Chapter 21: The Heart
Introduction to the Cardiovascular System
The cardiovascular system is essential for maintaining homeostasis by supplying oxygen and nutrients through blood circulation.
Proper heart function adjusts pumping capacity to meet tissue demands.
The Heart is the primary organ in the cardiovascular system, it never stops contracting, ensuring blood stays in motion and efficiently delivers essential substances to various tissues while also aiding in the removal of waste products.
Controlled by the autonomic nervous system
Cardiac Output: volume of blood pumped per minute— worries between 5 and 30 liters per minute
Overview of the Cardiovascular System
Two Closed Circuits:
The heart has 4 muscular chambers, acting together as one muscle:
R & L Atria (2)
R & L Ventricles (2)
The heart acts as a double pump:
Pulmonary Circuit: Oxygen-deficient blood is pumped from the right atrium to the right ventricle, transported to the lungs for oxygenation, and then returned to the left atrium, where it is distributed to the left ventricle before being pumped into the systemic circuit.
Short, low-pressure citculation
Systemic Circuit: Oxygen-rich blood is pumped from the left ventricle into the aorta, which delivers it to the rest of the body, providing essential nutrients and oxygen to tissues before returning deoxygenated blood to the right atrium.
Long, High-pressure circulation
There is also the Coronary Circuit: Which supplies the heart muscle with oxygenated blood, and then back to the R side of the heart
Blood Vessels:
Arteries: A vessel that transports blood away from the heart.
Veins: A vessel that transports blood to the heart.
Capillaries: Thin-walled vessels that interconnect for nutrient and gas exchange “exchange vessels”
This is the only place where things can leave the CVS, as it is a closed system
Heart Chambers:
Four chambers:
Right Atrium
Right Ventricle,
Left Atrium
Left Ventricle.
Atria collect incoming blood
Ventricles pump blood out.
Structure of the Heart Wall
Layers of the Heart Wall:
Epicardium: Visceral layer of serous pericardium.
Myocardium: Muscular layer, facilitating contraction.
Endocardium: Linings inside of heart chambers (covers 2 AV valves, 2 Semilunar valves, 2 atria, and 2 ventricles)
Cardiac Muscle Tissue:
Cardiac muscle cells are small, depend on aerobic respiration.
Intercalated Discs connect cardiac muscle cells, conducting impulses and forces of contraction.
The Pericardium
Pericardium:
The Body Cavity that surrounds the heart, located in the mediastinum.
Contains pericardial fluid for lubrication.
Visceral Pericardium (inner, epicardium) covers the heart; Parietal Pericardium (outer) lines the cavity.
Fibrous Pericardium— Fibrous sac that anchors pericardial cavity to the diaphragm
The Cardiac Skeleton
Function of Fibrous Cardiac Skeleton:
Stabilizes contractile cells and valves, providing physical support
Supports blood vessels and nerves, adds strength and elasticity, isolates atria from ventricles.
Orientation and Superficial Anatomy of the Heart
Heart Orientation:
Rotated slightly to the L
Anterior Surface:
R Atrium, R Ventricle, L Ventricle
Posterior Surface:
L Atrium, a small portion of R Atrium
Positioned at an angle, base at the top (great vessels connection) and apex at the bottom.
Major surfaces include: anterior (sternocostal), posterior, and diaphragmatic surfaces.
External Landmarks:
Grooves mark chamber separations:
Interatrial Groove— Separates L & R atria
Coronary Sulcus— Separates the atria and the ventricles
Anterior Interventricular Sulcus— Separates L & R ventricles
Posterior Interventricular Sulcus— Separates L & R ventricles
Auricle of R Atrium— Small, ear-shaped muscular pouch that increases capacity for blood collection
Auricle of L Atrium— Small, ear-shaped muscular extension functioning as a reservoir for blood returning from the pulmonary veins
Auricles are extensions of atria.
