CH.7 The Respiratory SYSTEM
%%Beginning of PP #1%%
Function and Structure of the Respiratory System
Functions of the Respiratory System
- The respiratory system has three major functions:
- Deliver air to the lungs and then move that air to the blood for distribution to the tissues
- Remove carbon dioxide waste and water waste from the blood, and discard it from the lungs
through exhalation - Move air through the larynx, enabling speech.
Structure of the Respiratory System
- The respiratory system can be divided into two broad categories: The upper respiratory system and the lower respiratory system.
- The upper respiratory system consists of the nose, mouth, pharynx, larynx, epiglottis, and trachea.
- The lower respiratory system consists of the bronchial tree and lungs, and is located in the thoracic cavity.
The Nose
- The nasal cavity is located on the interior portion of the nose, and is usually where air enters the body. Nas/o means
- “nose,” and –al means “pertaining to.”
- The nostrils are the external openings of the nose, and the nasal septum is a piece of cartilage that separates the nose into two (usually) equal sections.
- Olfactory receptors are nerve endings in the nose that provide the senses of smell and taste.
- The nose has some mechanisms to help prevent infection:
- Cilia are tiny, thin hairs just inside the nostrils that serve as a filtration system for the incoming air.
- Mucous membranes serve as the lining of the nose as well as other parts of the respiratory system. They secrete mucus.
- Mucus is a slippery fluid secreted by the mucous membranes that protects and lubricates tissues, as well as trapping pathogens and foreign substances.
Tonsils
- The tonsils and adenoids are also part of the lymphatic system, but are also considered part of the respiratory system.
- These structures help defend the body from infectious substances from entering the nose and mouth.
- The palatine tonsils are located at the back of the mouth, and are generally just called the tonsils.
- The nasopharyngeal tonsils are located behind the nose and palate, and are commonly called the adenoids.
- Nas/o means “nose,” pharyng/o means “pharynx,” and –eal means “pertaining to.”
The Sinuses
There are 4 pairs of paranasal sinuses, which are generally just called the sinuses.
Para- means “near,” nas/o means “nose,” and –al means “pertaining to.”
They are air-filled cavities lined with mucous membranes.
The sinuses have 3 major functions:
- To lighten the bones of the skull
- To provide resonance for the voice
- To produce mucus for the nasal cavity
The frontal sinuses are located just above the eyebrows.
The sphenoid sinuses are located behind the eye, in the sphenoid bone
The maxillary sinuses are located just under the eyes
The ethmoid sinuses are located between the nose and eyes.
The Pharynx and Larynx
- The pharynx is also known as the throat, and has three divisions:
- The nasopharynx is the part of the throat posterior to the nasal cavity, and goes behind the mouth. This is the passageway for the air from the nose.
Nas/o means “nose.”
- The oropharynx is the visible part of the throat when looking in the mouth; it is shared by the respiratory and digestive systems.
Or/o means “mouth.”
- The laryngopharynx is also shared by the respiratory and digestive systems; it opens into the esophagus (for food) and the trachea (for air).
Laryng/o means “larynx.”
- The larynx is also called the voicebox, and is located between the laryngopharynx and the trachea.
- The Larynx is protected by 9 pieces of cartilage, the largest of which is the thyroid cartilage. This piece of cartilage can protrude, and is known as the Adam’s apple.
- The vocal cords are located in the larynx. During speech, they come together and vibrate as air is expelled through the lungs.
The Trachea
- The trachea transports air to and from the lungs.
- It is located anterior (in front of) the esophagus.
- The trachea is held open by rings of cartilage that allow it to compress so food can fit down the esophagus.
Swalloing
- Due to the proximity of the trachea to the esophagus, the risk of aspiration, or choking, is high. Food and liquids could move into the trachea instead of the esophagus.
- There are two protective mechanisms to prevent this:
- During swallowing, the posterior portion of the roof of the mouth (or the soft palate) moves up
and back to prevent food and/or liquid form going into the nose. - The epiglottis, which is a lid-like tissue at the base of the tongue, swings down and closes the opening of the trachea.
- If swallowing happens too quickly, or if either of these mechanisms are compromised, then choking could occur.
