Nursing Arts theory test 1
Medical Asepsis
Important Topics:
What is medical asepsis/how is it different than surgical asepsis?
Medical asepsis refers to the practices used to eliminate or reduce microorganisms to prevent infection
surgical asepsis involves complete sterilization of all instruments and surfaces used in invasive procedures.
What is the difference between sterilization and disinfection?
Sterilization destroys all forms of microbial life, including spores,
disinfection only eliminates many, but not necessarily all, pathogenic microorganisms on surfaces or objects.
What are the types of infections for example - Hospital acquired infection?
Colonization
Presence of bacteria on the surface of the body without causing disease in the host
Local Infection
An infection that is in a specific location of the body
Systemic infection
An infection that spreads throughout the entire body and affect it simultaneously, often leading to widespread symptoms and complications.
Bacteremia
The presence of bacteria in the bloodstream
Septicemia
An infection that occurs when the bacteria enter the bloodstream and spreads throughout the body, potentially leading to severe outcomes such as sepsis, which can cause organ failure and even death.
Nosocomial infections (Health care acquired infections)
Endogenous Sources
Pathogens originating from the external environment, such as contaminated surfaces or medical equipment.
Exogenous sources
Pathogens arising from a patient's own body, which can lead to infections if the body's natural barriers are compromised.
Contributing Factors
Environment
Poor hand hygiene
Contaminated hospital equipment
Healthcare workers
Other patients
Chain of infection (what does it consist of and how to break it at each level)
Common pathogens
Bacteria: Microscopic organisms that only have one cell.
Viruses: Small pathogens (germs) that can infect and cause sickness to the host
Fungi: Group of eukaryotic microorganisms which can cause diseases'
Parasites: An organism that gets nutrients by living in another organism of another species
Reservoirs (i.e. source of infection):
Natural habitats where pathogens live and multiply, such as humans, animals, or the environment.
Portal of exit
The pathway through which a pathogen leaves its reservoir, potentially entering a new host through various routes such as respiratory secretions, blood, or bodily fluids.
Mode of transmission:
The means by which a pathogen spreads from one host to another, which can occur via direct contact, airborne transmission, vector-borne transmission, or contaminated surfaces.
Direct, indirect, droplet, airborne, vehicle, vectorborne
Direct Contact Transmission: Physical contact between an infected person and a susceptible person
Indirect Contact Transmission: Spread of infection through contact with contaminated objects or surfaces.
Droplet Transmission: Infections caused by microbes transmitted by droplets produced by coughing, sneezing or talking.
Airborne Transmission: Infections caused by microbes transmitted by airborne droplets
Vector Transmission: Infections transmitted to a human host from animals or insects
Vehicle Transmission: Indirect transmission of an infectious agent to a host through a contaminated source such as food and water.
Portal of entry (what are examples):
Respiratory tract
Gastrointestinal tract
Urinary tract
Skin and mucous membranes
Susceptible hosts (factors affecting susceptibility):
Age: Infants and elderly individuals often have weaker immune responses.
Nutritional status: Malnutrition or obesity can impair immune function.
Chronic diseases: Conditions like diabetes or heart disease can increase susceptibility to infections.
Medications: Immunosuppressive drugs can lower resistance to pathogens.
Stress: Physical or emotional stress may reduce the body's ability to fight off infections.
What are routine precautions?
Routine precautions are actions taken to prevent the transmission of infections and protect both healthcare workers and patients.
These include hand hygiene practices, the use of personal protective equipment (PPE) such as gloves and masks, and ensuring proper cleaning and disinfection of surfaces and equipment.
Handwashing – technique and importance of, when should it occur, when is it appropriate to use hand sanitizer?
Documentation
Why we do it – i.e. purposes/relevance of charting
To ensure accurate patient information is available for healthcare providers
To provide a legal record of care given and decisions made
To facilitate communication among healthcare team members
To support continuity of care and patient safety.
Difference between subjective and objective data
Subjective data:
Information reported by the patient, such as symptoms or feelings that cannot be directly observed or measured, and are influenced by personal perceptions and experiences.
Objective data:
Information obtained through measurements, observations, or physical examinations that can be quantified, verified, and are independent of personal feelings.