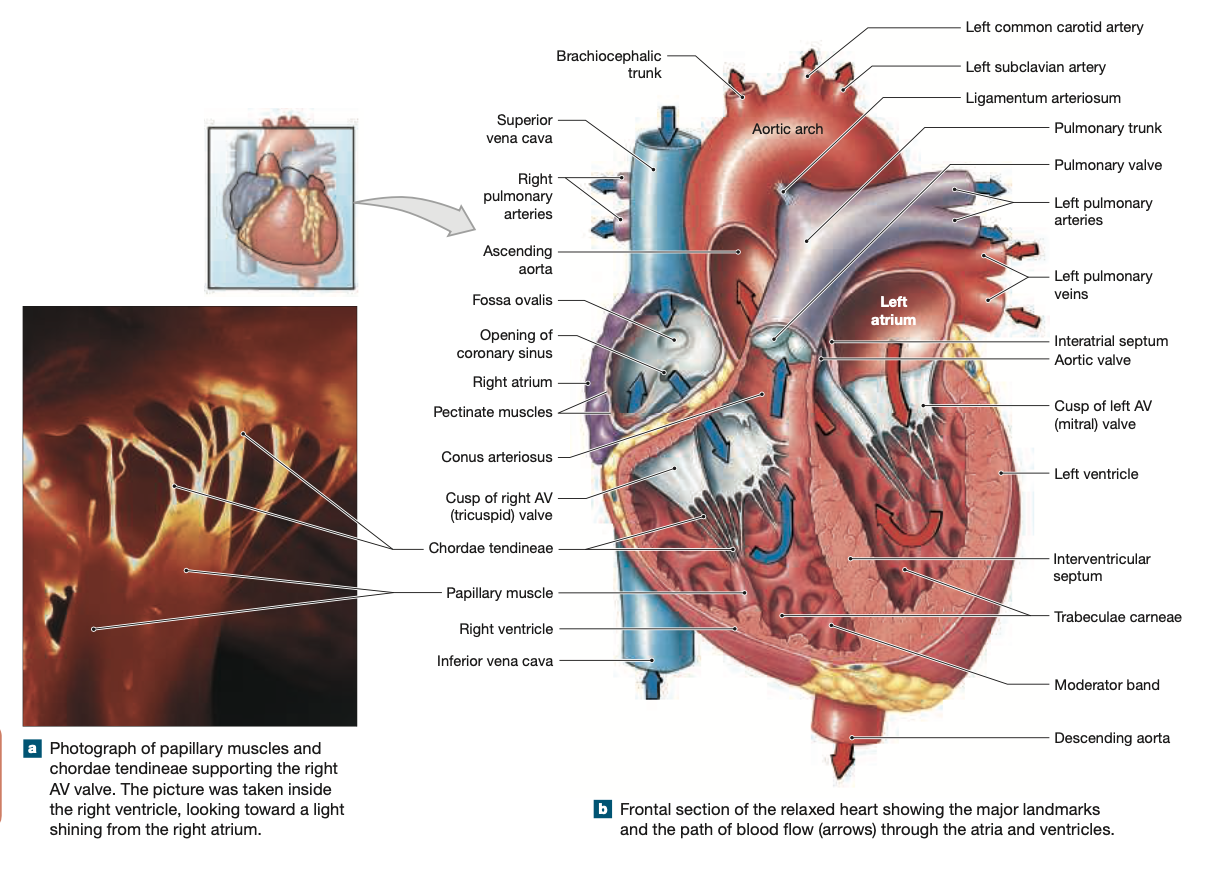
Internal Anatomy and Organization of the Heart
Separation of Chambers:
The interventricular septum separates atria, interventricular septum separates ventricles.
Valves maintain one-way blood flow between chambers.