The Lower Respiratory Tract and The Bronchi
- The lower respiratory tract consists of the bronchi, the alveoli, the lungs, and the diaphragm.
- The bronchi are 2 tubes that branch out from the trachea to the right and left sides. They bring air to the lungs.
- The bronchi and the lungs as a whole are called the bronchial tree.
- In the lungs, the bronchi continue, and divide into smaller and smaller branches called bronchioles
The Alveoli
- Alveoli are also called air sacs, and are clusters of sacs at the end of each bronchiole. They are arguably the most important structure in the lungs.
- Alveoli are the site of oxygen and carbon dioxide exchange in the body. Each lung has millions of alveoli.
- Pulmonary capillaries surround each alveolus, which allows the oxygen and carbon dioxide to move into and out of the blood, respectively.
- The alveoli also produce a substance called surfactant, which is a substance that reduces the surface tension of the alveoli, allowing them to open easier. This decreases the likelihood that the alveoli would collapse.
- Surfactant is the substance that is lacking in premature infants that makes their lungs immature. If premature infants that are struggling to breathe are given synthetic surfactant, their survival rates increase.
The Lungs
- The lungs are divided into lobes.
- The right lung has 3 lobes, and the left has 2 lobes. The left only has 2 because of the space taken up by the heart on that side of the thoracic cavity.
- The mediastinum refers to the middle part of the chest.
- It contains the tissues, heart, esophagus, trachea, lungs, lymph nodes, bronchi, other organs, and the thymus.
- The pleura is a membrane that surrounds the lungs and lines the inside of the thoracic cavity. It contains two layers.
- The parietal pleura is the outer layer, which lines the thoracic cavity and forms the parietal sac.
- The visceral pleura is the inner layer that is attached to the lung.
- Viscer/o means “vital organ,” and – al means “pertaining to.”
- The pleural cavity (or pleural space) is the fluid-filled space between the pleura, which allows for smooth movement during respiration.
The Diaphragm
- The diaphragm is the sheet of muscle separating the thoracic and abdominal cavities, and is essential for breathing.
- The diaphragm is stimulated by the phrenic nerves, meaning that if those nerves are compromised, breathing will also be compromised.
- The image on the right shows the respiratory system from the sinuses down through the diaphragm.
Respiration
- Respiration is defined as the exchange of oxygen and carbon dioxide; a single breath is considered one complete inhalation and exhalation. This process is also called ventilation.
- Inhalation is the action of bringing air into the lungs, which is accomplished by the contraction of the diaphragm, which pulls it downward, expanding the thoracic cavity.
- The expansion of the cavity causes a vacuum, which is filled by air.
- Exhalation is the process of pushing air out of the lungs, which is accomplished through the relaxation of the diaphragm, which moves it upwards, forcing the air out of the lungs as the thoracic cavity is compressed and returned to its original state.
Types of Respiration
- There are two types of respiration: External and internal.
- External respiration is inhalation and exhalation, or bringing air into the lungs for oxygen and carbon dioxide exchange, and then pushing the air back out.
- During inhalation, the oxygen immediately moves to the capillaries and goes to the red blood cells for body-wide distribution, and waste products move to the lungs. Those waste products are removed via exhalation in the form of carbon dioxide.
- Internal respiration is also called cellular respiration, and is the exchange of gases from the red blood cells and tissues.
- Oxygen passes from the blood to cells, and the blood takes up the waste from the cells in the form of carbon dioxide.
- Blood then takes the waste back to the lungs for removal.
%%Beginning of PP #2%%
Pathology of the Upper Respiratory System
Systemic Disorders: COPD
- Chronic Obstructive Pulmonary Disease (COPD) is a disorder characterized by obstructed bronchial airflow. This is generally caused by long-term smoking.
- COPD is progressive and permanent; people with COPD are also very susceptible to emphysema and chronic bronchitis.
- Emphysema is the long-term loss of lung function, which is also progressive. It has 3 major characteristics:
- A decrease in the number of alveoli.
- Enlargement of the remaining alveoli.
- Destruction of the alveoli. This causes rapid, shallow breathing, which causes the lungs to overinflate, leading to a slightly round-shaped chest, also called a barrel chest.
- Chronic Bronchitis is airway inflammation/irritation due to repeated exposure to an irritant, generally cigarette smoke.