How do you correct errors
Errors in data collection can be corrected by verifying the information with the patient, re-evaluating measurements, or consulting additional sources of data to ensure accuracy and reliability.
It is also essential to document any corrections made and to communicate changes with the healthcare team to maintain continuity in patient care.
Confidentiality
all records are securely managed and only accessible to authorized personnel.
it's important to provide training opportunities for staff to understand the importance of accurate data collection and the methods for correcting errors effectively.
Legal obligations
Nurses must adhere to local laws and regulations regarding patient confidentiality and data protection to ensure ethical practice and avoid legal repercussions.
This includes understanding the implications of the Health Insurance Portability and Accountability Act (HIPAA) and similar regulations that govern the handling of sensitive information.
General guidelines
include obtaining informed consent before sharing patient information, regularly updating training on privacy practices, and ensuring secure methods of communication to safeguard patient data.
Additionally, nurses should routinely assess their compliance with these regulations and participate in ongoing education to stay informed about any changes in laws that may affect patient care.
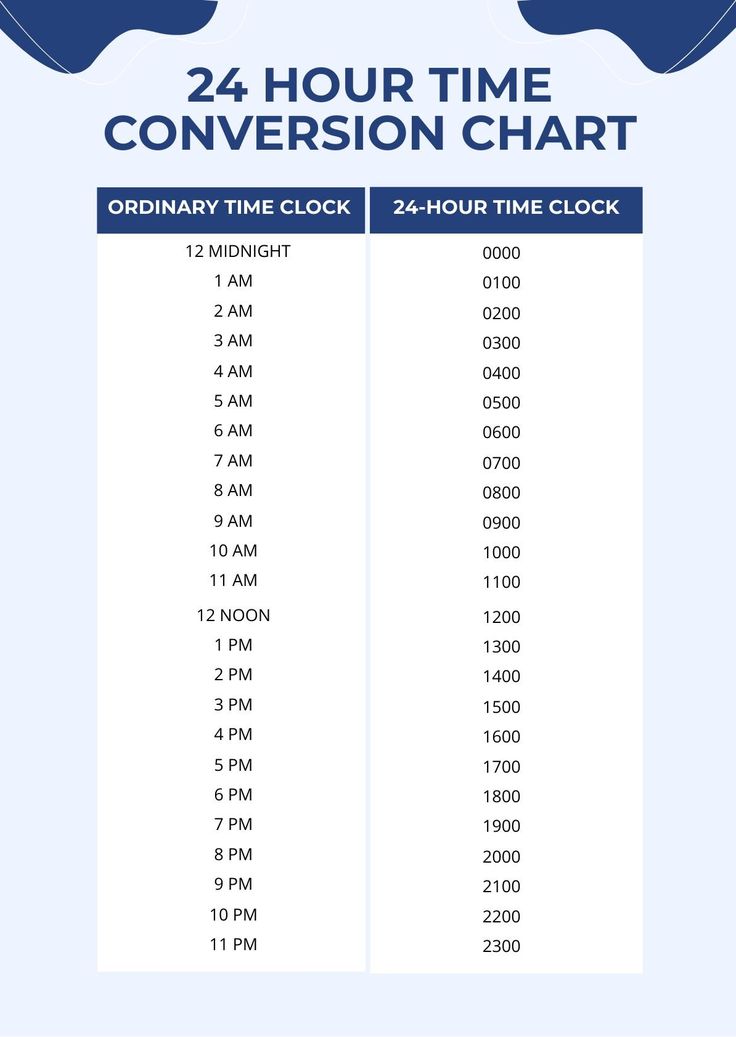
24-hour clock
becomes essential in scheduling patient care and medication administration, enabling accurate time management and ensuring timely responses to patient needs.
Nutrition
Prescribed and therapeutic diets (the different types, what types of food are included on each, and who would benefit from them) (clear fluids, full fluids, thickened fluids, and regular)
Clear fluids:
Includes broth, clear juices, and gelatin; beneficial for patients recovering from surgery or those with gastrointestinal issues.
Full fluids:
Comprise all clear liquids plus cream soups, milk, and custards; ideal for patients who may have difficulty chewing or swallowing solid foods.
Thickened fluids:
May include nectar, honey, and pudding consistency fluids; recommended for patients with swallowing difficulties to minimize aspiration risk.