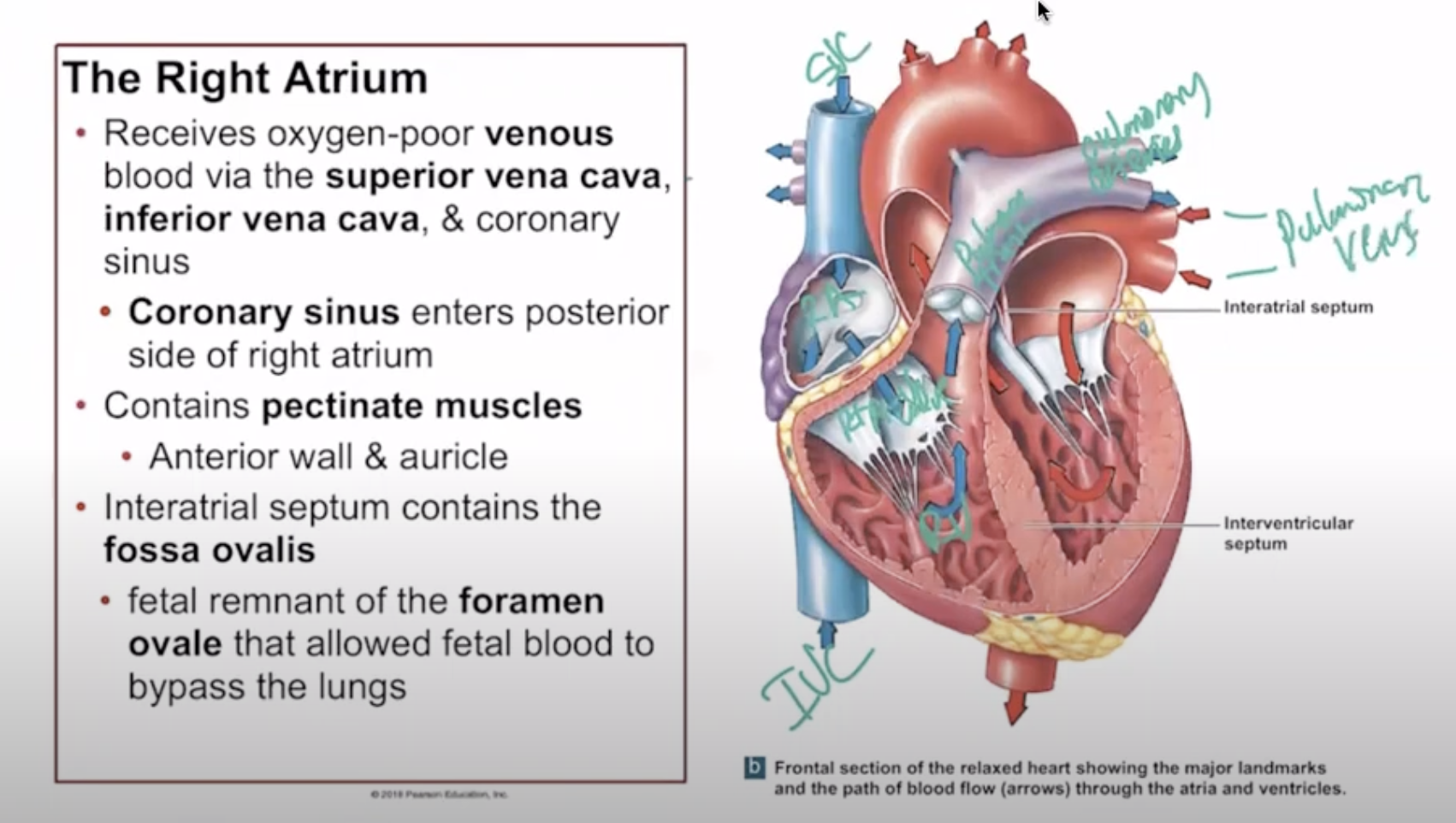
Right Atrium
Receives deoxygenated blood from systemic circulation via the:
Superior Vena Cavae— everything above the diaphragm
Inferior Vena Cavae— everything below the diaphragm
Coronary sinus— collects deoxygenated blood from the heart muscle
Contains pectinate muscles (pectinate describes muscle pattern) and the fossa ovalis (remnant of foramen ovale).