- Bronchi/o means “bronchial,” and –itis means “inflammation.”
- This inflammation leads to an increase in mucus production and the thickening of the air passages, causing chronic coughing and making the patient more susceptible to bacterial lung infections.
Systemic Disorders: Asthma
- Asthma is another prevalent chronic inflammatory disease. A person with asthma is known as an asthmatic. Asthma is characterized by episodic breathing difficulty, coughing, and wheezing. These episodes are known as asthma attacks.
- Wheezing is the sound caused by an airway that is partially obstructed.
- Asthma can be caused by allergens, environmental conditions, exercise, and infection.
- The airway inflammation of asthma causes the bronchial tubes to swell and fill with mucus.
- The bronchospasms of an asthma attack are contractions of the smooth muscle of the bronchi, causing them to shut. Asthma attacks can be life-threatening if not treated appropriately.
- Exercise-induced asthma is airway narrowing after 5-15 minutes of exertion, or can be caused by allergen exposure or cold weather.
Upper Respiratory Tract: General Terms
- Most upper respiratory tract infections are called acute nasopharyngitis, or the common cold.
- Nas/o means “nasal,” pharyng/o means “pharynx,” and –itis means “inflammation.”
- This can be caused by over 200 species of virus.
- Sinusitis is an inflammation of the sinuses.
- Sinus/o means “sinuses,” and –itis means “inflammation.”
- Rhinorrhea, or a runny nose, is a flow of mucus from the nose.
- Rhin/o means “nose,” and –rrhea means “flow.”
- Allergic rhinitis is an allergic reaction to airborne allergens, causing sinusitis and rhinorrhea.
- Rhin/o means “nose,” and –itis means “inflammation.”
- Epistaxis, or a nose bleed, may be due to a runny nose, injury, increased blood pressure, or anticoagulant use.
Upper Respiratory Tract: Infections
- Influenza is a highly-contagious viral infection that is most commonly spread during the cooler months.
- It causes an upper respiratory inflammation, chills, fever, and muscle pain.
- There are many strains of the influenza virus, so the vaccine must be amended each year to be effective against the prevalent strain of that year.
- Pertussis, or whooping cough, is a bacterial infection of the upper respiratory tract caused by Bordatella pertussis.
- Pertussis is characterized by a sudden cough, followed by shortness of breath and a noisy inhalation, which sounds like a whoop. Diphtheria is a bacterial infection of the throat and upper respiratory tract caused by Corynebacterium diphtheriae.
- This bacteria produces a toxin which can damage the heart and nerves, and can also produce a membrane over the throat, making breathing difficult.
- Croup is an illness that affects infants and young children, causing a barking cough and stridor.
- Stridor is a high-pitched sound caused by obstruction of the larynx and swelling of the vocal cords
Pharynx and Larynx Disorders
- Pharyngitis, or a sore throat, is inflammation of the pharynx caused by an illness, such as the cold, flu, or sinus infection.
- Pharyng/o means “pharynx,” and –itis means “inflammation.”
- Laryngitis is an inflammation of the larynx.
- Laryng/o means “larynx,” and –itis means “inflammation.”
- A laryngospasm is a sudden closure of the larynx. It is associated with gastroesophageal reflux disease.
- Laryng/o means “larynx,” and –spasm means “sudden movement.”
- Voice Disorders:
- Aphonia is the loss of the ability for normal speech sounds.
- A- means “without,” phon/o means “sound,” and –ia means “condition.”
- Dysphonia is difficulty speaking, which can impair vocal quality. Dys means “bad,” phon/o means “sound,” and –ia means “condition.”
Trachea and Bronchi Disorders
- Tracheorrhagia is bleeding of the mucous membranes of the trachea, which can be caused by a variety of factors, including injury.
- Trache/o means “trachea,” and –rrhagia means “bleeding.”
- Bronchiectasis is the permanent stretching, or dilation, or the bronchi.
- Bronchi/o means “bronchial tree,” and –ectasis means “dilation.”
- This can occur due to infection and inflammation, and can negatively affect respiration.
- Bronchiectasis causes an increased susceptibility to infection in the future, including severe respiratory infections.
