Depression
major depressive disorder (mdd) criteria
five or more of the following symptoms have been present during the same 2-week period; at least one of the symptoms is either depressed mood (1) or loss of interest or pleasure (2)
depressed mood most of the day, nearly every day
markedly diminished interest or pleasure in all, or almost all activities most of the day, nearly every day
significant weight or appetite change
insomnia or hypersomnia nearly every day
psychomotor retardation or agitation nearly every day
fatigue or loss of energy nearly every day
feelings of worthlessness or excessive guilt nearly every day
diminished ability to think or concentrate nearly every day
recurrent suicidal ideation, plan, or attempt
significant distress or impairment
symptoms not due to substance use or medical problem
symptoms not better explained by another disorder
there has never been a manic or hypomanic episode
NOTE: responses to a significant loss (e.g., bereavement, financial ruin, losses from a natural disaster, a serious medical illness or disability) may include the feelings of intense sadness, rumination about the loss, insomnia, poor appetite, and weight loss noted in Criterion A, which may resemble a depressive episode
although such symptoms may be understandable or considered appropriate to the loss, the presence of a major depressive episode in addition to the normal response to a significant loss should also be carefully considered
this decision inevitably required the exercise of clinical judgment based on the individual’s history and the cultural norms for the expression of distress in the context of loss
impact of depression
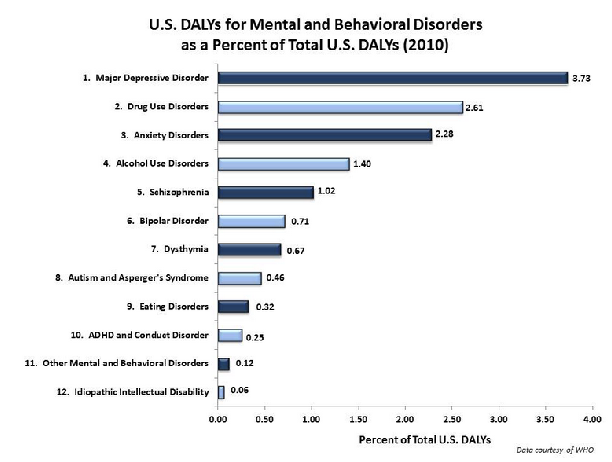
disability-adjusted life years (DALYs)
metric for describing impact/impairment of diseases, disorders, injuries, and conditions
DALY: years of life lost + years lived with disability (lost years of healthy life)
13.6% of DALYs are caused by mental/behavioral disorders
major depression carries the heaviest burden (3.73% of DALYs)
epidemiology
epidemiology: study of distribution, patterns, and determinants of health and disease in populations
lifetime prevalence of MDD
% who meet criteria at some point in lifetime
16.6% (Kessler et al., 2012)
current prevalence of MDD
% currently meeting criteria
7.1% (Kessler et al., 2012)
course and outcome
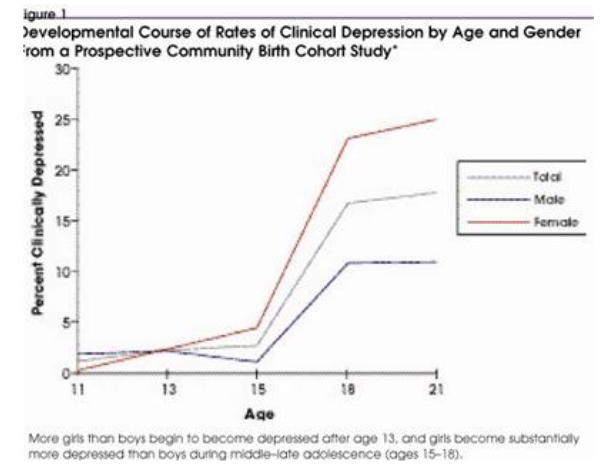
age at onset
average = 24 to 29 years old
earlier onset worsens prognosis
rates increase during adolescence
sex difference in rate first appears in early adolescence, with females being at higher risk than males
number of major depressive episodes
lifetime average = 4
average length = 4.5 months
~25% of people have 6+
etiology of MDD
etiology: the cause, set of causes, or manner of causation of a disease or condition
biopsychosocial model
suggests biological, psychological, and social factors all influence the development of MDD
framework for organizing potential etiological influence on psychopathology
biological influences
genes- abnormal genes (typically in interaction with environment)
neurotransmitter systems- dysregulation of neurotransmitters and receptors
neurophysiology- abnormalities in structure and functioning of brain regions
neuroendocrine system- altered activity in the hypothalamic-pituitary-adrenal (HPA) axis
genetic influences
behavior genetics- study of the degree to which genes and environment influence behavior
doesn’t tell us which genes are responsible
helps establish heritability of mental illnesses
percentage of variation in characteristic that us attributable to genetic influences
depression: 37% -50% (Sullivan et al., 2012)
molecular genetics- study of influence of specific genes and environment on behavior
MDD is polygenic
associated with configuration of several irregular genes, not with single disordered gene
challenges facing molecular genetics- attempts to find specific genes involved in MDD (and other clinical phenomena) plagued by large number of non-replications
genetic influences on mental illness polygenic- associated with configuration of several irregular genes, not with single disordered gene
genes unlikely to lead directly to clinical problems- produce brain, neurochemical, hormonal changes that lead to clinical problems/ interact with environments events to lead to clinical problems
genetic influence are not fixed but unfold and change across development in dynamic interaction with environmental factors
neurotransmitter influences
neurotransmitters: chemicals that facilitate communication across synapses between neurons
released into synaptic gap to bind with receptors on post-synaptic membrane
abnormalities in the number and sensitivity of receptors for monoamine neurotransmitters may be implicated in MDD