irrational and persistent fear
-plegia - paralysis
-psych/o - mind
Radicul/o - spinal nerve root
Somn/o - sleep
Thalam/o - thalamus
Ventricul/o - ventricle, cavity
Nervous System:
Amnesia - Loss of memory
Ataxia - Loss of muscular coordination
Axon - A fiber in the neuron that carries impulses away from the body of a cell
Bradykinesia - Abnormal or slowness of motion
Central Nervous System - The brain and spinal cord
Cephalgia/cephalalgia - Headache
Cerebrospinal - Surgical opening into the skull
Craniotomy - Surgical opening into the skull
Dendrite - A fiber in the neuron that carries impulses toward the body of a cell
Discectomy - Surgical excision of an intervertebral disc
Dysphasia - Impairment of speech (syn. -aphasia)
Encephalomalacia - Softening of the brain often due to ischemia or infarction
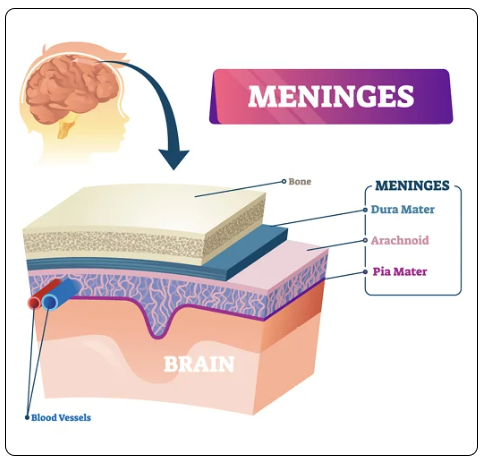
Epidural - Pertaining to above or outside the dura mater
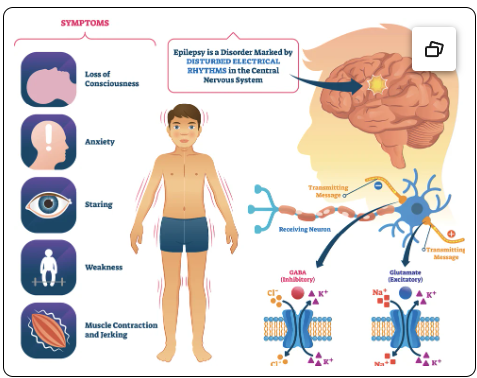
Epilepsy - a brain disorder characterized by electrical-like disturbances resulting in seizures
Gray Matter - Axons that are not covered in myelin
Hemiparesis - Weakness on one side of the body
Intracranial - Within the skull
Intrathecal administration - Injection into the spinal canal or subarachnoid space
Laminectomy - Excision of the vertebral posterior arch or spinal process
Meningitis - Inflammation of the meninges or the membranes covering the spinal cord or brain
Myelin - A substance that covers some axons to insulate, protect, and assist in electrical conduction
Myelitis - Inflammation of the meninges or the membranes covering the spinal cord or brain
Neuralgia - Severe or stabbing pain in the course or distribution of a nerve
Neuritis - Inflammation of a nerve
Neurologist - Physician who specializes in diagnosis and treatment of disorders of the nervous system
Neurolysis - Destruction of nerve tissue or lysis (breaking up) perineural adhesions
Neuron - Basic functional unit of the nervous system
Neurorrhaphy - Repair of severed nerve by suture, graft, or synthetic conduit
Neurosis - Emotional condition or disorder; anxiety is a primary characteristic
Neurotransmitters - a chemical that transmits energy across a synapse
Paranoia - A mental disorder, often includes delusions involving persecution
Peripheral nervous system - nerves outside of the brain and spinal cord
Poliomyelitis - Inflammation of gray matter of the spinal cord
Psychosis - an abnormal condition of the mind, gross disorganization, or distortion of mental capacity
Quadriplegia - Paralysis of all four extremities
Radiculitis - Inflammation of the spinal nerve roots
Sciatica - Severe pain along the sciatic nerve, usually unilateral based on the nerve root affected
Subdural - Below the dura mater
Vagotomy - Surgical incision of the vagus nerve
White matter - axons that are covered in myelin
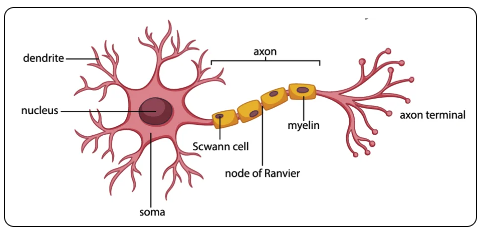
Neuron - A single nerve cell, comprised of a soma (or cell body), containing the cell nucleus, several dendrites and an axon
Dendrites - resemble tree branches and increase the number of possible connections among nerve cells. Picking up signals that travel through the cell and continue along the axon and transmitted to the next cell.
Axon Terminals (synaptic bulbs) - the ends of axons that release neurotransmitters to send messages to other cells.
