Anti-cancer agents
Summary cancer
Cytotoxic chemotherapy
- These include most of the anticancer drugs
- There are four types: Antimetabolites, plant derivatives, alkylating agents and antineoplastic antibiotics.
- Two of them are cell cycle dependent: Antimetabolites and plant derivatives.
- Two of them are cell cycle independent: Alkylating agents and antineoplastic antibiotics. Both of these induce DNA damage of some sort,
Antimetabolites
- These are drugs which inhibit DNA or RNA synthesis and are cell cycle dependent: requires replicating cells.
- Often used to treat leukemia, breast cancers, ovary and GIT cancer etc.
Fluorouracil
- which is a pyrimidine analog.
- Fluorouracil, also called 5-FU, act as a thymidylate synthase (TS) inhibitor. It interrupts the action of TS, which therefore blocks the synthesis of thymidine. Therefore it inhibits DNA synthesis.
Methotrexate
- A folic acid analog
- Inhibits dihydrofolate reductase (DHFR), an enzyme which is important for tetrahydrofolate synthesis.
Plant derivatives
- Are drugs which inhibit mitosis, by inhibiting microtubule or topoisomerase.
- They are cell cycle dependent: requires replicating cells.
Vincristine
- Vinca alkaloid
- Causes mitotic arrest in the metaphase, due to inhibiting microtubules.
- Treat acute leukemia etc
- SE: Peripheral neuropathy, suppression of bone marrow activity, nausea, vomiting :)
Campothecins
- Inhbits topoisomerase I, which causes dsDNA breaks.
Alkylating agents
- Very broad spectrum, used for e.g. lymphoma, sarcoma, cancers of the lung
- Are not dependent on cell cycle
- Alkylation = transfer of an alkyl group from one molecule to another
- They’re causing systemic toxicity and are carcinogenic :)
- The main MoAs:
- Depurination → DNA strand breakage
- ds rxn → Crosslinking DNA
- Mismatching of DNA bases → miscoding
Cisplatin
- Is used for testicular cancer, but also lung, bladder, cervical.
- It contains platinum (but no alkyl group)
- Causes interstrand crosslinks, causing base pairs to bind to different pairs of the double helix → apoptosis
- Will kill the cells in all stages of the cell cycle
Anti-neoplastic antibiotics
- Are DNA damaging agents
- Used in many cancers, e.g. leukemias, lymphomas, breast, stomach etc
- interrelate between specific DNA because which:
- Block synthesis of RNA, DNA or both
- Cause DNA strand scission (breaks the chemical bond)
- Interfere with cell replication
Doxorubicin
- A type of anthracycline
- Amongst the widely-used cytotoxic chemotherapies
- It has four MoAs:
- Inhibits topoisomerase II
- intercalate into DNA which will block DNA & RNA synthesis, as well as causing DNA strand scission
- Generate free radicals
- Bind to cell membranes to alter fluidity and ion transport
Hormonal
- Hormones can drive cancer
- There are many tumours which arise in hormone-sensitive tissues, e.g. breast, ovarian, endometrial, prostate and testicular cancers
Hormone treatments for cancers of the reproductive system
Hormones can be used to treat some cancers…
- Glucocorticoid (cortisol) is a steroid hormone which has anti-inflammatory effects. Synthetic cortisol might lessen some of the side-effects from anti cancer drugs, e.g. nasea, vomiting, pain.
- Oestrogen can palliatively be used as treatment of androgen-dependent prostatic tumours, due to it’s negative feedback inhibition of Gonadotropin releasing hormone (GnRH) secretion from hypothalamus.
- Progestogens can be used for advanced endometrial cancer, due to inhibiting endometrial cell growth and causing cell differentions.
Hormone antagonists
Even though hormones can be used to treat cancers, we more often see them as drivers of cancers. Therefore, there are a lot of inhibitors of hormones which are used as anti-cancer treatment.