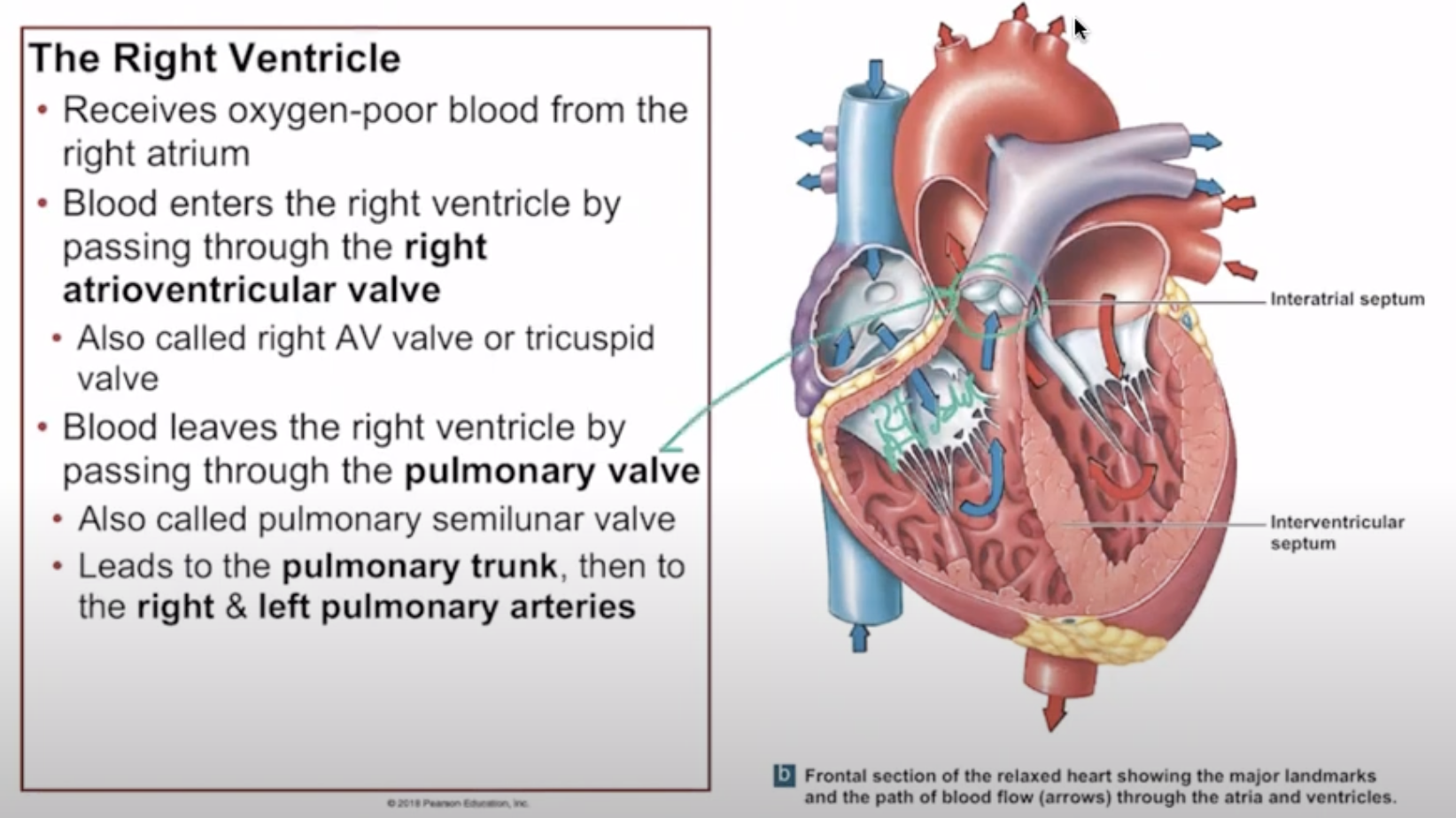
Right Ventricle
R ventricle receives oxygen-poor blood from the R atrium
Blood flows through the R Atrioventricular (tricuspid) or (R AV Valve) to the right ventricle.
