NURS 1550- Distribution, Biotranformation, and Excretion of Drugs
NURS 1550- Distribution, Biotranformation, and Excretion of Drugs
Review
- Drug absorption → Into the body
- Drug distribution → Around the body
- Drug metabolism → Biotransformation (changing) of drug
- Drug excretion → Out of body
Review- Absorption
- Movement of a drug from its site of administration into the blood
- The rate of absorption determines how soon effects will begin
- The amount of absorption helps determine how intense the effects will be
- Factors Affecting Drug Absorption
- Rate of dissolution
- Surface area
- Blood flow
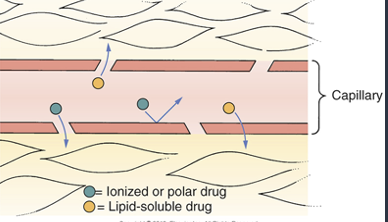
- Lipid solubility
- pH partitioning
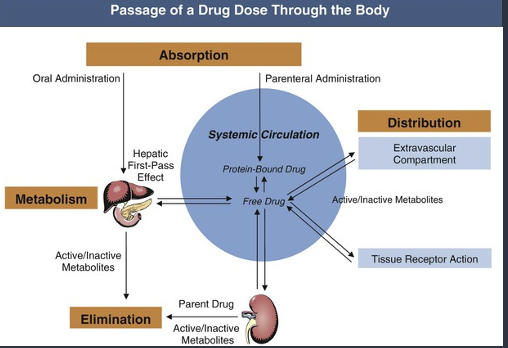
Distribution
- Movement of drugs throughout the body
Exiting the Vacular System
- After a drug has been delivered to organ/tissue, it must exit vasculature
- Typical capillary beds
- Drugs pass between capillary cells rather than through them
Blood Flow to Tissues
- Drugs are carried by the blood to tissues and organs of the body
- Blood flow determines the rate of delivery
- Abscesses and tumors
- Low regional blood flow affects therapy
- Pus-filled pockets rather than internal blood vessels
- Solid tumors have a limited blood supply
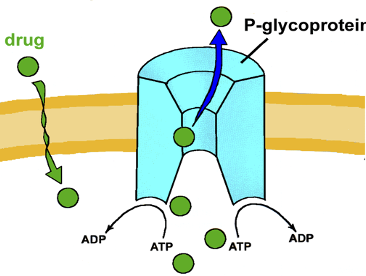
Blood-Brain Barrier
- Tight junctions exist between capillary cells in CNS
- Junctions prevent most drug passage
- Drugs must be able to pass through the cells of the capillary wall
- Drugs must be lipid-soluble or have a transport system to cross BBB
- P-Glycoprotein present in BBB

Placental Drug Transfer
- Membranes of the placenta do NOT inhibit passage of drugs
- Movement determined same way as for other membranes
- Risks with drug transfer
- Decreased mental aptitude, gross malformations, low birth weight
- Mother’s use of habitual opioids: Birth of drug-dependent baby
Protein binding
- Membranes of the placenta do NOT inhibit passage of drugs
- Movement determined same way as for other membranes
- Risks with drug transfer
- Decreased mental aptitude, gross malformations, low birth weight
- Mother’s use of habitual opioids: Birth of drug-dependent baby
