Workshop 6: Muscle Physiology Notes
Learning Objectives and Overview of Muscle Tissues
Compare and contrast the three basic types of muscle tissue.
Describe the gross structure of a skeletal muscle.
Describe the microscopic structure and functional roles of the myofibrils, sarcoplasmic reticulum, and T tubules of skeletal muscle fibers.
Describe the sliding filament model of muscle contraction.
Explain how muscle fibers are stimulated to contract by describing events that occur at the neuromuscular junction.
Follow the events of excitation-contraction coupling that lead to cross bridge activity.
Define motor unit and muscle twitch.
Explain how smooth, graded contractions of a skeletal muscle are produced.
Differentiate between isometric and isotonic contractions.
Describe the length-tension relationship.
Describe the 3 muscle fibre types and when you would use them.
Describe the different lever systems (covered in lab).
Three Types of Muscles
Skeletal muscles
Produce movement of the skeleton.
Are striated and voluntary.
Cardiac muscles
Specialized fibers found in the heart.
Striated branching fibers, involuntary.
Smooth muscles
Found in the tubes and cavities of the body (arterial walls, gut, bladder, uterus), involuntary.
Unstriated (therefore called smooth).
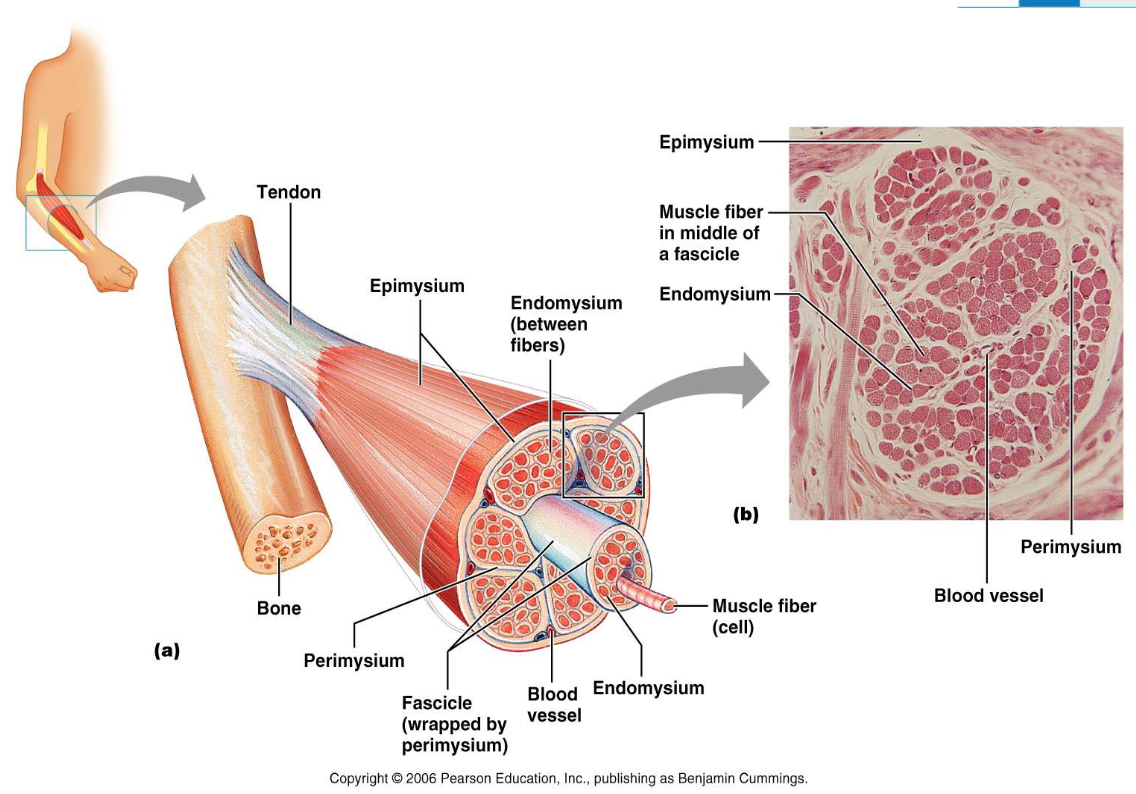
Organization of Muscle Connective Tissue
Named according to its relationship with the muscle fibres.
Continues as tendon.
Epimysium: Covers the whole muscle.
Perimysium: Covers muscle fascicle (bundle).
Endomysium: Covers only one muscle fibre (myofibre) (one muscle cell).
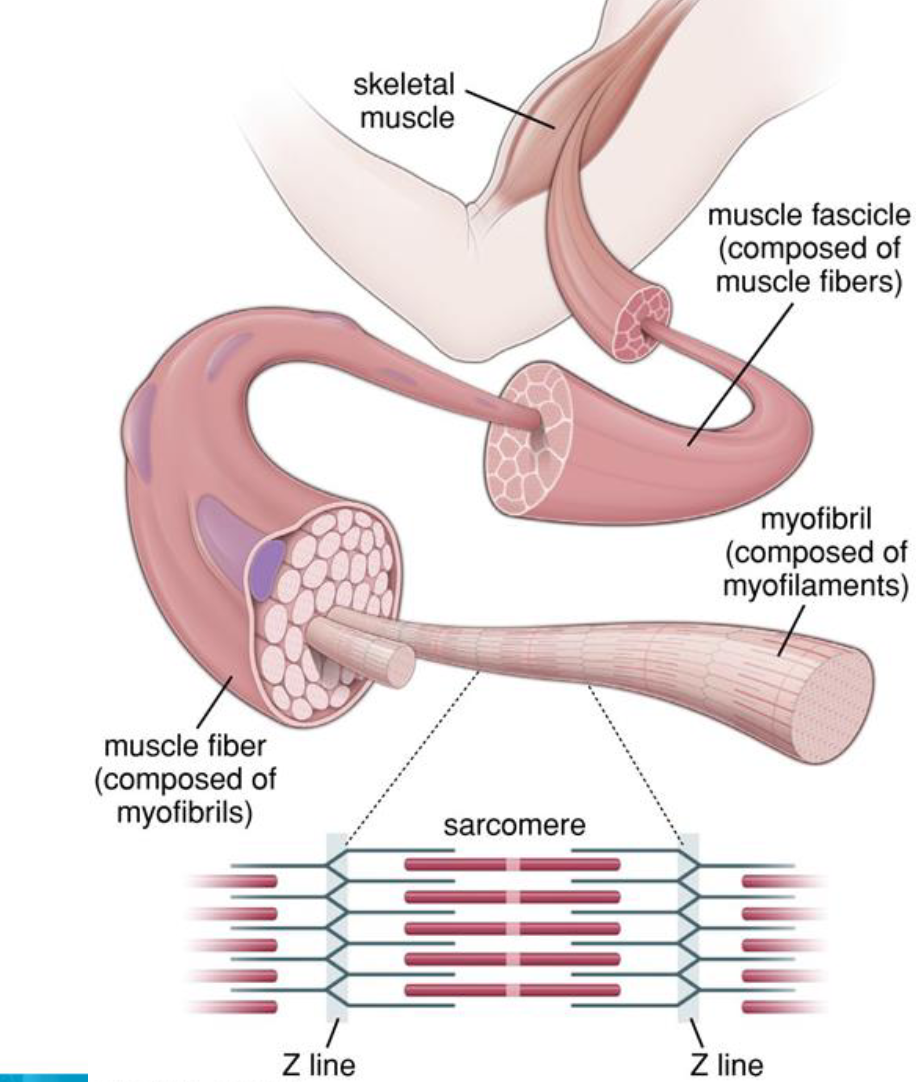
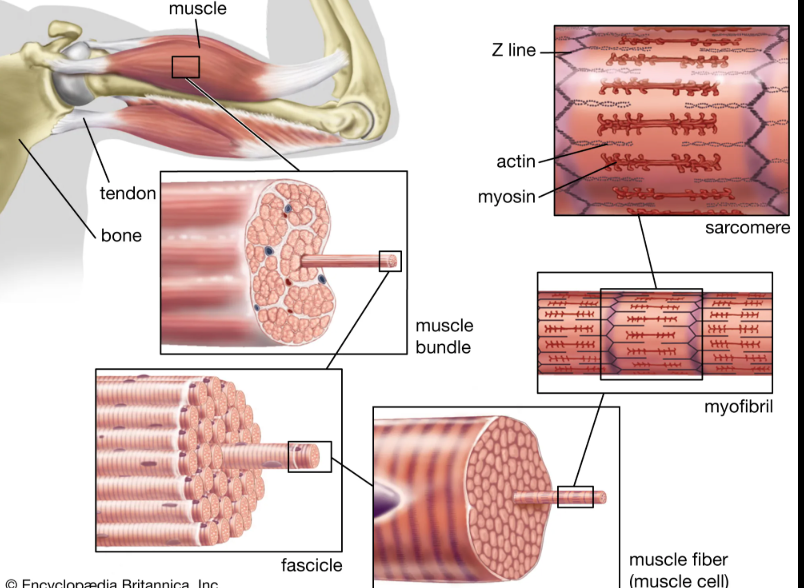
Muscle Structure
Whole muscle (organ)
Muscle fascicle
Muscle fibre (cell)
Myofibril (a specialised intracellular structure)
Thick and thin filaments (cytoskeletal elements)
Myosin and actin (protein molecules)
The Muscle Fibre (Cell)
Each fibre is a long, striated, cylindrical cell with multiple nuclei beneath the sarcolemma.
Sarcolemma: The cell membrane of a muscle fibre.