Regular diet:
A balanced diet that includes all food groups; suitable for most patients as it provides adequate nutrition for recovery and overall health.
Considerations when feeding a client, considerations for a client with dysphagia.
Ensure that food options are appropriate in consistency; avoid anything that may be difficult to swallow, such as whole pieces of meat or dry bread.
Encourage small bites and thorough chewing to facilitate swallowing.
Position the client upright during meals to reduce the risk of choking and aspiration.
Monitor the client for signs of difficulty swallowing or discomfort, and adjust food textures as necessary.
What is dysphagia? What is a complication of dysphagia?
Dysphagia is a medical condition characterized by difficulty in swallowing due to various underlying causes, such as neurological disorders or structural abnormalities.
A complication of dysphagia can include aspiration pneumonia, which occurs when food or liquids enter the lungs instead of the stomach, leading to infection.
What is the role of the Speech language pathologist (SLP) and when should they be consulted?
The role of the Speech Language Pathologist (SLP) is to assess and treat swallowing disorders, providing specific interventions to improve swallowing function and ensure safe nutrition.
They should be consulted when a patient presents with signs of dysphagia, such as coughing during meals, weight loss, or recurrent respiratory infections, as early intervention can significantly improve outcomes.
What are some safety considerations when feeding a client?
Ensure the patient is seated in an upright position to reduce the risk of aspiration.
Offer small bites and encourage the patient to chew thoroughly before swallowing.
Ensure that adaptive equipment, such as specialized utensils or plates, is used to assist with feeding.
Monitor the patient closely for any signs of distress, such as choking or difficulty breathing, during meals.
Use appropriate utensils and food textures based on the patient's swallowing ability, avoiding hard, dry, or sticky foods.
Monitor the patient closely during meals for any signs of distress or difficulty.
Allow ample time for eating and encourage the patient to take small bites and chews adequately before swallowing.
How do you convert pounds to kilograms?
To convert pounds to kilograms: 1 pound is approximately equal to 0.45 kilograms for easier mental calculations.
Formula: Weight in kilograms = Weight in pounds × 0.45
Weight in pounds/2.2
Temperature, Pulse, Respiration, Blood Pressure and Oxygenation
Why do we check vital signs?
Vital signs provide essential information about a patient's current health status, helping to identify any changes or potential issues that require immediate attention.
When do we check vital signs?
Vital signs are typically checked during patient admissions, at regular intervals throughout hospitalization, before and after medical procedures, and whenever there is a change in the patient's condition.
Normal ranges for temperature, pulse, respirations, blood pressure and oxygenation for all age groups.
Temperature:
Normal range: 36 to 38 degrees Celsius
Pulse:
Normal Range: 60-100 BPM
Rhythm: Irregular or regular
Rate: BPM
Strength: 0-4+
Equality: Lateral or bilateral
Respirations:
Normal range: 12-20 BPM (Breaths per minute)
Blood Pressure:
Normal range: 120/80 mmHg
S/D - Systolic/diastolic
Measurement: mmHg (millimetres of mercury)
Oxygen Saturation:
Normal range: 95%-100%
Those who have COPD (Chronic obstructed pulmonary): 88%-92%
Factors affecting/influencing temp, pulse, respirations and blood pressure, oxygen saturation.
Environmental conditions (e.g., altitude, temperature)
Activity level and exercise
Age and health status of the individual
Hydration levels and blood volume changes
Smoking and inhalation of pollutants
Recent respiratory infections or illnesses
Common sites for Temp (how to determine most appropriate site, technique and considerations for each site, advantages and disadvantages of each site)
Common sites for temperature measurement:
Oral: Convenient and non-invasive; influenced by recent eating or drinking.
Rectal: Most accurate; recommended for infants and critically ill patients but invasive.
Axillary: Safe and easy; less accurate than other methods, affected by environmental temperature.
Tympanic: Quick and relatively accurate; may be affected by earwax or improper technique.
Temporal artery: Non-invasive and fast; can be affected by sweating or hair coverage.
What are some non-pharmacological ways to reduce temperature?
Cool compresses: Applying a cool, damp cloth to the forehead, wrists, and neck can help lower body temperature.
Hydration: Encouraging fluid intake, particularly cool water or electrolyte drinks, aids in regulating body temperature.