Axon terminals of a transmitting neuron and dendrites of a receiving neuron do not touch. They are separated by a space called a synapse.
Synapse - minute electrical impulses are passed from one nerve to another via chemical messengers called neurotransmitters (such as serotonin)
Neurotransmitters - chemical messengers that carry signals between neurons, muscles, and glands in the body.
Control everything from thoughts and emotions to movement and sleep.
Disruption of normal production or function of neurotransmitters may cause mood and attention disorders
Central Nervous System (CNS)
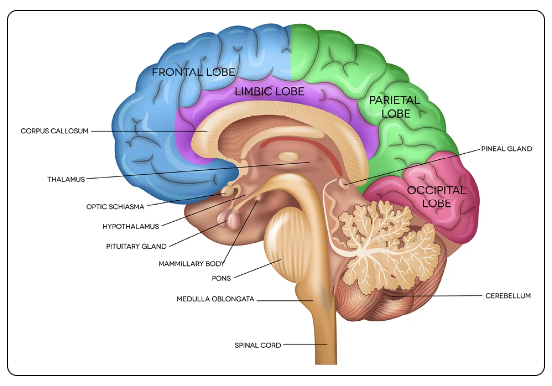
Brain: Divided into distinct regions
Cerebrum -
located in the supratentorial region
Fontal, temporal, parietal, and occipital lobes
Frontal Lobe - front part of the brain, involved in planning, organizing, problem solving, selective attention, personality, and a variety of higher cognitive functions including behavior and emotions
Temporal Lobes - 2 lobes, one on either side of the brain. Right lobe involves visual memory; left lobe mainly involves verbal memory. Both lobes help sort new information and are believed to be responsible for short-term memory. Evaluate hearing input and smell.
Parietal Lobes - lie behind the frontal lobe and above the temporal lobes, at the top of the brain. Contains primary sensory cortex controlling sensation. Right parietal lobe processes visuospatial info; left lobe processes spoken and written info
Occipital Lobe - in the back of the brain and processes visual info, like recognition of shapes and colors
Cerebellum - located in the infratentorial region at the "bottom" of the brain, below the occipital lobe; helps coordinate movement (balance & muscle coordination)
Brainstem - Low extension of the brain where it connects to the spinal cord. Most of the cranial nerves come from the brainstem. Controls neurological functions necessary for survival (breathing, digestion, heart rate, blood pressure) and for arousal (being awake and alert). The pons and medulla are portions of the brainstem.
Ventricles of the Brain - Structures containing cerebrospinal fluid (CSF), which bathes and cushions the brain and spinal cord. Ventricles are continuous with the central canal of the spinal cord.
Meninges - a series of tough membranes that cover the brain and spinal cord
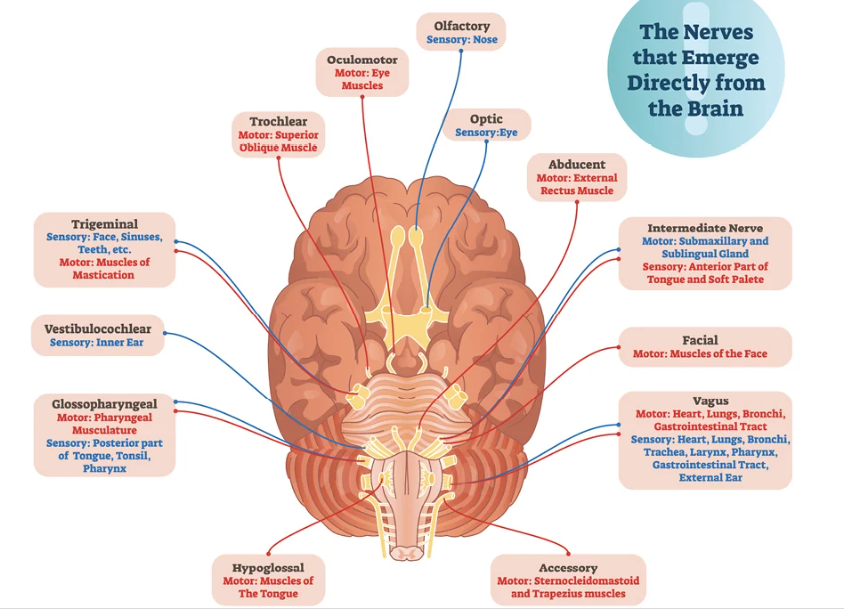
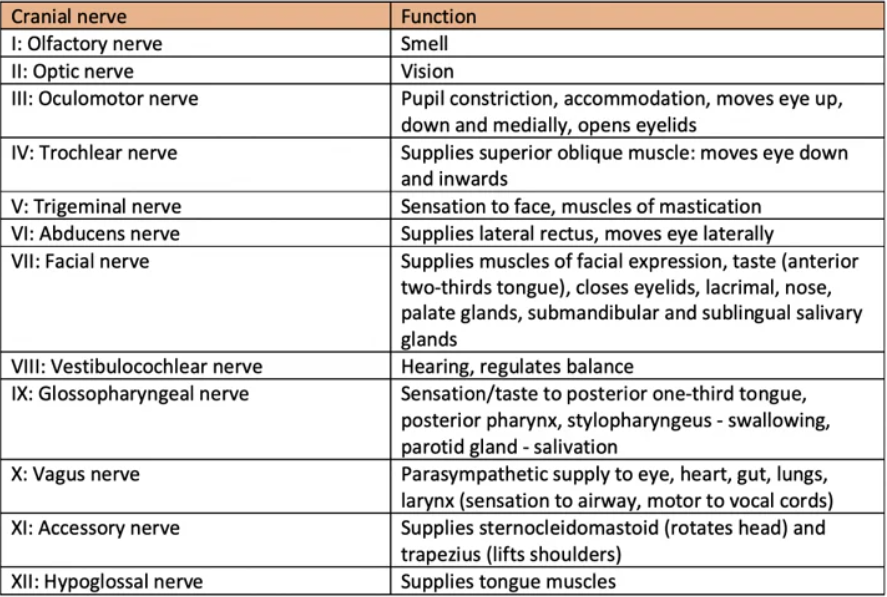
Cranial Nerves:
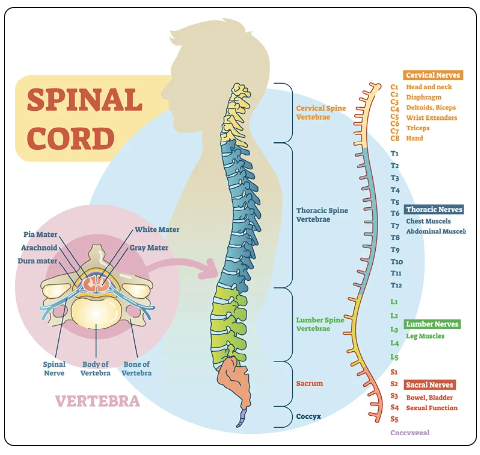
Spinal Cord - a bundle of nerves that extends from the base of the brain (medulla oblongata) downward, to the space between the first and second lumbar vertebrae (conus medullaris)