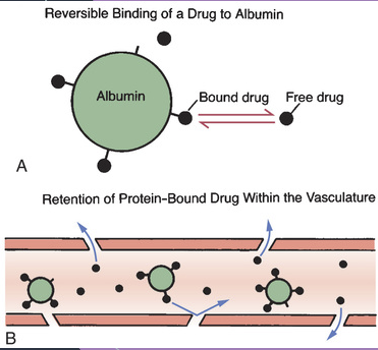
Protein Binding
- Drug reversibly bound to albumin in vasculature
- Can lead to changes in drug concentration
- Some drugs have higher affinity
- Competition for sites
Entering Cells
- Some drugs must enter cells to reach the site of action
- Most drugs must enter cells to undergo metabolism and excretion
- Many drugs produce their effects by binding with receptors on the external surface of the cell membrane
- These do not need to cross the cell membrane to act
Drug Metabolism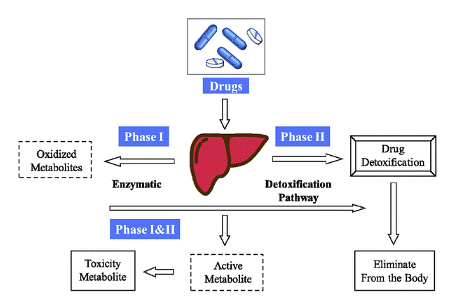
- Also known as biotransformation
- Defined as the enzymatic alteration of drug structure
- Most often takes place in the liver
- Hepatic drug-metabolizing enzymes
- Therapeutic consequences of drug metabolism
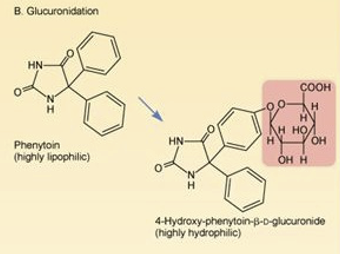
Therapeutic Consequences of Drug Metabolism
- Accelerated renal drug excretion – makes lipid soluble drugs more hydrophilic
- Drug inactivation – converts active compounds to inactive forms
- Increased therapeutic action
- Activation of prodrugs
- inactive when administered, active once metabolized (i.e. Levodopa dopamine)
- Increased or decreased toxicity
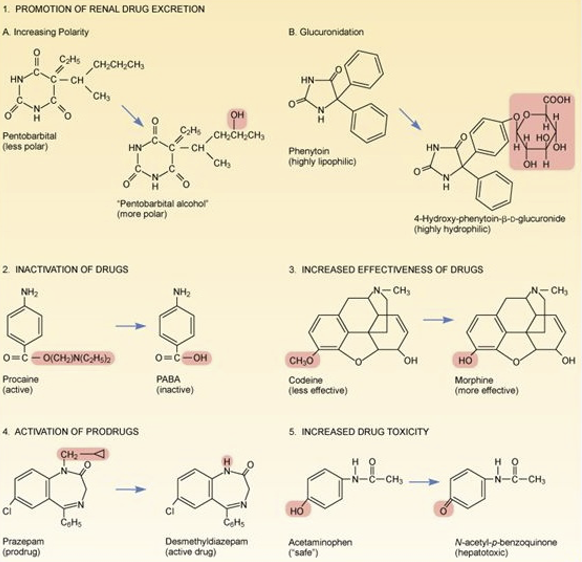
Hepatic Drug-Metabolizing Enzymes
- Most drug metabolism that takes place in the liver
- Performed by the hepatic microsomal enzyme system (P450 system)
- Cytochrome p450 (CYP)- a heme-containing protein that transfers electrons to change the make-up of a molecule
- Three of CYP proteins metabolize drugs
- The rest meatbolize endogenous substances
- Metabolism does not always result in a smaller molecule
- Can synthesize a larger compound
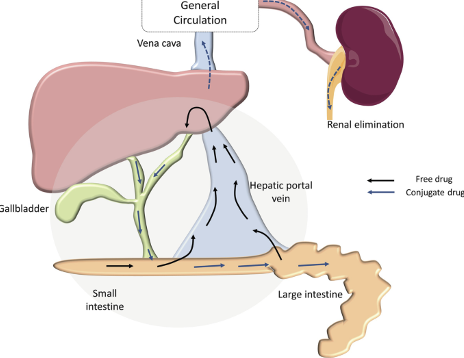
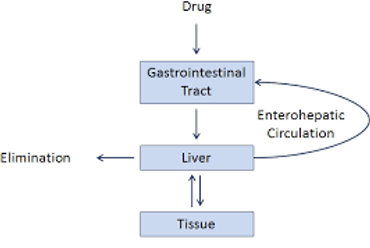
Enterohepatic Recirculation
- Repeating cycle in which drug is transported:
- From the liver into the duodenum (via the bile duct)
- Released back into intestine
- Hydrolyzed and releases free drug
- Back to the liver via the portal blood
- Limited to drugs that have undergone glucuronidation
- Can lead to drugs/effects lasting longer
- LIVER= HEPATIC
Special Considerations in Drug Metabolism