- Bronchorrhea is excess mucus production in the bronchi. This often happens due to asthma or bronchitis.
- Bronch/o means “bronchial tree,” and –rrhea means “flow.”
- If the mucus gets too thick, there is an increased risk for infection and airway obstruction
%%Beginning of PP #3%%
Pathology of the Lower Respiratory Tract
Pleural Cavity Disorders
- There are various disorders that affect the pleural cavity:
- Pleurisy, also known as pleuritis, is an inflammation of the pleural cavity.
- Pleur/o means “pleural cavity,” and –itis means “inflammation.”
- Pleurisy can happen for a variety of reasons: infection, trauma, tuberculosis, a tissue disorder, or as a complication from pneumonia.
- Pleurodynia is pain that occurs when inflamed layers of the pleura rub against one another. Pleurisy is a common cause for pleurodynia.–dynia means “pain.”
- A pleural effusion is excess fluid accumulation in the pleural cavity, which prevents the lung from fully expanding, causing breathing problems.
- A pyothorax, also called empyema of the pleural cavity, is pus in the pleural cavity.
- Py/o means “pus,” and –thorax means “lung.”
- A hemothorax is an accumulation of blood in the pleural cavity, and can occur as a result of trauma to the chest.
- Hem/o means “blood.”
- A pneumothorax is an accumulation of air in the pleural space, which can cause the lung to collapse. As with a hemothorax, this can occur due to injury, or it can be the result of a disease process.
- Pneum/o means “air,” or “lung.”
Lung Disorders
- Acute respiratory distress syndrome (ARDS) is a life-threatening condition. It is characterized by inflammation in the lungs and fluid in the alveoli, which impairs oxygen exchange and causes low levels of oxygen in the blood.
- This can be caused by trauma, pneumonia, smoke, sepsis, or aspiration.
- Sepsis is a systemic bacterial infection of the blood.
- Pulmonary edema is the collection of excess fluid in the lung tissues, especially the alveoli, as a result of congestive heart failure
- A pulmonary embolism is the blockage of a pulmonary artery. This could be due to a clot, or by foreign matter. This is a life-threatening condition, unless treated promptly.
- Pneumorrhagia is bleeding from the lungs.
- Pneum/o means “lung,” and –rrhagia means “bleeding.”
- Atelectasis is also known as a collapsed lung, and is the lack of total expansion of the lung. This can be due to blockage, or due to a condition such as a pneumothorax
Lung Infections
- Tuberculosis (TB) is an infectious disease caused by Mycobacterium tuberculosis.
- TB is highly contagious, since it is an airborne pathogen.
- It generally attacks the lungs, causing pleurisy and hemoptysis, or coughing up blood.
- TB is an opportunistic pathogen, meaning that it causes disease most often in persons with compromised immune systems. Healthy people can carry TB without showing symptoms of the disease.
- Strains of TB have become multidrug-resistant, meaning that the normal antibiotics used to treat TB are ineffective. This can occur due to patients not strictly following their antibiotic regimen, allowing the bacteria to develop resistance.
- Cystic fibrosis (CF) is a genetic disorder that causes the lungs and pancreas to overproduce mucus, damaging the lungs and causing poor growth and nutrition.
- Although CF itself is not an infection, the thick mucus in the lungs can clog the lungs, leading to progressively more severe infections.
- The bacteria responsible for lung infections in individuals with CF eventually become drug-resistant, and these infections generally cause death at a young age.
Pneumonia
- Pneumonia is an inflammation of the lungs in which the alveoli and airways fill with pus and fluids. It can be caused by bacterial or viral infections, and often follow infections that weaken the immune system.
- There have been numerous causative agents of pneumonia identified, but most are caused by bacteria, fungi, viruses, air pollution, or aspirated liquids or chemicals.
- Some types of pneumonia are named for their location in the lungs, and other types are named for their cause.
- Bronchopneumonia is pneumonia that affects the bronchioles, and begins as a localized inflammation. This can lead to lobar pneumonia.
- Lobar pneumonia is pneumonia that affects one or more lobes of a lung. If the pneumonia affects both lungs, it is called double pneumonia.
- Bacterial pneumonia is pneumonia caused by a bacterial infection, and is also called pneumococcal pneumonia. The bacteria responsible is often Streptococcus pneumoniae.