Lies within the vertebral column and is protected
Cauda Equina - The collection of nerves at the end of the spinal cord
Below the first/second lumbar vertebrae (conus medullaris), spinal nerves continue as the cauda equina
Consists of the 2nd-5th lumbar nerves, 5 sacral nerves, and the coccygeal nerve
Spinal Cord 3 Main Functions:
Serve as a conduit for motor information traveling down the spinal cord to the muscles
Serve as a conduit for sensory information traveling up the spinal cord to the brain
Serve as a center for coordinating reflexes
Spinal Cord Nerve Segments:
Cervical Segments: The spinal cord has 7 cervical segments, which give rise to 8 pairs of cervical nerves. These nerves are responsible for transmitting signals to and from the neck, shoulders, arms, and hands.
Thoracic Segments: There are 12 thoracic segments in the spinal cord, each forming a pair of thoracic nerves. These nerves primarily serve the chest and abdominal muscles.
Lumbar Segments: The spinal cord contains 5 lumbar segments, which form 5 pairs of lumbar nerves. These nerves are crucial for the function of the lower back, hips, and legs.
Sacral Segments: There are 5 sacral segments in the spinal cord, each giving rise to a pair of sacral nerves. These nerves are involved in the function of the pelvic organs and lower limbs.
Coccygeal Segments: The spinal cord has 3 to 5 coccygeal vertebral segments that fuse to form the coccyx (tailbone). These segments give rise to one pair of coccygeal nerves, which have a minor role in the sensory and motor functions of the pelvic region.
C1-C7 Spinal Nerves: These spinal nerves emerge above their corresponding vertebrae. For instance, the C1 nerve emerges above the C1 vertebra, the C2 nerve above the C2 vertebra, and so on until C7.
C8 Spinal Nerve and Below: Starting from the C8 nerve, which does not have a corresponding C8 vertebra, the spinal nerves emerge below their corresponding vertebrae. So, the C8 nerve emerges below the C7 vertebra. From there, T1 nerve emerges below the T1 vertebra, T2 below T2, and so forth down the spine.
Vertebral Segment: This refers to one vertebral bone along with its associated structures like articular processes and laminae. It’s essentially one of the building blocks of the spine.
Vertebral Interspace: This is the space between two adjacent vertebral bodies. It contains the intervertebral disc, which is composed of:
Nucleus Pulposus: The soft, gel-like center of the intervertebral disc that absorbs shock.
Annulus Fibrosus: The tough, outer layer of the disc that provides structure.
Cartilaginous Endplates: The layers of cartilage that attach the disc to the vertebrae above and below.