Sarcoplasm: The cytoplasm of muscle cell.
Myofibril: Rod-like contractile element, spans the cell length, comprises 80% of the volume of the muscle fibre.
Myofilaments: Include the thick filament MYOSIN & the thin filament containing ACTIN, TROPONIN & TROPOMYOSIN. Causes the striated appearance of skeletal muscle.
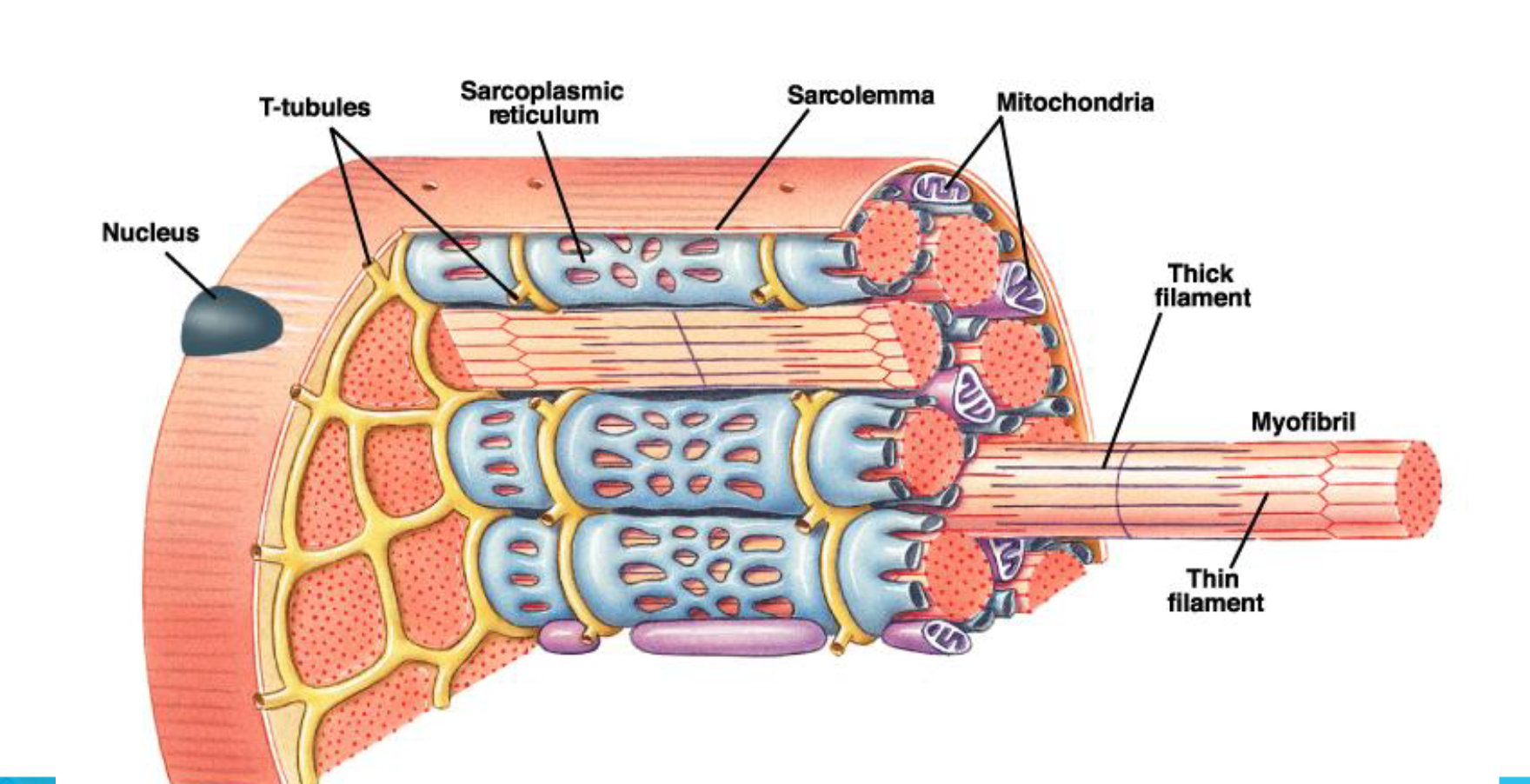
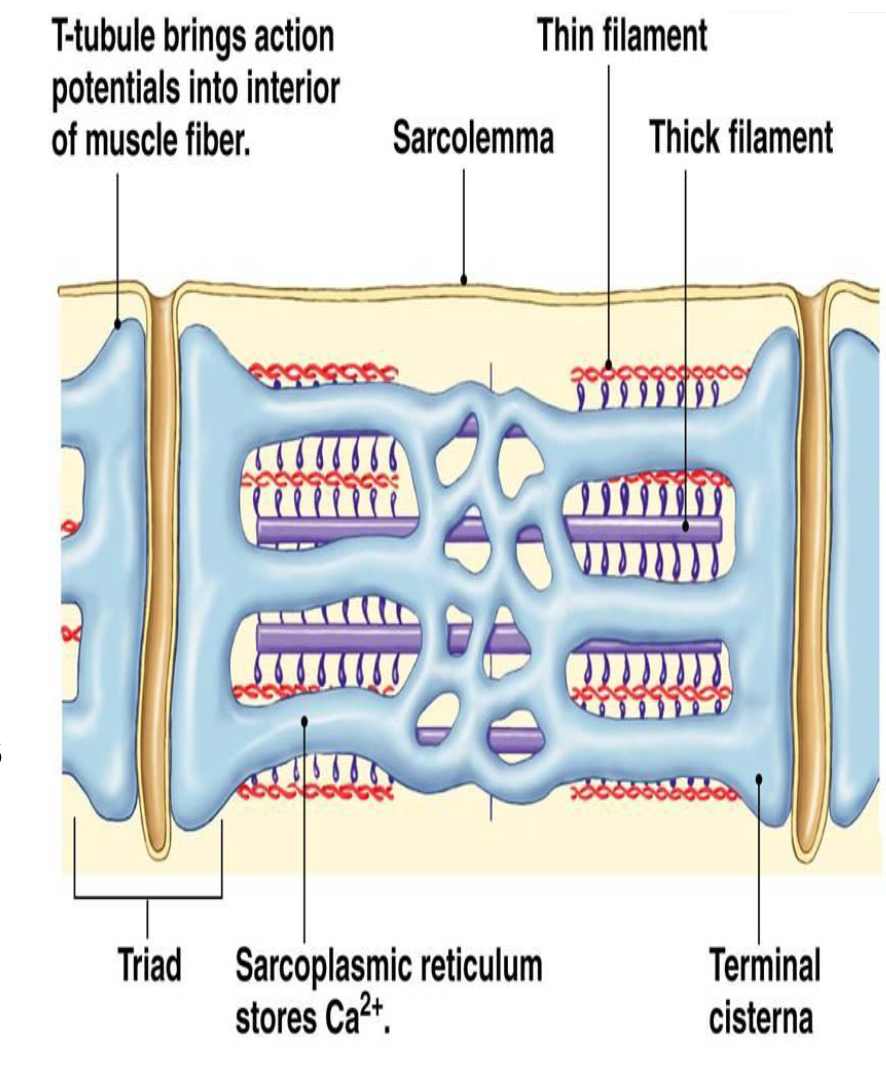
Intracellular Spaces Surrounding Myofibrils
Transverse Tubules (t-tubules):
Extend into muscle cells from the sarcolemma & consist of membrane-lined channels.
Bring the action potential into the interior of the muscle fibre.
Sarcoplasmic Reticulum:
Interconnected sacs and tubes that surround each myofibril.
Come into close contact with t-tubules.
Terminal cisternae (bulges) on either side form a triad.
Stores calcium when the muscle fibre is relaxed.
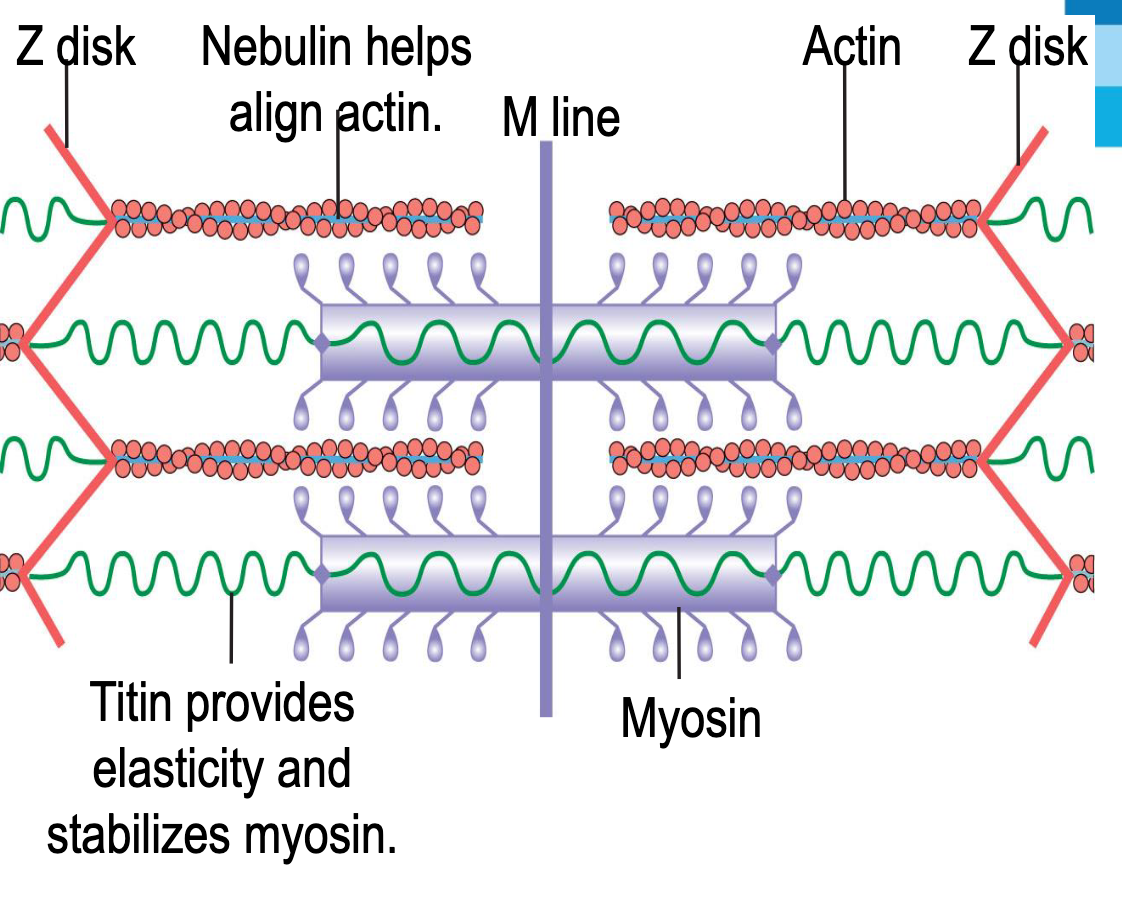
Sarcomere
Titin: Elastic proteins that run through the thick filaments, beginning at the M lines, and ending at the Z discs.