- Walking pneumonia is caused by a bacteria known as Mycoplasma pneumoniae, and causes a longer-lasting, but often milder form of pneumonia. This disease gets its name from the fact that the patient generally is not hospitalized or bedridden.
- Pneumocystis pneumonia is caused by a fungus called Pneumocystis carinii. This is an opportunistic infection, and is often the disease that causes death in individuals with AIDS.
- Viral pneumonia causes around 30% of all pneumonia, and can be caused by a number of viruses.
- Aspiration pneumonia is caused by aspiration, which is the inhalation of a foreign substance into the lungs, usually food or liquid, but occasionally vomit or chemicals.
- Community-acquired pneumonia is a pneumonia that results from an infection acquired outside of a hospital or clinic. It may be caused by a bacteria, virus, or fungus, and is the most common form of pneumonia.
- Hospital-acquired pneumonia is pneumonia that is acquired during a hospital stay or visit to a clinic. This is especially severe for patients on a ventilator, who are particularly susceptible to this type of illness.
- Another term for hospital-acquired pneumonia is nosocomial pneumonia. Nosocomial means hospital-acquired.
Interstitial Lung Diseases
- Interstitial lung diseases are a group of disorders that cause inflammation and scarring of the alveoli and the tissues that support them. These tissues become stiff from the scarring, which reduces the amount of oxygen that can be transferred.
- Interstitial means “related to the spaces within or around a tissue or organ.”
- This can occur due to connective tissue diseases (such as rheumatoid arthritis or scleroderma), or environmental toxins such as asbestos and silica.
- Pulmonary fibrosis is also called interstitial fibrosis, and is the formation of scar tissue in the lung, causing decreased lung capacity and difficulty breathing. In fibrosis, normal tissue is replaced by hardened fibrotic tissue.
- Pneumoconiosis is fibrosis caused by dust in the lungs. This usually occurs after occupational or environmental contact.
- Silicosis is pneumoconiosis caused by inhaling silica dust. This occurs from occupations such as ceramics, sandblasting, glasswork, quarrying, and foundry work.
- Asbestosis is pneumoconiosis caused by inhaling asbestos particles, which were used as building materials in the past.
Lung Cancer
- Lung cancer is the leading cause of cancer death in the United States.
- Risk factors for lung cancer include smoking, and inhaling secondhand smoke.
Breathing Disorders: General Terms
- Breathing disorders describe a large group of disorders that cause changes in breathing, either the rate of breathing or the depth of breathing.
- Eupnea is baseline breathing, or breathing that is at a normal rate and easy to perform. Generally, an adult has a normal respiratory rate of between 12 and 20 breaths per minute.
- Eu- means “good,” and –pnea means “breathing.”
- Apnea is the absence of normal respiration. This is temporary, and occurs often in premature infants, and can also occur during sleep.
- A- means “without,” –pnea means “breathing.”
- Sleep apnea is a disorder in which breathing repeatedly stops and starts, decreasing the blood oxygen levels. Obstructive sleep apnea is caused by a narrowing of the airway caused by relaxed muscles at the back of the throat.
- Snoring is a symptom of sleep apnea, and is noisy breathing during sleep.
Breathing Disorders
- Bradypnea is an abnormally slow respiratory rate, generally under 10 breaths per minute.
- Brady- means “slow,” and –pnea means “breath.” Tachypnea is an abnormally fast respiratory rate, generally over 20 breaths per minute. Tachy- means “fast.”
- Dyspnea is also called shortness of breath, and is difficult breathing. Often, this type of breathing is also described as labored breathing. Dyspnea can often be the first symptom of congestive heart failure.
- Cheyne-Stokes respiration is a type of breathing characterized by an irregular pattern, which includes rapid and shallow breaths, and short periods of apnea. This breathing pattern is seen in patients nearing death.
- Hyperpnea occurs with exertion, and is breathing that is deeper and more rapid than normal breathing. It can also be caused by some disease states, or in areas of high altitude. Hyper- means “excessive.”
- Hypopnea is a shallow and slower than usual respiration.
- Hypo- means “beneath.”
- Hyperventilation is quick and deep respiration. This can happen with anxiety, and causes dizziness and tingling in the extremities.