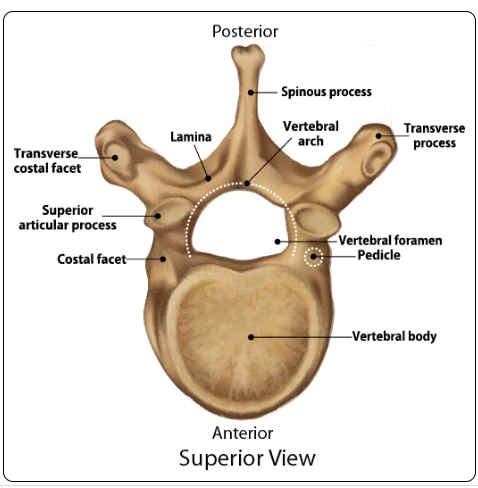
Vertebra:
Corpus - The body and main portion of the vertebra
Vertebral Foramen - The passageway of the vertebral segments, where the spinal cord passes through
Spinous Process - Posterior projection of the vertebra
Transverse Processes - Projections on either side of the vertebra
Lamina/Laminae - are small ridged areas midway between the spinous process, the transverse process, and the vertebral arch
Laminectomy - Complete excision of the laminae, in addition to the entire posterior portion of the vertebra
Laminotomy - partial excision of one or more lamina
Facet Joints - Paravertebral facet joints, z-joints, or zygapophyseal
Located on the posterior spine on each side of the vertebrae where it overlaps the neighboring vertebrae
Provides stability
Gives spine ability to bend and twist
Made up of 2 surfaces of the adjacent vertebrae that are separated by a thin layer of cartilage
Often the site of diagnostic or therapeutic injection (pain relief)
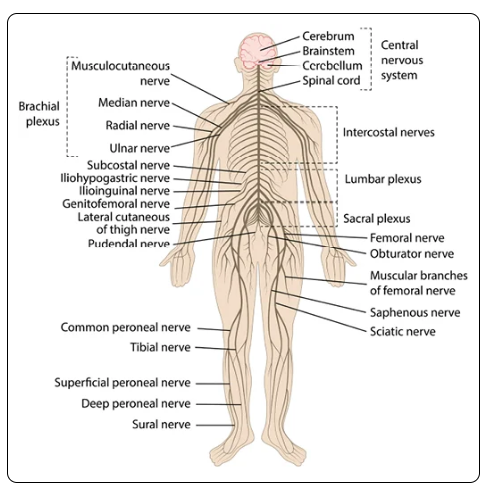
PNS - Peripheral Nervous System:
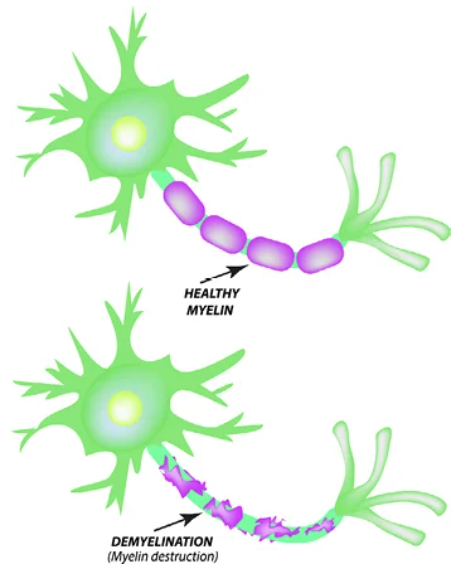
Myelination - The axon is coated with a myelin sheath (layer of fatty cells - Schwann cells), acting as insulation. Most nerves in the PNS are myelinated.
If the myelin sheath were not present, nerve impulses could generate unwanted responses in nearby neurons. Ex. Muscle contractions, jerky, irregular movements
Myelin sheath damage (MS) people have difficulty with muscle control
Nodes of Ranvier - Gaps in the myelin sheath at regular intervals along the axon. Allows faster transmission of nerve impulses.
Nerve Plexus - network of intersecting nerves that combine spinal nerves in the same body area. There are several nerve plexuses in the body:
Cervical plexus - Serves the head, neck, and shoulders
Brachial Plexus - Serves the chest, shoulders, arms and hands
Lumbar Plexus - Serves the back, abdomen, groin, thighs, knees, and calves
Sacral Plexus - Serves the pelvis, buttocks, genitals, thighs, calves, and feet
Lumbosacral Plexus - Sometimes the lumbar and sacral plexuses are interconnected
Solar or celiac plexus - Serves the internal organs
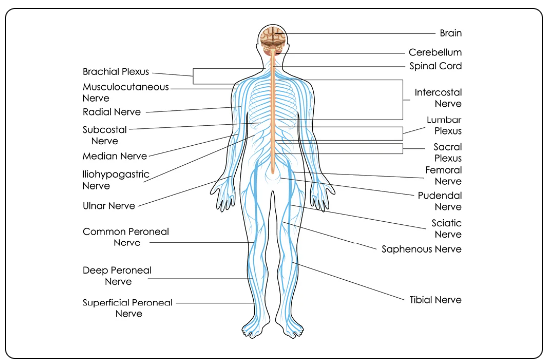
Major Nerves:
Femoral Nerve - Sensory (afferent - toward the CNS) and motor (efferent - away from the CNS) nerve supplying the front of the thigh and part of the lower leg
Common Fibular Nerve (Common Peroneal) - Sensory and motor nerve supplying the knee and superior tibiofibular joints and tibialis anterior muscle
Divides into superficial and deep fiburlar (peroneal) nerves
The fibular nerves (also known as the peroneal nerves) are branches of the sciatic nerve that serve various functions in the lower leg and foot. They are divided into two main branches:
Superficial Fibular (Peroneal) Nerve:
This nerve innervates the muscles in the lateral compartment of the leg, which are responsible for foot eversion (turning the foot outward).