Stabilise the position of each thick filament within the sarcomere and serve as elastic elements that help muscles return to their resting length.
Actin: Nebulin helps align actin.
Myosin and Actin
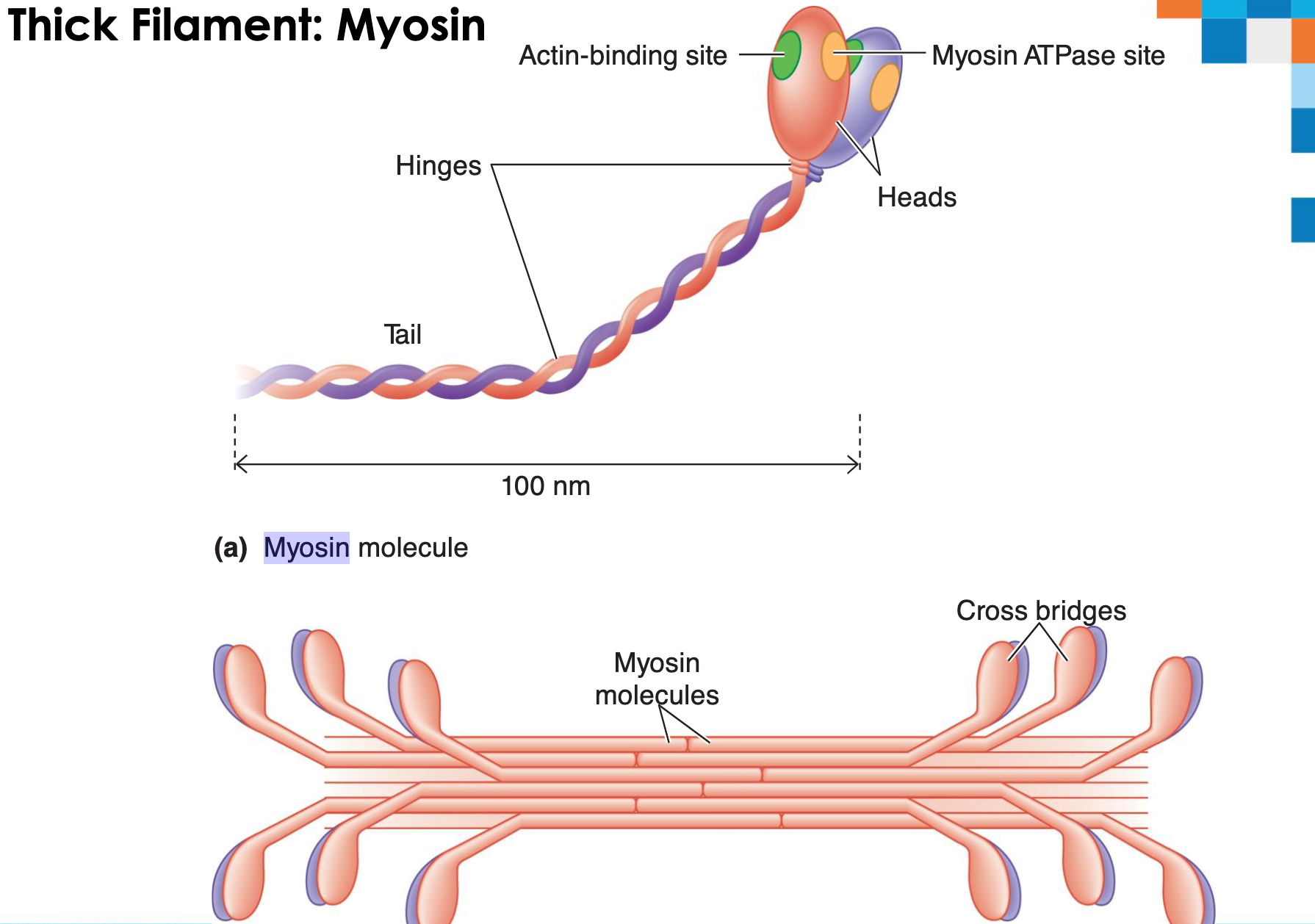
Myosin forms thick filaments.
Protein consisting of two identical subunits, each shaped somewhat like a golf club.