→ It’s important to know that hormones do not cause cancer, but only drive it. This is because the hormones often have proliferative effects on certain types of cells.
- Anti-oestrogens and aromatase inhibitors are used to treat breast cancer
- Anti-androgens are used for testicular cancer
Anti-oestrogens (SERMS)
SERMs are Selective oestrogen receptor modulators. One examples is:
Tamoxifen.
- It blocks actions of oestrogen in breast tissue, and therefore inhibits the growth of breast cancer.
- It upregulates TGF-beta
- It is a partial agonist / partial antagonist depending on the type of eostrogen receptor: ERalpha gives an enhanced proliferation effect, whereas ERbeta has an antiproliferative effect.
Aromatase inhibitors
- Examples are: Anastrozole, letrozole, exemestane.
- They inhibit the conversion of androgens into oestrogen in the adrenal cortex (but not in the ovary).
- This is because post-menopausal women has their main source of oestrogens in the adrenal cortex; It’ll therefore be the therapy of choice of breast cancer in postmenopausal women.
- However, this has significant adverse effects on bone.
Anti-androgens
- Anti-androgen therapy is used when:
- Patients are unable to have prostate-cancer-treating surgery (which is the primary therapy
- Before radiation to try to shrink the cancer (neo-adjuvant therapy)
- Together with radiation therapy as an initial treatment if the patient is at higher risk of cancer coming back after therapy
- If the cancer ramins of comes back after therapy
Enzalutamide
- It acts at three key stages of AR signalling pathway:
- Inhibits androgen binding to the androgen receptors
- It also inhibits nuclear translocation of the hormone/androgen receptor complex
- Aaaaand it also inhibits binding of the hormone/androgen receptor complex to DNA!
Monoclonal antibodies (mAbs)
Immunotherapy - is a way to boost the body’s immune defences to fight cancer. This is done by using substances made by the body (or in a lab) to improve or restore immune system function. It can work by:
- Stopping or slowing the growth of cancer cells. These attach themselves to cancer cells, which will make it easier for the immune system to find the cancer cells.
- Helping the immune system work better at destroying cancer cells, e.g. by blocking molecules which hinder the immune system.
- Leave the healthy cells in the body intact: which will minimize side effects during treatment.
There are seven strategies behind Monoclonal antibodies based cancer therapeutics:
- Tumour-specific IgG. In which IgG-Ab binds to antigens specific to the tumour. These mediate antibody-dependent cellular cytotoxicity (ADCC) by immune effector cells.
- Angiogenesis inhibition - In which IgG bind to VEGF, which then won’t bind to VEGFR and there will therefore not be any angiogenesis.
- Checkpoint blockade in which IgG activates the immune system by targeting CTLA4, a receptor which downregulates the immune system. Example: Ipilimumab.
- Radioimmunotherapy in which immunoconjugates (ab + radioactive) which binds to the tumour to try to target that site and kill it with radioactivity!
- Antibody-drug conjugate therapy in which a tumour-specific antibody is bound with the cytotoxic drug, in order to try and deliver the drug on site to poison the tumour.
- Bispecific antibody therapy where the antibody binds to the tumour and CD3 on T-cells → which leads to t-cell activation and tumour cell killing!
- CAR T Cells (Chimeric antigen receptor), which mediate MHC-unrestricted tumour cell killing by enabling T cells to bind target cell surface antigens.
Trastuzumab
Is a cancer drug which inhibits growth factor receptor-ligand signalling pathways.
- MoA: It attaches to the oncogenic protein HER2 (human epidermal growth factor receptor 2). When growth factors bind to HER2 it initiatives cell growth and division. However, when the Trastuzumab binds to the receptor, this blocks it the growth factor signals → which will lead to apoptosis
- This will also inform the immune system that something is wrong, and the immune system will attack the cancer cell.