It also provides sensory innervation to the skin on the dorsum (top) of the foot and part of the lower leg.
Deep Fibular (Peroneal) Nerve:
This nerve innervates the muscles in the anterior compartment of the leg, which control dorsiflexion (lifting the foot upward) and toe extension.
It provides sensory innervation to the skin between the first and second toes on the dorsum of the foot.
These nerves are crucial for both motor and sensory functions of the lower leg and foot. They help in movements such as walking, running, and balancing.
Intercostal Nerves - The upper thoracic nerves innervate primarily the chest and upper abdomen; the only nerves not originating from a plexus
Median Nerve - provides nerve supply to most flexor muscles of the forearm and provides sensation for the thumb, index, middle fingers, and a portion of the ring finger. It is the only nerve passing through the carpal tunnel
Musculocutaneous nerve - Sensory and motor nerve of the coracobrachialis, biceps brachii, and the greater part of the brachialis (bicep and side of forearm) - arises from the brachial plexus
Radial Nerve - provides nerve supply to the triceps brachii muscle of the arm and all 12 muscles in the posterior osteofascial compartment of the forearm
Saphenous Nerve - sensory nerve of the knee joint, subsartorial, and patellar plexuses, and the skin on the medial side of the leg and foot
Sciatic Nerve - The larges nerve of the body. From spinal nerves L4 through S3, runs through the buttock and down the lower limb.
Supplies the skin of the leg and the muscles of the back of the thigh.
Divides just above the knee into the tibial and common fibular (Common Peroneal) nerves
Subcoastal Nerves - Sensory and motor nerves of the skin of lower abdomen and lateral side of gluteal region, and parts of abdominal transverse, oblique, and rectus muscles.
Tibial Nerve - Sensory and motor nerve, supplies the muscles and skin of the knee, calf, and sole of the foot, and the toes.
A branch of the sciatic nerve
Ulnar Nerve - Provides sensation for the little finger and a portion of the ring finger and innervates some muscles of the hand and forearm.
COMMON CONDITIONS:
Nervous System -
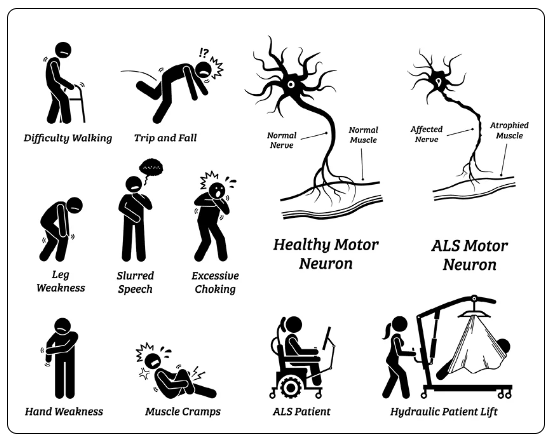
Amyotrophic lateral sclerosis (ALS) - aka Lou Gehrig's disease. A progressive neurodegenerative disease that affects motor nerve cells in the brain (upper motor neurons) and spinal cord (lower motor neurons) - causing loss of motor control.
Most common degenerative disease of the neuromuscular system
As motor nerve cells die, the ability of the brain to initiate and control muscle movement is lost. Because motor nerves are no longer sending impulses to the muscles, they waste away (atrophy), causing increased muscle weakness
Usually begins with muscle twitching and weakness in an extremity
Does not impair a person's intellectual reasoning, mental abilities, memory, vision, hearing, or sense of taste, smell or touch.