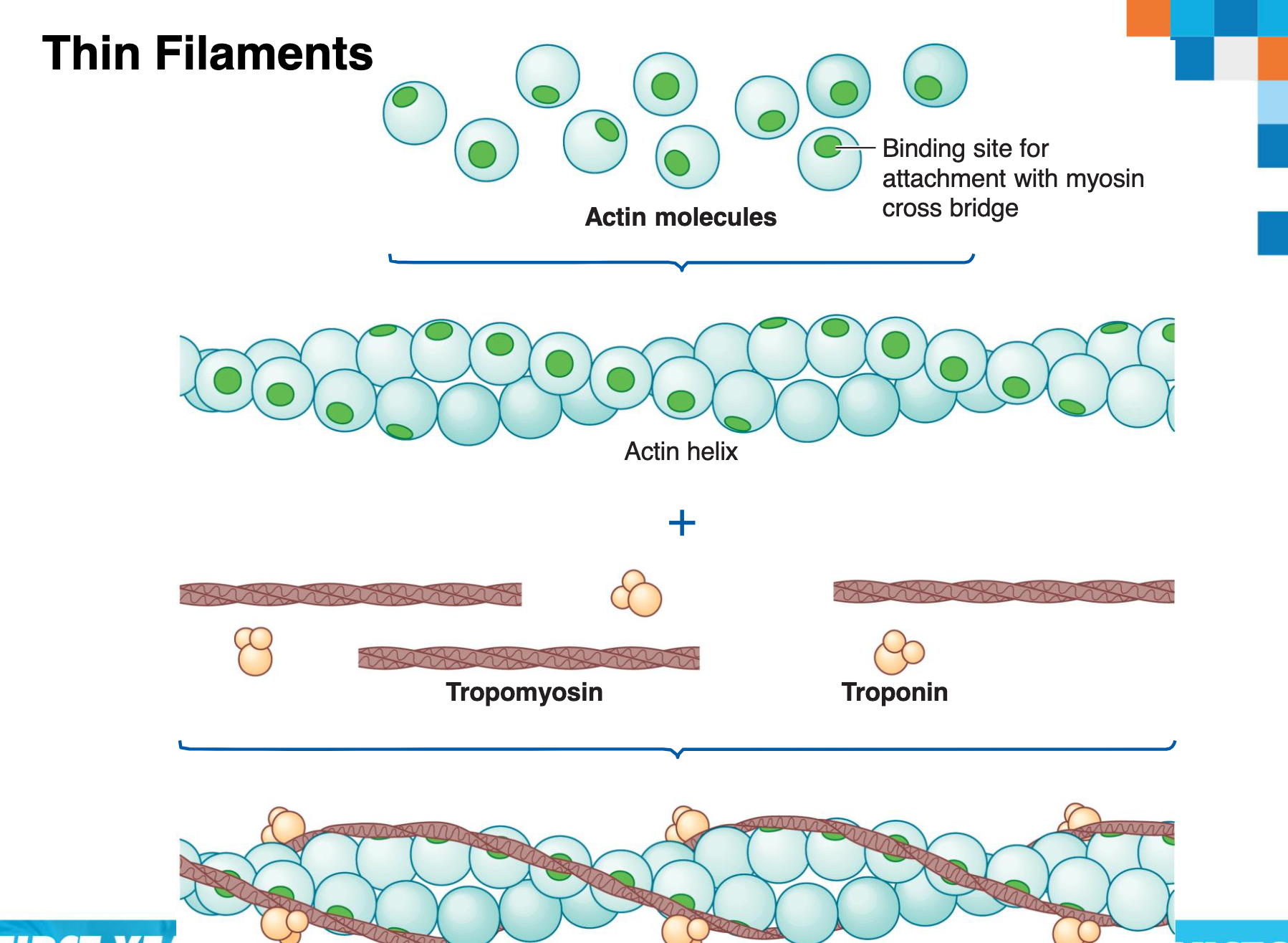
Actin is the main structural component of thin filaments.
Interacts with the myosin cross-bridges.
Two other proteins, tropomyosin and troponin, lie across the surface of actin.
Thick Filament: Myosin
Myosin molecule structure showing heads, hinges, tails, actin-binding site, and myosin ATPase site.
Myosin molecules form cross bridges.
Thin Filaments
Actin molecules form an actin helix.
Tropomyosin and troponin are also present.
Binding site for attachment with myosin cross bridge.
Muscle Contraction
There are two elements to muscle contraction:
The neuromuscular junction – where a nerve stimulates a muscle cell to initiate contraction.
Muscle contraction/’Sliding filament theory’ – how the muscle creates a contraction.
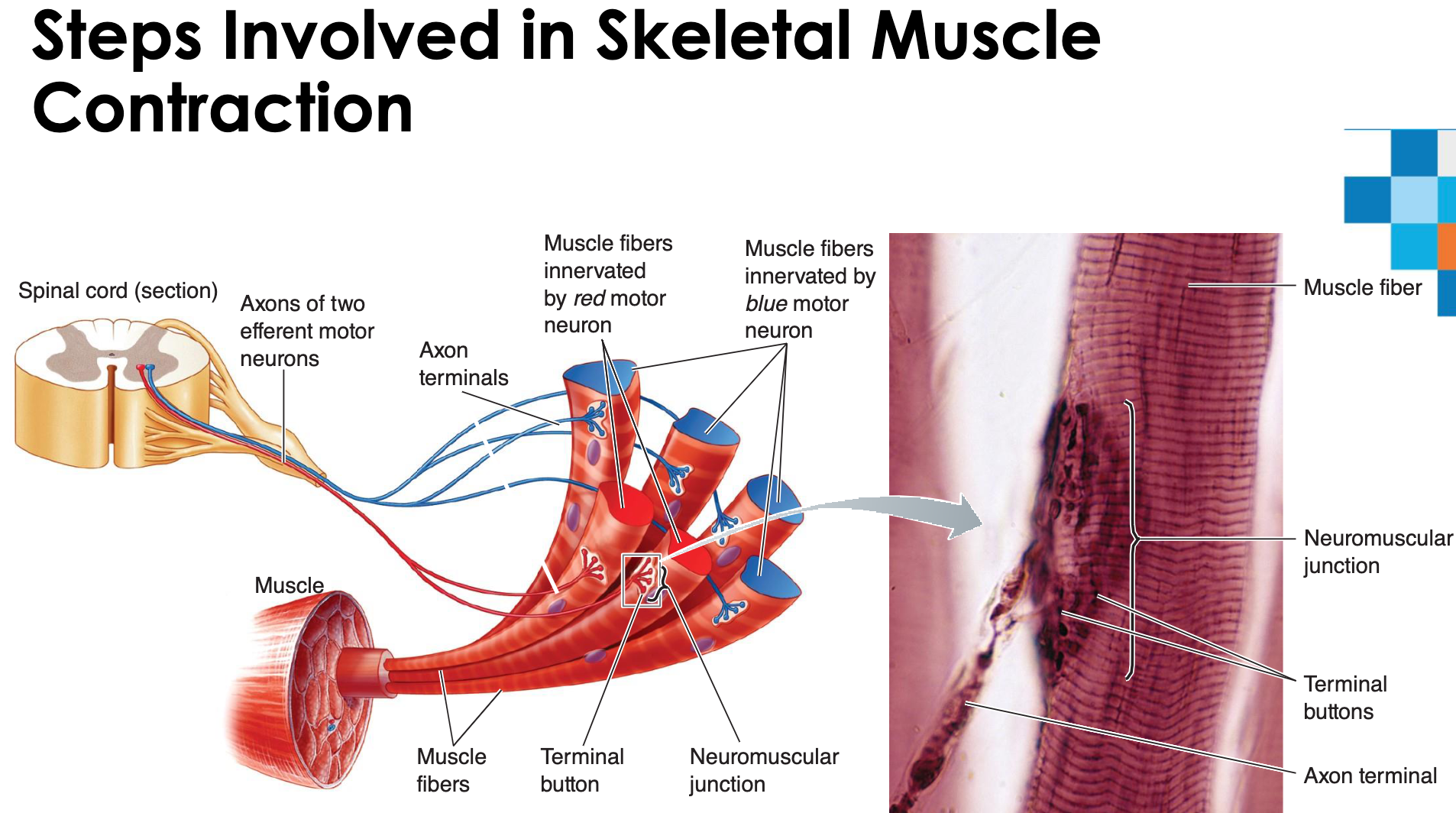
The Neuromuscular Junction
Motor neurons and skeletal muscle fibers are chemically linked at neuromuscular junctions.
