Endocrine, Blood, Heart, Lymphatic, and Respiratory System Study Notes
Posterior Pituitary Hormones
Hormones stored in posterior pituitary and produced by hypothalamus: ADH (antidiuretic hormone) and oxytocin.
These are not synthesized in the posterior pituitary itself; they are made in the hypothalamus and transported/stored in the posterior pituitary for release when needed.
Anterior Pituitary Hormones
Anterior pituitary secretes six major hormones:
TSH (thyroid-stimulating hormone)
ACTH (adrenocorticotropic hormone)
LH (luteinizing hormone)
FSH (follicle-stimulating hormone)
GH (growth hormone)
PRL (prolactin)
TINY ANTS LOVE FRESH GREEN PLANTS
Hypothalamic releasing hormones (examples mentioned): GnRH (gonadotropin-releasing hormone; GRH in the talk), TRH, CRH, GHRH, somatostatin (not listed in talk but relevant for regulation).
LH and FSH are gonadotropins; they are stimulated by GnRH from the hypothalamus.
Adrenal Glands: Cortex vs Medulla
Adrenal medulla (inside) produces catecholamines:
Epinephrine (adrenaline)
Norepinephrine (noradrenaline)
These medullary hormones mediate fight-or-flight effects: ↑ heart rate, bronchodilation, vasodilation in some vessels, etc.
Adrenal cortex (outside) produces steroid hormones:
Mineralocorticoids (e.g., aldosterone): promotes Na+ reabsorption and shifts water retention, leading to increased blood pressure.
Glucocorticoids (e.g., cortisol): regulates glucose metabolism, interacts with insulin, affects blood sugar; stress response; anti-inflammatory actions.
Androgens/sex hormones (gonadocorticoids).
Key regulatory hormone: ACTH (from anterior pituitary) stimulates cortisol production in the cortex; ACTH is activated by CRH from hypothalamus.
Clinical connections: excessive or deficient cortisol leading to Cushing’s syndrome or Addison’s disease.
Thyroid, Parathyroid, and Calcium Regulation
Calcitonin (from thyroid) and parathyroid hormone (PTH) regulate blood calcium in opposition (antagonists):
PTH raises blood calcium (hypocalcemic to hypercalcemic balance via bone resorption, kidney reabsorption, and vitamin D activation).
Calcitonin lowers blood calcium.
Note from transcript: there was a quick mix-up naming the regulator source; standard physiology is PTH from parathyroids and calcitonin from thyroid, not hypothalamus.
Other calcium-related hormones often discussed with thyroid include TSH (thyroid-stimulating hormone) and its role in thyroid hormone production, which indirectly affects metabolism and calcium handling via overall systemic effects.
Blood: Composition, Cells, and Blood Types
Blood composition: Plasma is the liquid component and is the most abundant portion of blood; typically about 55% of whole blood; the remaining ~45% are formed elements (red cells, white cells, platelets).
Representation from transcript: plasma is the largest component; percentage discussions reflect typical hematology knowledge.
Red blood cells (RBCs) carry oxygen via hemoglobin (Hb). The molecule responsible for oxygen transport on RBCs is hemoglobin.
Leukocytes (white blood cells) are involved in immune defense.
Coagulation cascade (blood clotting): Involves intrinsic and extrinsic pathways converging on the common pathway.
Common pathway components include factors X, II (prothrombin), V, and I (fibrinogen), leading to formation of thrombin and fibrin.
A representative schematic:
ext{Prothrombin (II)} o ext{Thrombin (IIa)} ext{ via } ext{Prothrombinase}(Xa+Va)
ext{Fibrinogen (I)} o ext{Fibrin} (Ia) ext{ via } ext{Thrombin}
ABO blood types (antigens and antibodies):
Type O: has antibodies against A and B; no A/B antigens.
Type AB: has all A and B antigens; no anti-A or anti-B antibodies; universal recipient for RBCs.
Type A: has A antigens; anti-B antibodies.
Type B: has B antigens; anti-A antibodies.
Heart: Anatomy, Conduction, and Vessels
Cardiac apex location: commonly taught as the left 5th intercostal space at the midclavicular line; the transcript shows a student answer of “bottom left,” which is a simplified memory cue but not the precise anatomical landmark.
Sulci (grooves) of the heart:
Interventricular sulcus (groove between left and right ventricles).
Interatrial sulcus/atrioventricular grooves separate atria from ventricles and mark coronary vessels.
Atria and auricles (ears): the atrial appendages are called auricles (horseshoe-shaped pockets).
Foramen ovale: fetal opening between the right and left atria that normally closes after birth.
Electrical conduction order (pacemaker-to-pump):
SA node → AV node → AV bundle (bundle of His) → bundle branches → Purkinje fibers.
The transcript shows student confusion; the correct sequence is SA node -> AV node -> AV bundle -> bundle branches -> Purkinje fibers.
Blood flow vs. electrical system interplay is emphasized for nursing practice; nurses often monitor or manage devices that interact with these conduction pathways.
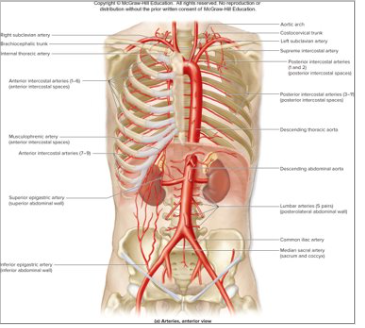
Major vessels and heart vessels:
Elastic (conducting) arteries near the heart (e.g., the aorta) are large and elastic.