Doesn't affect sexual, bowel, or bladder functions
Symptoms usually occur unilaterally (asymmetrical) in hands, limbs, or feet, and spreads
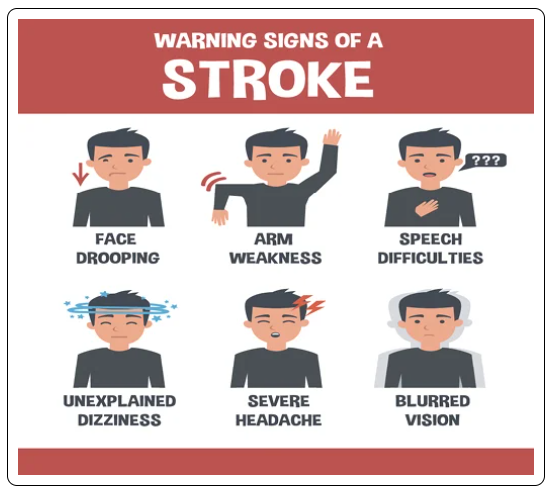
Cerebrovascular Accident/Stroke (CVA) - Occurs when the tissue in the brain is deprived of oxygen due to an interruption or reduction in the blood supply to the brain
Ischemic Strokes - 87% of strokes. Caused by an abrupt blockage of arteries that supply oxygen rich blood to the brain
Occur abruptly and require immediate attention
Transient Ischemic Attack (TIA) - Mini stroke. When the symptoms of a stroke last only a short time (mins-24 hours) and resolve without causing any permanent damage
Hemorrhagic Strokes - caused by bleeding into the brain when a cerebral artery leaks or ruptures. Blood flow to the brain is interrupted and the brain cells are damaged due to increased pressure from the blood seeping into and around the brain tissue
Hemiplegia - complete paralysis to one side of the body is a common result
Hemiparesis - One sided weakness is a common result
Risk Factors - Hypertension, atherosclerosis (plaque in the blood vessels), heart disease, diabetes, high cholesterol, and smoking.
Epilepsy - Abnormal electrical activity within the brain and cause seizures.
During a seizure, many neurons fire at the same time, much faster than usual. This surge may briefly affect a person's movements, sensations, emotions, and behaviors, and the temporary disturbance or normal neuronal activity may cause decreased awareness or loss of consciousness.
Ongoing/uncontrolled seizures may cause brain damage
Brain's electrical rhythms tend to become imbalanced.
Seizures occur when the normal pattern of nerve cell activity is disrupted by sudden and synchronized bursts of electrical energy from clusters of neurons in the brain, causing repeated seizures.
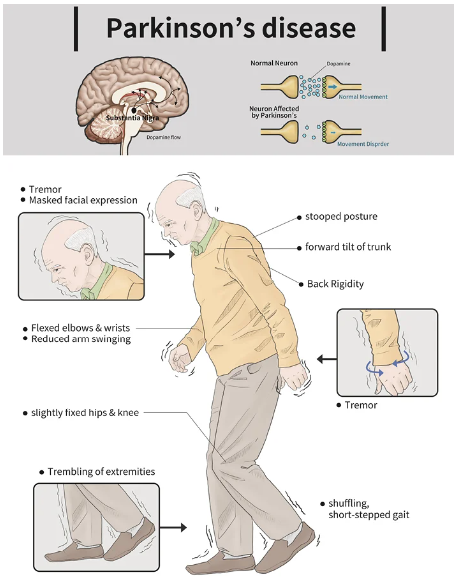
Parkinson's Disease (PD) - chronic neurodegenerative disorder that gradually strips away motor abilities, leaving people with a slow and awkward gait, rigid limbs, trembling of the extremities and head while at rest, and lack of balance.
Starts slow, worsens over time
Cause unknown. Likely due to a complex interaction between genetic and environmental factors
Occurs when the cells in the area of the brain called the substantia nigra stop working or die off. These brain cells manufacture dopamine, a neurotransmitter that helps control and coordinate muscle movement.
Most common movement disorder - progressive loss of muscle control with leads to motor symptoms
Tremors (rhythmic shaking)
Muscle stiffness or rigidity
Slowness of movement (bradykinesia)
Difficult to walk, talk, complete simple tasks
Mental Health:
Anxiety - Causes feelings of uneasiness and fear. Can manifest physical symptoms such as racing heart, sweating, or restlessness.
Treatment: mental health therapy, medication, or a combo of both
Depression - mood disorder that causes persistent and intense feelings of hopelessness, sadness, and loss of interest for extended periods of time.
MDD (Major depressive disorder) can lead to a variety of emotional and physical problems, making it difficult to work, study sleep, eat, and enjoy friends and activities. Normal day to day feel like life isn't worth living.
Treatment: mental health therapy, medication, or a combo of both
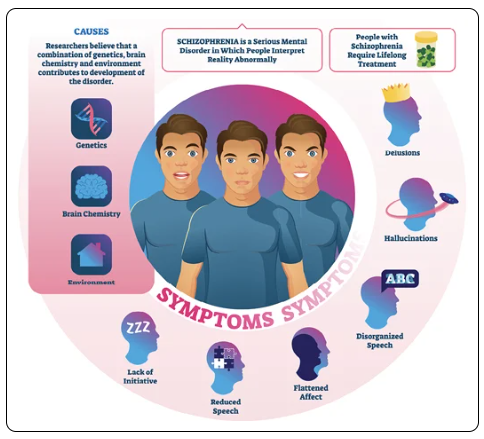
Schizophrenia - a severe chronic psychiatric disorder. A psychosis where a person cannot tell what is real from what is imagined. Sometimes losing touch with reality. May seem like a hodge-podge of confusing thoughts, images, and sounds.