Each muscle cell has only one neuromuscular junction.
Muscle fiber: single, long, and cylindrical muscle cell.
Terminal button: enlarged knoblike structure at the end of axon terminal branches.
Motor end plate: shallow depression where axon terminals end.
Release of the neurotransmitter ACh at the neuromuscular junction.
Initiation of an action potential in the muscle fibre.
Acetylcholinesterase (enzyme) ends ACh activity at the neuromuscular junction.
Sequence of Events at the Neuromuscular Junction
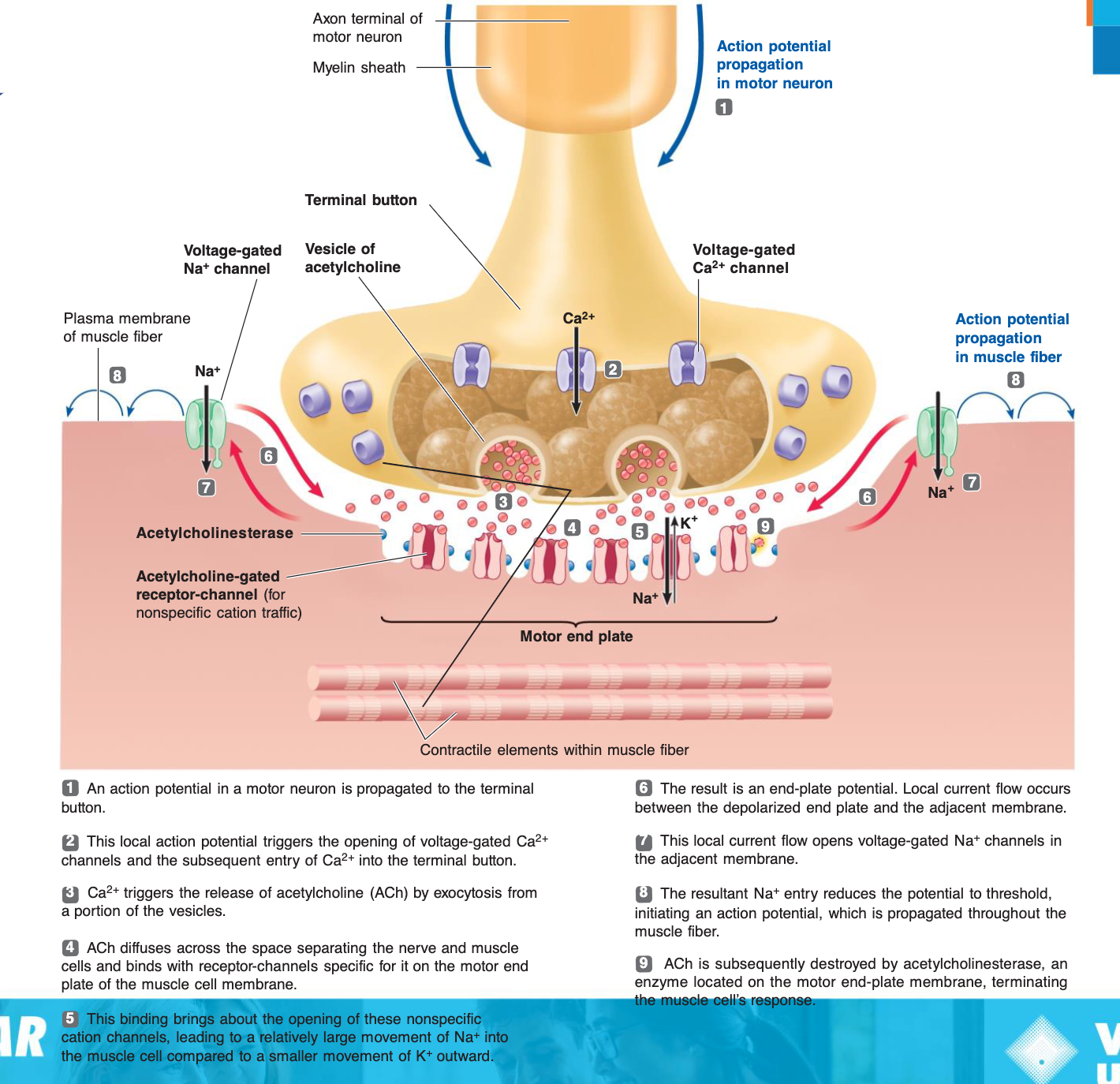
Local Depolarization and Action Potential
Local depolarization leads to the generation of the end plate potential on the sarcolemma.
Generation and propagation of the action potential (AP).
Repolarization
Depicts the repolarization phase with closed Na^{+} channels and open K^{+} channels.
Excitation-Contraction Coupling
Latent period: Time between AP initiation and the beginning of contraction.
AP is propagated along sarcolemma to T tubules.
Voltage-sensitive proteins stimulate Ca^{2+} release from SR: Ca^{2+} is necessary for contraction.
Steps in E-C Coupling
Action potential is propagated along the sarcolemma and down the T tubules.
Calcium ions are released from the terminal cisternae of the sarcoplasmic reticulum (SR).
Calcium binds to troponin and removes the blocking action of tropomyosin.
Contraction begins; myosin binds to actin.
Phases of Muscle Fiber Stimulation
Phase 1: Muscle fiber is stimulated by a motor neuron.
Action potential (AP) arrives at the axon terminal at the neuromuscular junction.
ACh is released and binds to receptors on the sarcolemma.
Ion permeability of the sarcolemma changes, leading to local depolarization (end plate potential).
Local depolarization ignites AP in the sarcolemma, which travels across the entire sarcolemma and along T tubules.
Phase 2: Excitation-contraction coupling occurs.
SR releases Ca^{2+}, which binds to troponin, exposing myosin-binding sites (active sites) on actin.
Myosin heads bi
nd to actin, and contraction begins.
Molecular Basis of Skeletal Muscle Contraction
During contraction, cycles of cross-bridge binding and bending pull thin filaments inward, according to the sliding filament mechanism.