The R ventricle contracts, forcing blood toward the Pulmonary (Semilunar) Valve, which opens due to the increased ventricular pressure.
The blood then exits to the Pulmonary Trunk, a large artery that carries deoxygenated blood to the R & L pulmonary arteries and then lungs.
Papillary Muscles hold the valve shut to prevent backflow of blood into the right atrium during ventricular contraction, ensuring one-way flow through the heart.
Chordae tendineae— the chords that hold the papillary muscles in place and prevent the inversion of the valves
Moderator band— a fibrous band of muscle tissue that helps synchronize the contraction of the heart's chambers due to pressure differences
Found only in R ventricle
Trabecular carneae— Muscle pattern found on the inner walls of the ventricles that assist in the contraction
Interventricular septum— separates L & R ventricles, preventing overexpansion of the thin-walled R ventricle
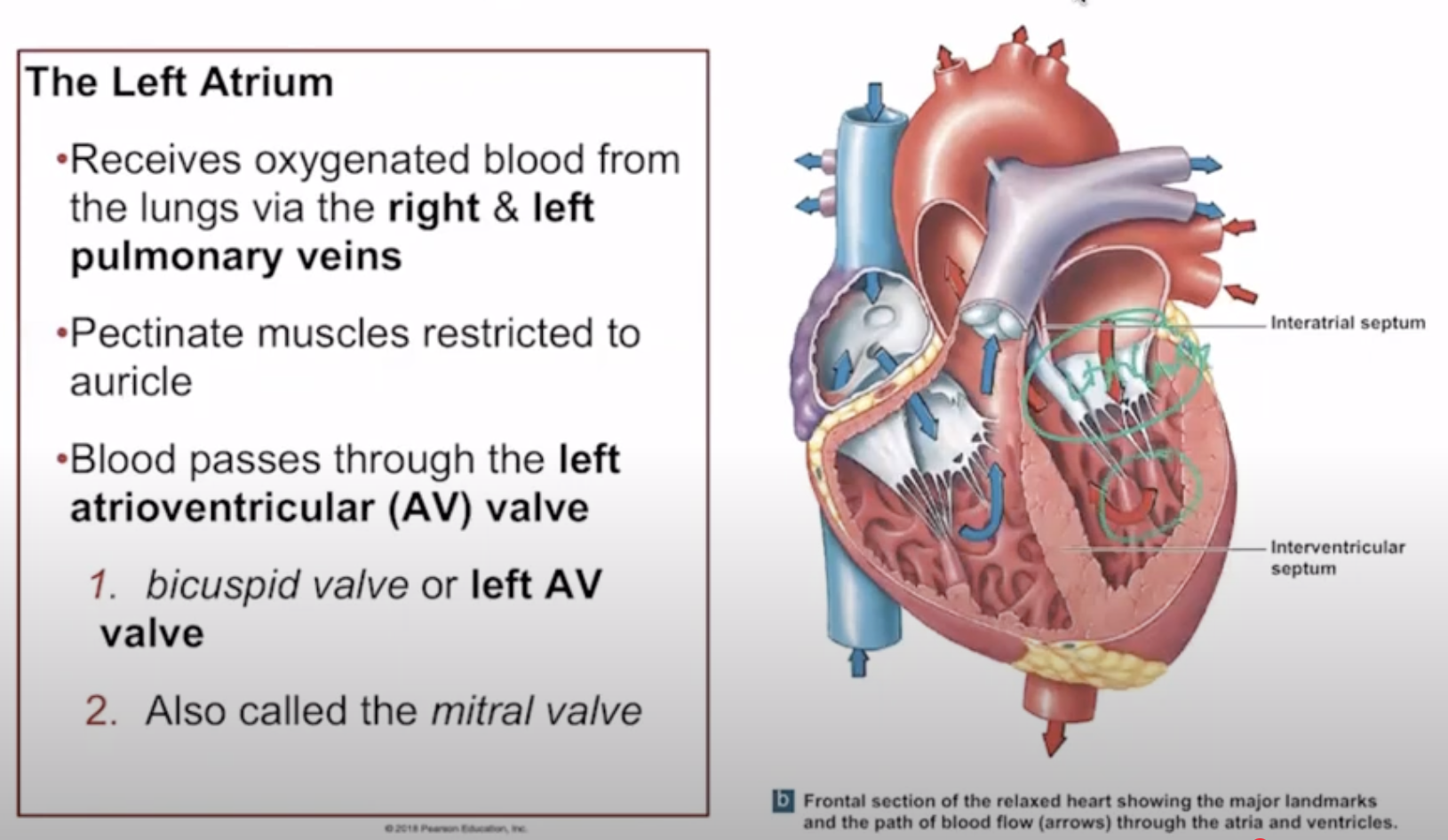
Left Atrium
Receives oxygenated blood from Pulmonary Veins
The L atrium has thicker walls than the R atrium because of the greater pressure it must withstand while pumping blood into the left ventricle.