Breathing Disorders: Coughing
- Coughing is a reflex, and is the act of clearing the throat and airways of mucus or foreign materials. It is an important mechanism to clear the body of pathogens and other harmful substances.
- Expectoration is synonymous with coughing, and is the act of coughing up and spitting out mucus, saliva, or other body fluids.
- Hemoptysis is the coughing or expectoration of blood or blood-stained mucus from the lungs or bronchial tubes, caused by bronchial or pulmonary hemorrhage.
- Hem/o means “blood,” and –ptysis means “coughing.”
- This can occur due to injury, a tuberculosis infection, or some neoplasm
Lack of Oxygen
- There are many disorders that can cause a lack of oxygen, and many terms to describe the various states of lack of oxygen.
- Anoxia is the total absence of oxygen from the body’s tissues and organs even if there is sufficient blood flow to that tissue or organ. Oxygenation must be restored within 4-6 minutes to avoid irreversible brain damage. An- means “without,” and –oxia means “pertaining to oxygen.”
- Hypoxia is a state of deficient oxygen in the body’s tissues or organs. This can be caused by a number of diseases, or environmental conditions such as carbon monoxide poisoning or high altitude. Hypo- means “beneath”
- Altitude hypoxia, or altitude sickness, occurs when there is a decrease in oxygen levels. This often occurs around 8,000 feet and above.
- Hypoxemia is the state of deficient oxygen in the blood. This can occur due to heart conditions or respiratory disorders.
- Hyp/o means “beneath,” ox/y means “oxygen,” and –emia means “blood condition.”
- Cyanosis is a bluish discoloration of the skin and mucous membranes due to a lack of sufficient oxygen. Generally, cyanosis is first seen around the lips, nails, and eyes.
- Cyan/o means “blue,” and –osis means “condition.”
- Hypercapnia is the buildup of carbon dioxide in the blood.
- Hyper- means “excessive,” capn/o means “carbon dioxide,” and –ia means “condition.
Lack of Oxygen: Disorders
- Airway obstruction is also called choking, and is the physical blockage of the airway by food or a foreign object. This requires immediate care in the form of the Heimlich maneuver, in which abdominal thrusts are applied in an attempt to force the obstruction away.
- Asphyxia is a loss of consciousness caused by insufficient oxygenation to the body. Asphyxiation (or the state of asphyxia) can be caused by choking, suffocation, drowning, or inhaling gases.
- Smoke inhalation is damage to the lungs caused by smoke, where the alveoli are coated by particles that prevent the exchange of oxygen and carbon dioxide.
- Respiratory failure is also called respiratory acidosis, and occurs when the levels of oxygen in the blood become dangerously low, and the levels of carbon dioxide become dangerously high. This can be due to a chronic condition or can happen acutely (or suddenly).
Sudden Infant Death Syndrome
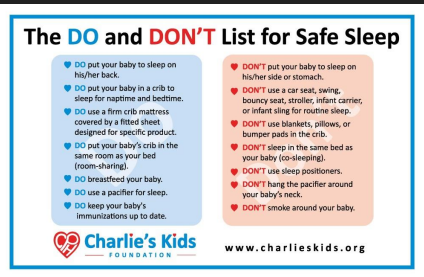
- Sudden infant death syndrome (SIDS) is the sudden death of an infant between 2 and 6 months of age.
- The cause of SIDS is unknown, but public education campaigns such as “Safe to Sleep” has decreased the incidence of SIDS in the United States.
%%Begginning of PP #4%%
Diagnosis and Treatment of the Respiratory System
Medical Professionals
- A pulmonologist is a physician who specializes in the diagnosis and treatment of respiratory system disorders.
- Pulmon/o means “lung,” and –ologist means “expert.”
- A thoracic surgeon is a physician who performs surgeries on the structures of the chest, including the heart, lungs, and esophagus.
- An otolaryngologist is also known as an ear, nose, and throat specialist, or ENT, and is a physician who specializes in diagnosing and treating disorders of the head and neck.
- Ot/o means “ear,” laryng/o means “larynx,” and –ologist means “expert.”
- A respiratory therapist is a licensed medical professional that provides respiratory treatments to patients.