Contraction is accomplished by thin filaments from the opposite sides of each sarcomere sliding closer together between the thick filaments.
Power stroke: Stroking motion pulls the thin filament toward the center of the sarcomere.
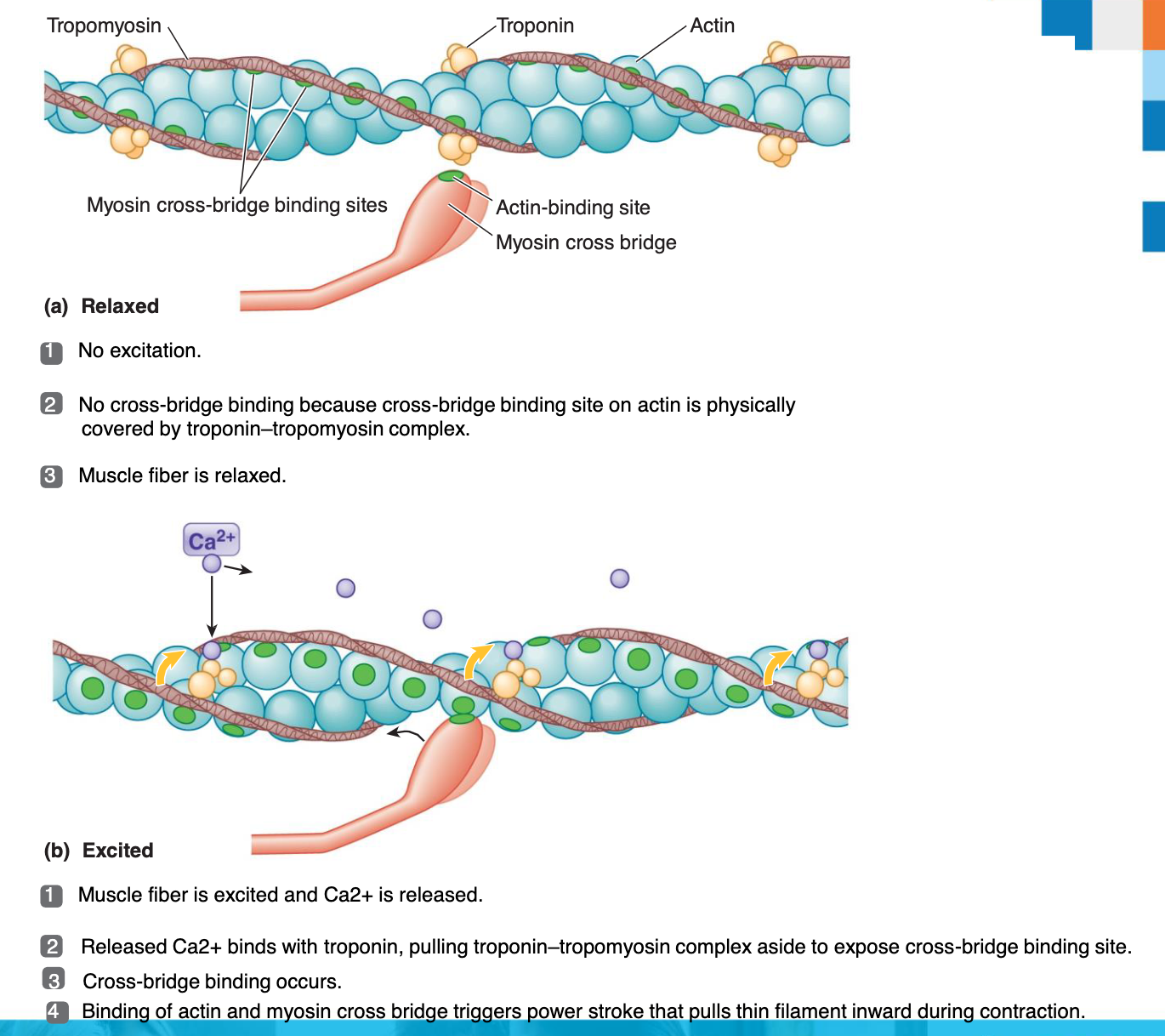
Relaxed vs. Excited Muscle Fiber
Relaxed: No excitation; cross-bridge binding site on actin is physically covered by the troponin–tropomyosin complex.
Excited: Muscle fiber is excited, Ca^{2+} is released, it binds with troponin, pulling the troponin–tropomyosin complex aside to expose the cross-bridge binding site, leading to the power stroke.
Single Cross-Bridge Cycle
Binding: Myosin cross bridge binds to actin molecule.
Power stroke: Cross bridge bends, pulling thin myofilament inward.
Detachment: Cross bridge detaches at end of power stroke and returns to its original conformation.
Binding: Cross bridge binds to more distal actin molecule; cycle repeats.
Cross-Bridge Stroking
All cross-bridge stroking is directed toward the center of the thick filament.
Simultaneous pulling inward of all six thin filaments surrounding a thick filament.
Sarcomere Changes During Contraction
Contracted: Sarcomere shorter, I band shorter, H zone shorter.
Relaxed: Sarcomere, I band, and H zone are at their normal lengths.
A band remains the same width during contraction.
Cross-Bridge Cycle: Detailed Steps
Energized: ATP split by myosin ATPase; ADP and Pi remain attached to myosin; energy stored in cross bridge.
Binding: Ca^{2+} released on excitation removes inhibitory influence from actin, enabling it to bind with cross bridge.
Bending: Power stroke of cross bridge triggered on contact between myosin and actin; Pi released during and ADP released after power stroke.
Detachment: Linkage between actin and myosin broken as a fresh molecule of ATP binds to myosin cross bridge; cross bridge assumes original conformation; ATP hydrolyzed.
Rigor complex occurs if no fresh ATP is available (after death), actin and myosin remain bound.
Comprehensive Overview of Muscle Contraction Steps
An action potential arriving at a terminal button of the neuromuscular junction stimulates the release of acetylcholine, which diffuses across the cleft and triggers an action potential in the muscle fiber.
The action potential moves across the surface membrane and into the muscle fiber’s interior through the T tubules. An action potential in the T tubule triggers the release of Ca^{2+} from the sarcoplasmic reticulum into the cytosol.
Ca^{2+} binds to troponin on thin filaments.
Ca^{2+} binding to troponin causes tropomyosin to change shape, physically moving it away from its blocking position; this uncovers the binding sites on actin for the myosin cross bridges.
Myosin cross bridges attach to actin at the exposed binding sites.
The binding triggers the cross bridge to bend, pulling the thin filament over the thick filament toward the center of the sarcomere. This power stroke is powered by energy provided by ATP.