Complex condition that interferes with a person's ability to think clearly, manage emotions and behaviors, make decisions, and relate to others
Symptoms: Hallucinations, delusions, disorganized speech and behavior
Treatment: Ongoing and lifelong. Therapy, medications, or a combo.
Substance Use Disorders (SUD) - Drug addiction. A disease that affects a person's brain and behavior and leads to an inability to control the use of a legal or illegal drug or medication.
AOD - Alcohol and other drugs
A pattern of using a substance that leads to problems or distress such as failure to fulfill responsibilities at work, home, school, and/or repeated using the substance in situations in which it is physically hazardous.
Illegal - Ex. Meth, cocaine, heroin
Legal - Ex. Alcohol, nicotine, prescription drugs
Individuals often rely on a substance to feel good or to cope with everyday life and are unable to moderate or quite, no matter the consequence.
Body becomes dependent on the chemicals released by each substance and begins craving more.
Treatment: Therapy and medication
COMMON PROCEDURES:
Skull, Meninges, and Brain -
Skull - bony protection surrounding the brain and is made up of 22 bones
Facial Bones - 14 bones form the face and jaw
Cranial bones - 8 bones protect the brain
Fontanel - space covered by tough membranes between the bones of an infant's cranium; has yet to close. 2 cranial fontanels in the infant skull
Posterior Fontanel - between occipital and 2 parietal bones
Anterior Fontanel - between the frontal and 2 parietal bones
Posterolateral Fontanel (mastoid) - between the temporal bone and the mastoid process
Anterolateral (sphenoid) - between the temporal, parietal, and frontal bones
Meninges -
Hematoma - localized collection of blood that has usually clotted.
Found in organs, spaces, or tissues, and are the results of a break in the wall of blood vessels
Subdural hematoma - leakages of blood between the dura and arachnoid membranes
Must be drained. Allowing them to expand unchecked can result in displaced brain tissue (under pressure), resulting in anoxia or death to those tissues and eventual death to the individual
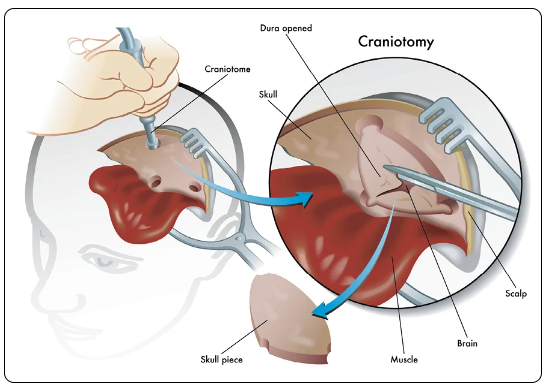
Craniotomy - Bony opening cut into the skull. A section of skull, called a bone flap, is removed to access the brain underneath and subsequently replaced
Labeled by the part of the skull opened (Ex. Frontal craniotomy indicates the opening is in the frontal bone)
If 2 parts of adjacent bones are opened, both bones are mentioned (Ex. Frontotemporal craniotomy)
Craniectomy - Bony opening cut into the skull where a bone flap is removed to access the brain and not replaced
Suboccipital Craniectomy - surgery on the back of the brain beneath the tentorium, removal of the lower part of the occipital bone
Retromastoid Craniectomy - bone removal is more to the side, just behind the mastoid bone
Burr Holes - series of small holes made into the skull, which is cut between each adjacent burr hole until the bone flap is separate from the surrounding skull
Lesions - The dura is under the skull. Surgeon will cut the dura to access lesion. If meningioma is attached to the dura, the surgeon may cut the dura around the tumor to leave a margin of normal dura
Loss of dura, substitutes can be used:
Bovine Pericardium (covering of the heart)
Banked human Dura
GORE-TEX plastic
Absorbable collagen matrix
The surgeon may wish to line the cavity left by removal of the tumor, with an absorbable wafer impregnated with an anticancer drug. Has been shown to extend life.
Pituitary Tumor - can cause a patient to develop visual field defects, absent menstrual cycles, infertility, decreased libido, impotence, decreased body hair, and decreased production of other stimulating hormones.
Usually in anterior lobe and are benign, small, and encapsulated.
Often can be successfully removed by surgery call a transsphenoidal hypophysectomy - performed through the nose
Temporal Lobectomy, extratemporal lobectomy, hemispherectomy, corpus callosotomy - surgeries that can be used to reduce seizures by removal of that part of the brain
Vagus Nerve Stimulator (VNS) can be sued to reduce seizure frequency
Cerebrospinal Fluid (CSF) Shunt - Placement of an extracranial shunt, or tube, to divert excess CSF from the ventricles of the brain to another body area (most often the abdominal cavity
The standard treatment for hydrocephalus (an accumulation of CSF).