Ambient temperature management: Keeping the room cool, using fans, or air conditioning can support the body's natural cooling processes.
Tepid sponge baths: Immersing or sponging with lukewarm water can promote heat loss through evaporation.
Different pulse sites (where to find each on the body, why would you check for different pulse sites, characteristics of pulse - rate, rhythm, volume, equality)
Radial pulse: Located at the wrist, on the thumb side; commonly used due to its accessibility. It provides a good indication of heart rate and rhythm in conscious patients
Carotid pulse: Found in the neck beside the trachea; used in emergencies to assess circulation when other sites are difficult to feel.
Femoral pulse: Located in the groin area; important in assessing blood flow to the lower body, especially in trauma cases.
Popliteal pulse: Found behind the knee; helps evaluate circulation to the lower legs.
Dorsalis pedis pulse: Detected on the top of the foot; significant for checking arterial supply to the foot.
Posterior tibial pulse: Located behind the ankle; assesses circulation in the foot and helps identify peripheral vascular disease.
Axillary pulse: Palpated in the armpit; crucial for evaluating blood flow to the upper limb.
Apical pulse: Heard at the apex of the heart; vital for assessing heart rate and rhythm, helping to monitor cardiac function.
Brachial pulse: Found on the inner aspect of the arm; important for checking blood pressure and assessing circulation to the forearm and hand.
Characteristics of pulse include:
Rate: The number of beats per minute, indicating heart function health.
Rhythm: Regularity of beats, which can reveal potential arrhythmias.
Volume: Strength of the pulse, reflecting cardiac output and vascular resistance.
Equality: Ensuring both sides of the body have similar pulse strength is vital for detecting vascular issues.
Respirations (procedure to assess, characteristics – rate, rhythm, depth, volume, sounds, secretions)
Rate: The number of breaths per minute, an important indicator of respiratory function.
Rhythm: The pattern of breathing, which can be regular or irregular, and may indicate underlying health concerns.
Depth: The amount of air inhaled or exhaled, providing insight into the efficiency of the respiratory system.
Volume: The total amount of air exchanged during each breath, crucial for assessing overall lung capacity.
Sounds: Auscultation can reveal wheezing, crackles, or diminished breath sounds, which are significant for diagnosing respiratory conditions.
Secretions: Observation of any abnormal mucus or sputum can help identify infections or other respiratory issues.
Blood pressure (procedure and technique) What is happening during the diastolic and systolic phase?
During the systolic phase, the heart contracts and pumps blood into the arteries, causing the pressure to rise, which is measured as the systolic blood pressure.
during the diastolic phase, the heart relaxes and fills with blood, leading to a decrease in pressure, measured as diastolic blood pressure. Understanding these phases is essential for accurate blood pressure assessment and diagnosis.
Why is bp cuff size important? What is the correct way to measure and position a bp cuff?
The blood pressure cuff size is crucial because an improperly fitting cuff can lead to inaccurate readings; a cuff that is too small may give falsely elevated readings, while one that is too large may produce falsely low results.
To measure blood pressure accurately, the cuff should be placed around the upper arm, ensuring that it is snug but not too tight, approximately one inch above the elbow crease. Additionally, the patient's arm should be at heart level, with the palm facing upward to facilitate proper measurement.
Define hypotension, and hypertension, postural hypotension.
Hypotension: A condition characterized by abnormally low blood pressure, often defined as a systolic pressure below 90 mmHg, which can lead to symptoms such as dizziness, fainting, or fatigue.
Hypertension: A condition marked by consistently elevated blood pressure readings, typically defined as a systolic pressure above 130 mmHg or a diastolic reading exceeding 80 mmHg, increasing the risk of heart disease and stroke.
Postural hypotension: Also known as orthostatic hypotension, this condition occurs when a person's blood pressure drops significantly upon standing up after sitting or lying down, which can lead to symptoms like lightheadedness and an increased risk of falls.
Why is it important to understand a patients baseline oxygen saturation?
Understanding a patient's baseline oxygen saturation is crucial because it helps determine any deviations from their normal levels, which can indicate the onset of respiratory distress or complications related to underlying health conditions. Additionally, by knowing the baseline, healthcare providers can make informed decisions regarding interventions and monitor the effectiveness of treatments.