After the power stroke, the cross bridge detaches from actin. If Ca^{2+} is still present, the cycle returns to step 5.
When action potentials stop, Ca^{2+} is taken up by the sarcoplasmic reticulum. With no Ca^{2+} on troponin, tropomyosin moves back to its original position, blocking myosin cross-bridge binding sites on actin. Contraction stops and the thin filaments passively slide back to their original relaxed positions.
Role of Calcium (Ca^{2+}) in Muscle Contraction
Calcium is the link between excitation and contraction.
Spread of action potential down transverse tubules → Calcium release from sarcoplasmic reticulum → ATP-powered cross-bridge cycling.
Contractile activity far outlasts the electrical activity that initiated it.
At low intracellular Ca^{2+} concentration:
Tropomyosin blocks the active sites on actin.
Myosin heads cannot attach to actin.
Muscle fiber relaxes.
At higher intracellular Ca^{2+} concentrations:
Ca^{2+} binds to troponin.
Troponin changes shape and moves tropomyosin away from active sites.
Events of the cross bridge cycle occur.
When nervous stimulation ceases, Ca^{2+} is pumped back into the SR and contraction ends.
Cross-Bridge Cycle: Detailed Steps
Cross Bridge Cycle Continues as long as the Ca^{2+} signal and adequate ATP are present.
Cross bridge formation: high-energy myosin head attaches to thin filament.
Working (power) stroke: myosin head pivots and pulls thin filament toward M line.
Cross bridge detachment: ATP attaches to myosin head and the cross bridge detaches.
“Cocking” of the myosin head: energy from hydrolysis of ATP cocks the myosin head into the high-energy state.
Muscle Relaxation
AP’s travelling along motor neuron stop.
AP’s in muscle cease.
Ca^{2+} actively transported from sarcoplasm into SR.
Ca^{2+} no longer bound to troponin.
Tropomyosin resumes its blocking function.
Myosin cross bridges cannot reattach to actin, therefore contraction ceases & relaxation occurs.
Activity
Complete your worksheet.
Access the Interactive module named ‘Muscle Physiology H5P’ Week 2 Workshop 6 on VU Collaborate.
Work through the slides by pushing each ‘hot spot’/information button.
Watch the videos to learn how a muscle contracts.
Complete the quiz questions within the module as well as the post class test to test your understanding).
Contractile Strength of Muscle
The strength of muscle contraction depends on:
The number of contracting fibres
The frequency of stimulation
The thickness of each muscle fibre
The initial length of muscle fibres before contraction takes place
Muscle – Functional Unit
The functional unit of muscle is a motor unit.
Consist of a single neuron & the muscle fibres it controls.
May contain 1 or 1000s of muscle fibres.
The number depends on the size and function of the muscle.
When a motor unit in the spinal cord is stimulated it initiates an impulse that causes all the muscle fibres supplied by that motor unit to contract simultaneously.
Motor Unit Illustration
Illustration depicting multiple motor units within a muscle, each consisting of a motor neuron and the muscle fibers it innervates.
The Motor Unit
Whole muscles contracted in a GRADED fashion
Produced by variations in the number of motor units activated
Fine neural control over strength of muscle contraction = many small motor units
e.g. Muscles that position the eye have an average of 23 fibres per neuron/motor unit
Neural control over powerful muscle contraction = large motor units
e.g. Gastrocnemius = 1000 fibres per neuron/motor unit
Muscle Twitch
(a) No summation: If a muscle fiber is restimulated after it has completely relaxed, the second twitch is the same magnitude as the first twitch.
(b) Twitch summation: If a muscle fiber is restimulated before it has completely relaxed, the second twitch is added on to the first twitch, resulting in summation.
(c) Tetanus: If a muscle fiber is stimulated so rapidly that it does not have an opportunity to relax at all between stimuli, a maximal sustained contraction known as tetanus occurs.
The Length-Tension Relationship
Maximum relative tension is achieved when the muscle is 100-120% of resting length.
Sarcomere lengths from 2-2.25{\mu}m
Increases & decreases in muscle (& sarcomere) lengths result in rapid decreases in tension
Length-Tension Relationship Graph
Graph illustrating the relationship between muscle fiber length (compared with optimal length) and percent maximal tension.
Highlights the range of length changes that can occur in the body, from shortened to stretched muscle.
Skeletal Muscle Mechanics
Whole muscles are groups of muscle fibers bundled together and attached to bones.
Tendons attach the muscle to bones.
Muscle tension is transmitted to bone as the contractile component tightens the series-elastic component.
Tension is produced internally within the sarcomeres.
Contractile component of the muscle
Components of Muscle Mechanics
Thick and thin filaments (contractile component) and titin (parallel-elastic component).
Tendon (series-elastic component).
Types of Contraction
Isometric (i.e., constant length): muscle length remains constant as tension increases.
e.g. calf raise and hold
Concentric contractions
Muscle shortens
Eccentric contractions
Muscle lengthens
Isotonic (i.e., constant tension): load remains constant as the muscle lengthens or shortens.
eg, walking, running, squats , push-ups)
Muscle Fibre Types
Muscle fibres classified according to functional characteristics:
Speed of contraction
Characterised by how quickly ATP can be split (myosin ATPase activity)
Slow & fast fibres
Major pathways used for ATP production
Characterised by preferential use of aerobic oxidative phosphorylation or anaerobic glycolysis
Oxidative & glycolytic
Muscle Fibre Types
Fibres mainly classified as:
Slow oxidative (Type I)
Best Suited to endurance-type activity
Fast oxidative (Type IIa)
Best suited to running, walking etc
Fast glycolytic (Type IIb)
Best suited to short-term, intense, powerful movement like hitting a baseball
Muscle Fibre Types: Diagram
Illustrates the different types of muscle fibers (Type I, Intermediate, Type IIB) and their recruitment during early contraction and near exhaustion.
Fast-Twitch Glycolytic and Slow-Twitch Oxidative Muscle Fibers
Table summarizing the characteristics of slow-twitch oxidative, fast-twitch oxidative-glycolytic, and fast-twitch glycolytic muscle fibers including speed of development of maximum tension, myosin ATPase activity, diameter, contraction duration, Ca2+-ATPase activity in SR, endurance, use, metabolism, capillary density, mitochondria, and color.
Video References
Part 1: Events at the Neuromuscular Junction
https://www.youtube.com/watch?v=qccUQGZbyi8
Part 2: Excitation Contraction Coupling
https://www.youtube.com/watch?v=zUUB3nqh79c
Part 3: The Cross Bridge Cycle
https://www.youtube.com/watch?v=sIH8uOg8ddw