- The HER2 dimers will become endocytosed (which will lead to no growth)
- Clinical use: Used for cancer which over-express HER2. Many of these are breast cancers (25-30% of the breast cancers).
- It has been shown to increase 5-year survival rate in patients with agressive breast cancer.
- The drug is often given with taxane.
Bevacizumab
- Is a humanised monoclonal antibody
- Type b. - angiogenesis inhibition
- Clinical use: Is used for therapy of colorectal cancer - however it is expected to be useful for treating other cancers as well.
- MoA: The antibody neutralises VEGF, and therefore prevents angiogenesis which is crucial for tumour survival.
- Administration: IV infusion and is generally combined with other agents.
- Side effects: Hypertension, bleeding and thrombosis.
Cancer chemoprevention
Chemoprevention is the use of synthetic, natural or biological agents to suppress and prevent carcinogenic progression. These work by blocking DNA damage which initiate carcinogenesis, or arresting/reversing the progression of premalignant cells in which the damage has already occurred.
It may delay cancer, however you might still develop cancer in the future :(
Mechanisms of action of tumour-blocking agents
- Scavenging of free radicals
- Antioxidant activity
- Induction of phase II drug-matbolising enzymes
- Inhibition of phase I drug-metabolising enzymes
- Induction of DNA repair
- Blockade of carcinogen uptake
Mechanisms of tumour suppressing agents
- Alteration in gene expression
- Inhibition of cell proliferation, clonal expansion
- Induction of terminal differentiation, senescene
- Induction of apoptosis in preneoplastic lesions
- Modulation of signal transduction
Tamoxifen
- Is the oestrogen receptor inhibitor.
- It competitively inhibits the binding of estradiol ot estrogen receptors. It decreases DNA synthesis and therefore cellular response to estrogen.
- It increases the production of TGFb (which inhibits tumour cell growth) and decreases the production of IGF-1 (which stimulates tumour cell growth).
- Is used to prevent breast cancer
Raloxifene
- It acts as an oestrogen antagonist in uterine and breast tissue.
- It also lowers total and LDL cholesterol levels by functioning as an oestrogen agonist in lipid metabolism.
- It is given to postmenopausal women which have a high risk for developing breast cancer, or who have osteroporosis.
- It has activity against osteoporosis because it decreases bone resoption and bone turnover and increases bone mineral density.
NSAIDs
- COX-2 selective nonsteroidal antiinflammatory drug
- Example: Aspirin.
- NSAIDs blocks the conversion of arachidonic acid into prostaglandins. Prostaglandins are involved in inflammation and pain, but also in cell proliferation, angiogenesis, invasion and metastasis.
- NSAID-mediated activities will result in apoptosis, dimins cell proliferation and might block epithelial-to-mesenchymal transitions.
Dietary / metabolic factors
- Decrease risk: high fibre diet, nutrients (e.g. vitamins & minerals) in fruit and vegetables, high fish consumption
- Increase risk: high intake of red or processed meat or alcohol, too much salt and a diet high in saturated fat 🙁
- Phytochemicals are found to detoxificate carcinogens. They can interfere with different steps of carcinogenesis, e.g. inhibit metabolic activation by blocking tumour initiation, or stimulate detoxification of carcinogens.
- Examples are: garlic, ginger, chili peppers, turmeric, grapes, honey, tomatoes, broccoli.
- Selenium has been found to be good.
Cancer vaccines
- The vaccination against Human Papillomaavirus (HPV) is one of the most successful vaccinations against a cancer, in this case cervical cancer.
- The vaccine prevents infection by certain types of human papilloma viruses.
Targeted chemotherapies
Target therapies is a way in which we try to focus on a specific target in the cancer to make sure that we only e.g. kill the tumour cells. For this we want good targets that are present in the cancer cells but not on other cells. One good example is the HER2 which is what trastuzumab targets.
Protein Kinase Inhibitors (Small Molecule Inhibitors)
- Imatibin mesylate is a type of protein kinase inhibitor which inhibits intracellular BCR-ABL enzyme.