Diagnostic Procedures: Noninvasive
- The respiratory rate is the first diagnostic procedure performed regarding the respiratory system, since it is performed during the initial vital signs assessment. It is defined as the number of breaths per minute (one full inhalation and one full exhalation).
- Respiratory sounds are also discovered during the patient assessment, and are sounds such as rales, rhonchi, and stridor that give information about the state of the lungs.
- A spirometer is a device that records the volume of air inhaled and/or exhaled, and time required for each breath.
- Spir/o means “breathing,” and –meter means “a device used to record.”
- An incentive spirometer is used with patients that have had surgery recently, and helps expand the lungs to keep them working well after surgery.
- Pulmonary function tests are tests that measure the amount of air and its flow using a spirometer. The patient’s results are tested against normal ranges for that person’s age, sex, and height.
- A peak flow meter is a handheld device that measures the air flowing out of the lungs. This is often used for patients with asthma, so they can detect changes in the narrowing airways before an asthma attack.
- Pulse oximetry is an extremely important method of determining the levels of oxygenation in the tissues. It uses a small external device called a pulse oximeter, which is placed on the patient’s finger or earlobe. This provides an objective measurement of the oxygen saturation of the blood.
- Sputum cytology is performed to detect cancer cells under a microscope. The sputum specimen is coughed up from the lungs.
- Phlegm is the thick mucus secreted by the tissues lining the respiratory system, and sputum is phlegm that has been expelled through the mouth.
- Polysomnography is also called a sleep study, and uses physiological measurements of the body during sleep to detect changes in breathing associated with sleep apnea.
- Poly- means “many,” somn/o means “sleep,” and –graphy means “the process of creating a record.
More Invasive Diagnostic Procedures
- A chest X-ray is an x-ray technique that is used to diagnose problems with the lungs, including lung cancer, pneumonia, a pleural effusion, a pneumothorax, tuberculosis, and emphysema.
- A bronchoscopy is the visual examination of the bronchi using a bronchoscope, which is passed through the nose or mouth and down the airways. Operative procedures may also be performed during the bronchoscopy. Bronch/o means “airway,” and –scopy means “the process of looking.”
- A laryngoscopy is the visual examination of the larynx and/or vocal cords using a laryngoscope, which may be either flexible or rigid.
- Laryng/o means “larynx,” and –scopy means “the process of looking.”
- Indirect laryngoscopy is less invasive, and is performed by shining a light at the back of the soft palate.
- Tuberculosis can be detected using one of two screening methods:
- A tuberculosis skin test is performed by injecting a very small amount of purified protein derivative of tuberculin
under the skin and examining for a reaction 48-72 hours later. - A quantiferon blood test may be performed, which provides a less subjective result.
- Neither method will reveal whether an infection is active or latent; a chest x-ray must be performed to determine the type of infection if the screening tests are positive.
Medications
- Medications used to treat the respiratory system disorders are aimed at increasing the amount of oxygen that the body can take in.
- Asthma medications:
- A bronchodilator is a medication that relaxes and expands the bronchial passages into the lungs. Short-acting bronchodilators are used to treat acute asthma attacks, and longacting bronchodilators are used daily to help control asthma. These are also called rescue medications.
- Bronch/o means “airway,” and dilate means “to expand.”
- Controller medications are those taken daily, and are sometimes inhaled corticosteroids. They stop the lungs from reacting to the factors that trigger asthma.
- A metered-dose inhaler provides a specific amount of medication, which is combined with a gas propellant to push it into the lungs.
- A nebulizer is a device that pumps the medication into the lungs by mixing it with air or oxygen to turn it into a mist, which is inhaled by the patient.
- An antitussive is a medication that prevents or relieves coughing.
Treatments of the Upper Respiratory Tract
- A functional endoscopic sinus surgery is a procedure performed with an endoscope, which enlarges the opening between the nose and sinus cavity to treat chronic sinusitis.
- A laryngectomy is the surgical removal of the larynx.
- Laryng/o means “larynx,” and – ectomy means “the surgical removal.”
- A laryngotomy is the surgical incision into the larynx, which is performed when the upper part of the airway is obstructed. Endotracheal intubation is performed to establish or maintain an airway, especially when a patient is on a ventilator. This is done by passing a tube through the mouth into the trachea.