Blood flows to the left ventricle through the L Atrioventricular (mitral or bicuspid) or AV valve.
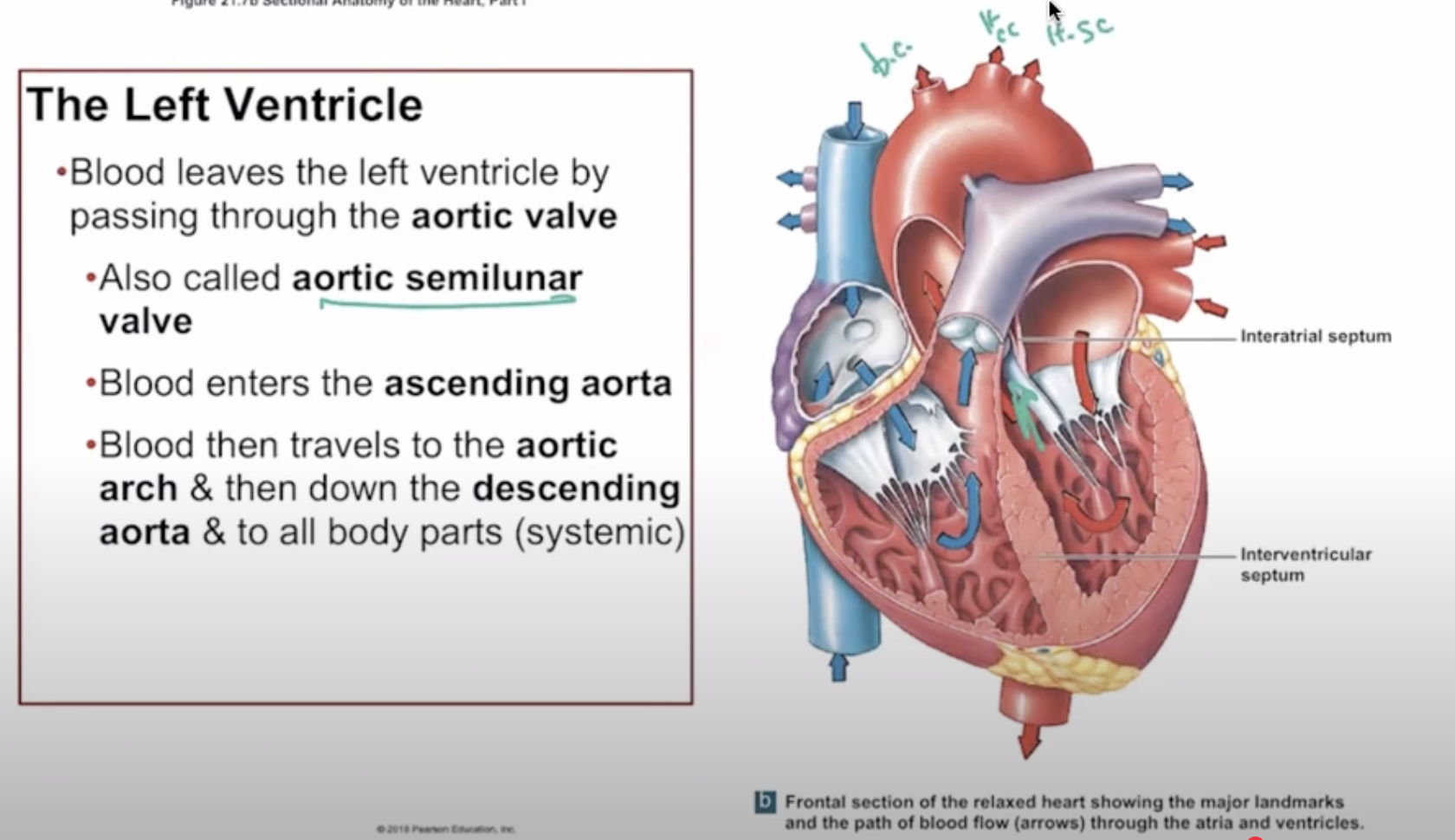
Left Ventricle
Largest and thickest chamber; pumps blood to the systemic circuit via the Aortic Valve (aortic semilunar valve), and the Aorta which has three branches servicing the upper body
Brachiocephalic Trunk— supplies blood to the right arm and head, splitting into the right subclavian and right common carotid arteries.
L Common Carotid Artery— supplies blood to the left side of the head and neck
L Cubclacarian Artery— supplies blood to the left arm and shoulder
Pumps at high pressure necessary for systemic distribution.
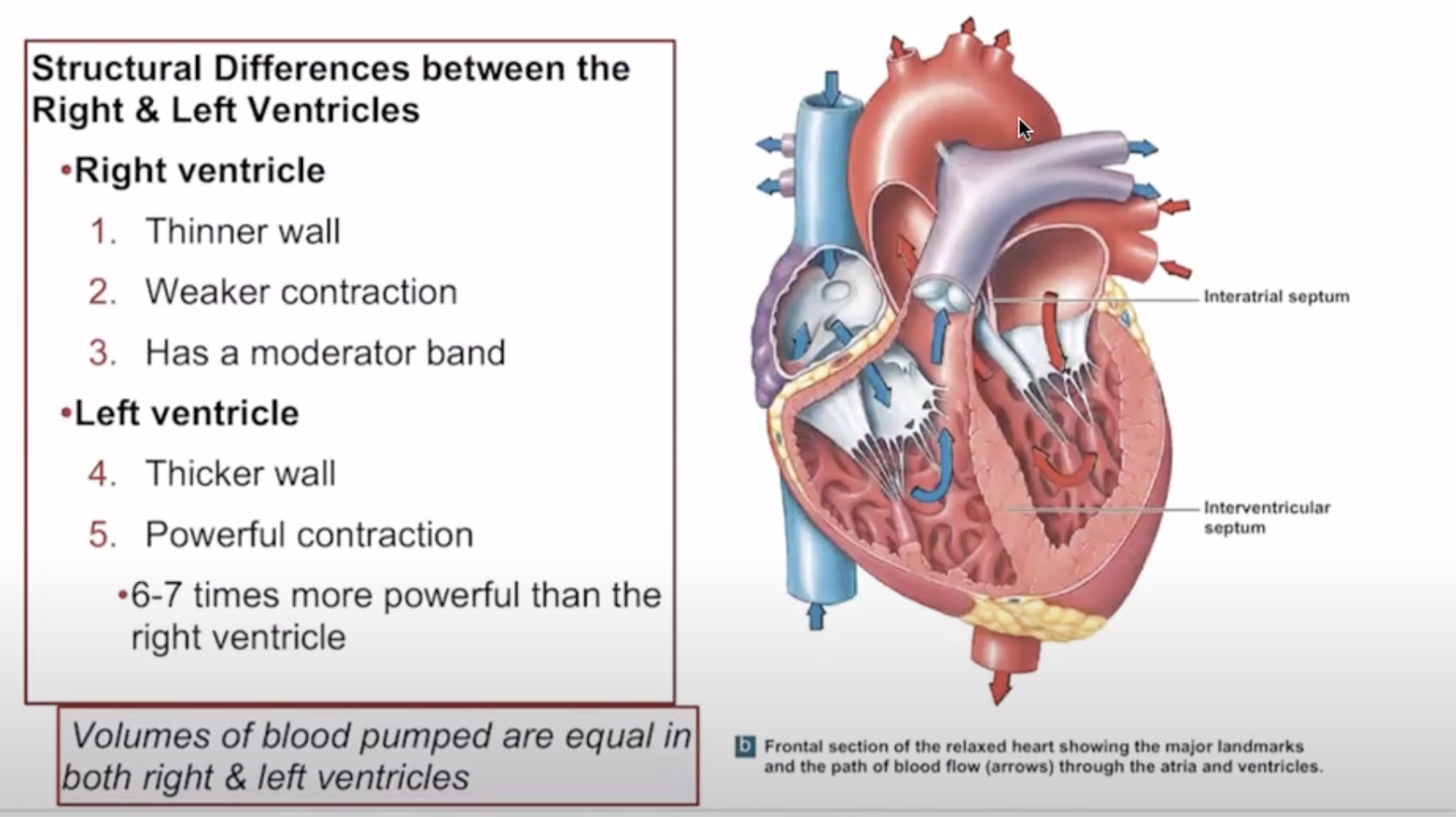
Structural Differences Between Right and Left Ventricles
R ventricle has thin walls for low-pressure function.
L ventricle has thick muscular walls for high-pressure output throughout the body.
Heart Valves
Components of AV Valves :
R & L AV Valves— Have CT cusps (flaps) attached to chordae tendineae and papillary muscles, which prevent backflow into the atria.