- BCR-ABL enzyme is a tyrosine kinase which is an oncogene, which is creates by fusing the Abl tyrosine kinase gene at chromosome 9 and the break point cluster (bcr) gene at chromosome 22. This BCR-ABL tyrosine kinase then is a continuously active which is found in pathogenesis of chronic myelogenous leukemia.
- It is basically a very specific target for this type of cancer and the Imatibin inhibits this receptor. By doing so it inhibits proliferation and survival.
- → It has improved the prognosis for CML patients!
- There are also few side effects
- However, there has been a rise in resistance, most often caused by reactivation of Bcr-Abl kinase activity :/
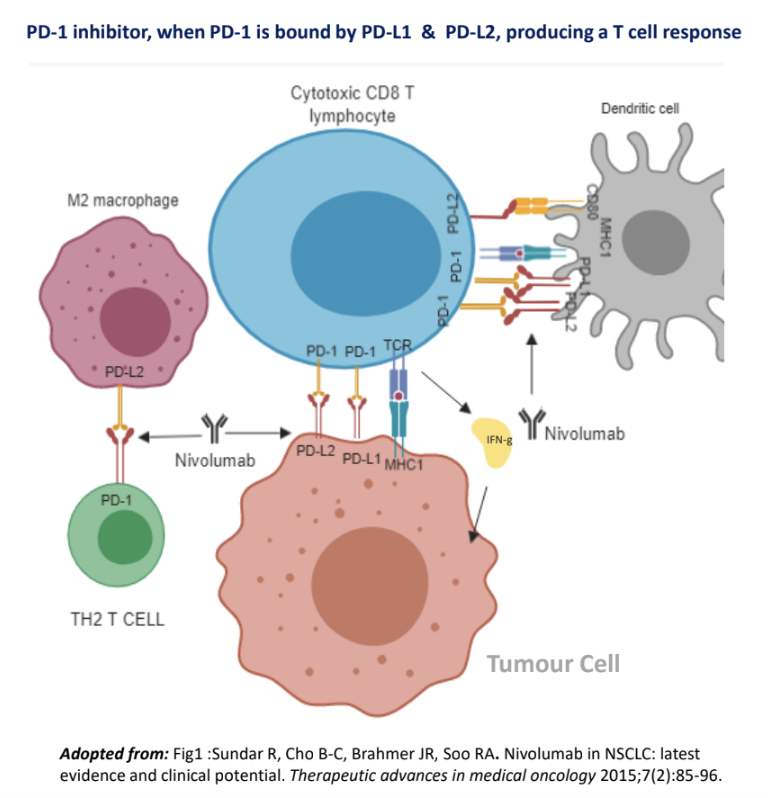
Immune checkpoint inhibitor immunotherapy
Immune checkpoints are important to the immune system. There are certain “brakes” which are there to prevent overly rigorous/lengthy immune responses which will destroy healthy cells. However, this is often used by cancer cells by binding to the immune checkpoint proteins on the surface of T-cells, which then will inhibit the immune response…
- Therefore there are antibody therapies which will block this binding, to reactivate the immune response by restoring T-cell anti-tumour function.
CTLA-4 (Cytotoxic T-leukocyte antigen 4)
- Ipilimumab is a checkpoint inhibitor which inhibits CTLA-4.
- Switching off CTLA-4 will cause the tumour to grow for a while, but then to regress.
- There was an overall extend to survival gain in people with advanced melanoma.
- However, it caused severe autoimmune side effects and some died 😛
Programmed death 1 (PD1)
Nivolumab is a drug which will initate PD1 in cancer cells:
- Programmed death can be induced on tumour cells by Interferon gamma (IFNy).
- This functionally exhausts the tumour fighting t-cells
- It is used for melanoma, non-small-cell lung canver, renal cell carcinoma and cervical cancer.