As arteries move away from the heart, they become smaller (arterioles).
Veins generally increase in size as they return to the heart.
Tunica layers: tunica media (muscular middle layer), tunica intima (innermost), tunica externa/adventitia.
The hilum (MIDDLE) of the lungs is the mediastinal region where bronchi, pulmonary arteries, and veins enter/exit the lungs.
Lungs and respiration anatomy:
Right lung has three lobes; left lung has two lobes (heart occupies space on left side).
Apex of the lung is located high near the clavicle; the apex is susceptible to injury around the collarbone area.
The diaphragm separates thoracic and abdominal cavities; lungs are largely in the thoracic cavity.
Larynx, trachea, bronchi, and zones:
Larynx (voice box) sits above the trachea.
Trachea leads to bronchi; terminal bronchioles lead into respiratory zones.
Conducting zone: from nose down to terminal bronchioles; no gas exchange.
Respiratory zone: respiratory bronchioles, alveolar ducts, and alveoli where gas exchange occurs.
Lung structure and perfusion concepts:
Alveoli are more numerous at the bases due to gravity-driven perfusion differences; upright individuals have better perfusion at the bases than the apices.
Smoking or inactivity can reduce perfusion efficiency and alveolar ventilation distribution.
Ear-to-nose connection: the auditory (Eustachian) tube connects the middle ear to the nasopharynx; risk of middle ear infections increases with swimming and nasopharyngeal pressure changes.
Lymphatic System and Immunity
Lymph basics: lymph is mostly water-based, with proteins and occasional pathogens; it can contain lipids in chyle.
Lymphatic vessels are closed-ended tubes; lacteals are lymphatic vessels in the small intestine that absorb dietary lipids (fat absorption).
Peyer’s patches (referred to as parapatches in the transcript) are lymphoid tissues in the small intestine that contribute to gut immunity.
MALT: Mucosa-associated lymphoid tissue; lymphoid tissue associated with mucosal surfaces (any mucus membranes).
Lymphatic function: lymphatic drainage is driven by hydrostatic/pressure gradients and tissue dynamics.
Thymus: location and anatomy: located in the mediastinum; typically described as having two lobes.
Lymphocyte maturation: standard immunology states that B cells mature in bone marrow and T cells mature in the thymus.
Immune defense structure: 3 tiers often discussed in nursing:
First line of defense: physical barriers (skin) and mucous membranes.
Second line of defense: innate immune responses (complement system, inflammation).
Third line of defense: adaptive immunity (antigen-specific responses).
Complement pathways:
Classical pathway requires antigen presentation to initiate.
Alternative pathway can activate more directly to promote effector functions.
Inflammation: classic cardinal signs are redness, heat, swelling, pain, and loss of function.
Immunity types:
Innate vs adaptive; acquired (active) immunity vs passive immunity.
Vaccines provide acquired immunity and training of the immune system to recognize specific antigens.
Respiratory System: Conducting vs Respiratory Zones
Upper vs lower respiratory tract definitions:
Upper tract includes nasal cavity, pharynx, larynx up to the vocal cords.
Lower tract includes trachea, bronchi, bronchioles, and lungs.
Conducting zone vs respiratory zone:
Conducting zone: cleans, humidifies, and transports air; no gas exchange.
Respiratory zone: sites of gas exchange (alveoli and respiratory bronchioles).
Larynx and pharyngeal anatomy: the larynx is the voice box; following it is the trachea.
Lung lobes and mediastinal context: as noted, right lung has three lobes; left lung has two due to heart position.
Pleura and lung support fundamentals (briefly implied): lungs are encased within pleural cavity, separated from the chest wall by pleurae.
Practical nursing notes:
Understanding apex vs base, lobes, hilum, and major vessels is essential for interpreting imaging and planning procedures (e.g., catheterization, chest tube placement).
Quick Connections and Clinical Takeaways (Integrated insights)
Endocrine–metabolic links:
Cortisol and glucose metabolism interact with insulin; cortisol elevation can raise blood glucose; stress affects glucose control.
Aldosterone’s mineralocorticoid action increases Na+ retention, which can elevate blood pressure; relevant in hypertension management.
ADH/vasopressin: excess (SIADH) causes water retention and potential hyponatremia; deficiency leads to polyuria and dehydration risk.
Blood and clotting relevance:
ABO compatibility is critical for transfusions; mismatches can trigger severe immune reactions.
The coagulation cascade converges on the common pathway (X, II, I, V) to form a fibrin clot; proper balance prevents bleeding or thrombosis.
Cardiac and pulmonary integration:
The left ventricle’s apex and ventricular wall mechanics relate to electrical conduction and mechanical pumping; conduction system integrity ensures synchronized contraction.
Gas exchange depends on alveolar surface area and perfusion distribution; bases typically have higher perfusion than apices in upright individuals.
Immunology and infection control:
Distinguishing innate vs adaptive immunity helps in understanding vaccines, infections, and inflammatory responses.
Lymphatic drainage and lymphoid tissues (MALT, Peyer’s patches, thymus) are central to mucosal defense and systemic immunity.
Fetal vs postnatal circulation:
Foramen ovale is a fetal opening that normally closes after birth; persistence can affect hemodynamics.