Intracranial shunts are created by means of ventriculocisternostomy or ventriculocisternal shunting
Torkildsen Type - technique that involves performance of a ventriculocisternostomy to form communication between the lateral ventricles and the cisterna magna
Drains CSF into the subarachnoid space, especially the cisterna magna where fluids will be absorbed
Burr holes drilled. Shunt inserted toward the lateral ventricle until the CSF flows through the shunt. The distal end of the shunt is directed toward the cisterna magna. The two ends are connected and tested. The dura is sutured closed and the scalp is reapproximated and closed in sutured layers.
Endoscopic third ventriculostomy - uses a laser under neuroedoscopic guidance to create a duct from the third lateral ventricle to the cisterna magna without need for a shunt.
Extracranial shunts may require periodic revisions, including irrigation and a complete or partial replacement
Reprogrammable Shunt - allows noninvasive pressure adjustments to correct over or under drainage of CSF
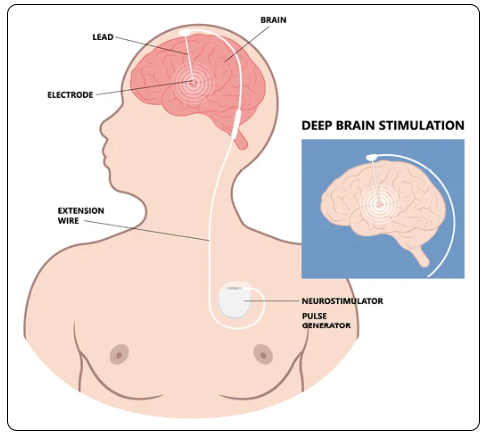
Neurostimulators (Brain) -
Neurostimulator pulse generator system - is surgically implanted, pacemaker like device delivering pre-programmed intermittent electrical pulses to a nerve or brain structure
Treat conditions not responding to medication alone, including intractable pain in the trunk, limbs, peripheral neuropathy, Parkinson's disease, epileptic seizures and others
Access by burr hole, craniectomy, craniotomy, etc
Deep Brain Simulation (DBS) - high frequency electrical stimulation of anatomic regions deep within the brain using neurosurgically-implanted electrodes. Stereotactically placed within targeted nuclei on one (unilateral) or both (bilateral) sides of the brain.
Three targets for DBS:
Thalamic Ventralis Intermedius Nucleus (VIM)
Subthalamic Nucleus (STN)
Globus Pallidus Interna (GPI)
Electroencephalography (EEG) - a test to measure electrical activity in your brain, recording any abnormalities in the brain waves.
Used to diagnose brain disorders like epilepsy or sleeping disorders
Routine EEG - 20-40 minutes of recording
Special EEG - 40minutes to hours of recording
Certain EEG codes are appropriate if both an awake and asleep study was intended, even if the patient did not sleep
Certain EEG codes are appropriate if an awake only study
Certain EEG codes are reported based on the person who performed the EEG
Codes are also based on whether the EEG is performed with video and the type of monitoring and maintenance performed.
Some codes have a time requirement
Spine & Spinal Cord :
Injection, Drainage, or Aspiration -
Epidural lysis of spinal adhesions - surgeon inserts a needle near the patient's tailbone and threads a catheter through the needle to inject medication into adhesions.
The needle may be removed after the procedure, but the catheter may remain in place for several days to continue treating the lesions.
Percutaneous Aspiration - procedure where the surgeon removes contents of a cyst or syrinx (a fistula or diseased area) with a needle.
Using a C-arm X-ray machine to verify placement of the needle, the surgeon aspirates the cyst or syrinx of its contents and removes the needle.
Often used to treat intraspinal-abscess, syringomyelia, and other disorders of the meninges
Injections of Neurolytic Substances - Alcohol, phenol, iced saline solution can be given to destroy nerve tissues or adhesions
Non-neurolytic substances - anesthetic, antispasmodic, opioid, steroid, etc can be given to control pain and/or muscle spasms
Epidural Injection (Continuous) - catheter placement involves using a special needle called a Touhy needle that's inserted between the vertebrae into the epidural space
Epidural space is between the endosteum of the spinal column and dural membrane, needs does not puncture the dura
Small catheter is threaded through the needle into the epidural space and the needle is withdrawn.
Catheter is taped in place to prevent movement and the anesthetic agent is injected or infused through the catheter
Laminotomy - the removal of a small pieces of the vertebra through a hole in the lamina
Laminectomy - more involved procedure where most of the bone is removed.
Surgical procedures that are performed to relieve back pain caused by pressure on the spinal cord or spinal nerves.
Relieve pressure by removing the portion of the vertebra that is causing the pressure
Procedures are grouped according to spinal region (cervical, thoracic, and lumbar)
Spinal Neurostimulators - Electrodes implanted along the spine, which are connected to a programmable pulse generator or receiver.
Electrodes may be either a catheter electrode array or arranged on a paddle
Treat chronic back pain by delivering low voltage electrical stimulation to the dorsal columns of the spinal cord to block the sensation of pain
Shunt, Spinal CSF - Shunt inserted through the dura into the subarachnoid space and passed around the flank to the peritoneal, pleural, or other space for drainage
Used to allow excess CSF to be drained for Hydrocephalus condition