Lubb— AV valves closing during ventricular contraction, beginning of ventricular systole (contracting), resulting in the first heart sound.
Semilunar Valves:
Aortic and Pulmonary valves have three crescent-shaped cusps but no chordae tendineae or papillary muscles.
The cusps open passively due to blood pressure changes and snap shut to prevent backflow.
Dubb— semilunar valves closing creates the second heart sound, signaling the end of ventricular systole and the beginning of ventricular diastole (not contracting).
Function: Supplies blood to the heart muscle; high oxygen demand due to aerobic metabolism.
Coronary Sinus: A large vein that collects deoxygenated blood from all coronary veins, and empties it into the R atrium for the pulmonary circuit.
Coronary Arteries and Branches:
Right coronary artery (RCA) gives rise to right marginal and posterior interventricular branches
Passes between the R auricle & pulmonary trunk and supplies blood to the right atrium, right ventricle, and parts of the left ventricle
Left coronary artery (LCA) gives rise to circumflex and anterior interventricular branches.
Branches into the anterior interventricular artery and the circumflex artery, supplying blood to the left atrium and left ventricle.
RCA & LCA originate at the aortic sinus
Coronary Veins
Drain blood from the myocardium into the coronary sinus.
Includes great cardiac vein, middle cardiac vein, and others draining the heart's surface.
Coordination of Cardiac Contractions
Autorhythmicity: Cardiac muscle contracts independently of neural inputs.
Nodal Cells:
Set the heart rate (mainly SA node) and distribute impulses.
Cardiac Cycle
Consists of the phases of contraction (systole) and relaxation (diastole).
Impulse conduction progresses through SA node, AV node, AV bundle, and Purkinje fibers.
Autonomic Control of Heart Rate
Heart Rate Modulation:
Basic rhythm set by pacemaker cells but modulated by the autonomic nervous system (ANS).
Norepinephrine increases heart rate; acetylcholine decreases it.
Cardiac centers in medulla oblongata respond to pressure and gas concentrations.