- –otomy means “surgical incision”
- A septoplasty is the surgical repair of the nasal septum, or the alteration of parts that need to be repaired.
- Sept/o means “wall,” and –plasty means “the surgical repair.”
- A tracheostomy is the surgical creation of a stoma into the trachea to insert a tube to facilitate breathing. This can be permanent or temporary. The term tracheostomy refers to both the procedure and the stoma. If you recall, a stoma is a surgically created opening on a body surface.
- Trache/o means “trachea,” and –stomy means “the creation of an opening.”
- A tracheotomy is an emergency procedure in which an incision is made into the trachea to provide an airway when the upper part of the trachea is blocked.
Treatments of the Lower Respiratory Tract
- Video-assisted thoracic surgery is the use of a specialized endoscope for the thorax called a thoracoscope to visualize the inside of the thoracic cavity with minimal incisions. Biopsies and small surgeries may also be performed using this type of surgical procedure.
- Thoracentesis is the removal of fluid from the pleural cavity through a surgical puncture of the chest wall with a needle. Fluid or air may be removed using this procedure.
- –centesis means “a surgical puncture to remove fluid.”
- A thoracotomy is the surgical incision of the chest wall to open the thoracic cavity. This will give the surgeon access to the lungs, heart, and other structures of the thoracic cavity.
- A penumonectomy is the surgical removal of all or part of a lung.
- Pneum/o means “lung,” and –ectomy means “the surgical removal.”
- A lobectomy is the removal of lobe of an organ, especially the brain, lung, or liver.
- A wedge resection is performed to surgically remove a small piece of cancerous tissue along with some healthy tissue around the margins.
Respiratory Therapy
- Diaphragmatic breathing is a breathing technique used to relax a patient and help relieve anxiety.
- A ventilator is a mechanical device that is used to replace or supplement the patient’s natural breathing pattern, providing artificial respiration. The machine forces air into the lungs, and exhalation occurs as the lungs naturally contract.
- A bag valve mask, or Ambu bag, is an emergency resuscitator mask used to help with patient ventilation. An air chamber is squeezed to force air through the mask and into the patient’s lungs.
- A continuous positive airway pressure (CPAP) machine is a mask connected to a pump that provides constant air pressure to hold the airway open, decreasing the amount of apnea disturbances through the night.
- A bilevel positive airway pressure (BiPAP) machine is similar to a CPAP machine, but can be set at a higher pressure for inhalation and lower pressure for exhalation.
Oxygen Therapy
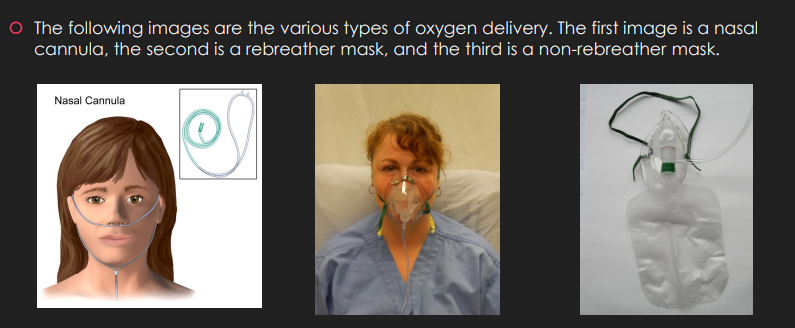
- Supplemental oxygen is oxygen that is administered to help a patient regain or maintain adequate oxygen saturation. The oxygen is administered through a compressor and delivered to the patient through one of the following:
- A nasal cannula is a small tube that divides into nasal prongs, one of each inserted into a nostril.
- A rebreather mask is a mask that allows the exhaled breath to be reused, which delivers up to
60% oxygen. - A non-rebreather mask is a mask that delivers higher levels of oxygen to the patient.
- Hyperbaric oxygen therapy uses a specialized chamber that allows air pressure to be raised to up to 3 times the normal amount. The patient breathes pure oxygen, and the increase air pressure allows the lungs and blood stream to absorb more oxygen. This increased oxygenation helps to fight infection and promote healing. Hyperbaric chambers were used frequently to help treat polio infections.