- Age -Renal function declines with age, dignozed with more health problems with age = more medication and more competiton
- Induction of drug-metabolizing enzymes
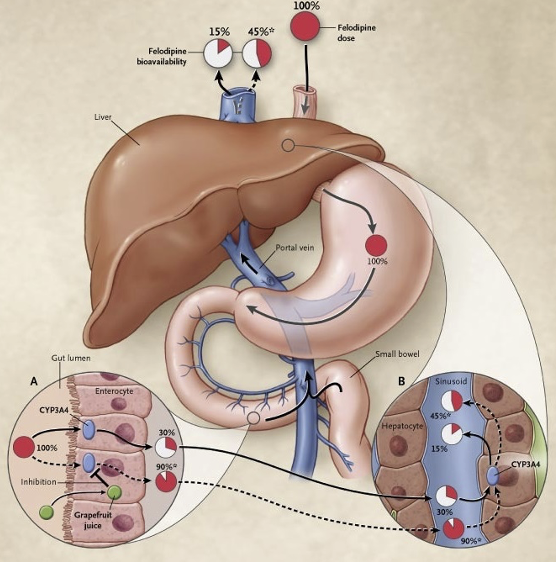
- First-pass effect
- Nutritonal status - certain meds need to be given with food, if someone is underweight?, anticoagulants, empty stomach
- Competition among drugs
Excretion
- The removal of drugs from the body
- Drugs and their metabolites can exit the body through urine, sweat, saliva, breast milk, or expired air
- Most excreted in urine
- Kidneys account for excretion of most drugs
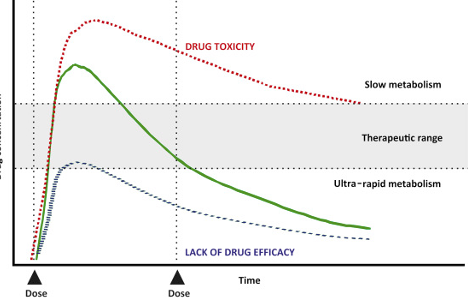
Time Course of Drug Reponses
- Plasma drug levels
- Clinical significance of plasma drug levels
- Two plasma drug levels defined
- Minimum effective concentration
- Toxic concentration
- Therapeutic range
- Single-dose time course
- The duration of effects is determined largely by the combination of metabolism and excretion
- For drug levels above the minimum effective dose, the therapeutic response will be maintained
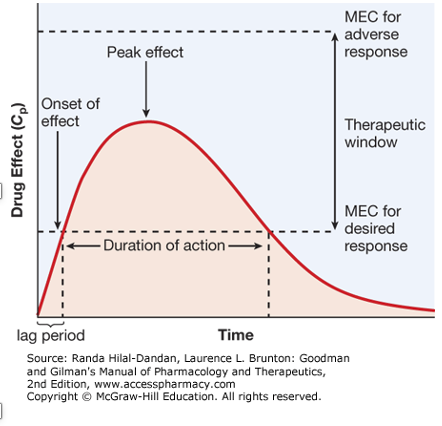
- Drug half-life
- Defined as the time required for the amount of drug in the body to decrease by 50%
- Percentage versus amount
- Determines the dosing interval
- Drug levels produced with repeated doses
- Process by which plateau drug levels are achieved
- Time to plateau
- Techniques for reducing fluctuations in drug levels
- Loading doses versus maintenance doses
- Decline from plateau
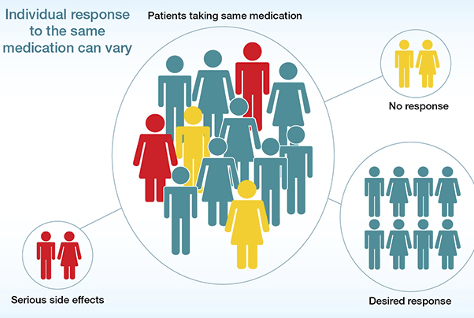
Individual Variation in Drug Responses
- Key factors that cause one patient to respond to drugs differently than another patient
- Important for nurses to know these factors to be better prepared to reduce individual variation in drug responses
- Body weight and composition
- Body surface area versus weight
- Age
- Pathophysiology
- Kidney disease
- Liver disease
- Acid-base imbalance
- Altered electrolyte status
- Tolerance
- Decreased responsiveness to a drug as a result of repeated drug administration
- Higher doses required
- Three types of drug tolerance
- Pharmacodynamic tolerance
- Metabolic tolerance
- Tachyphylaxis
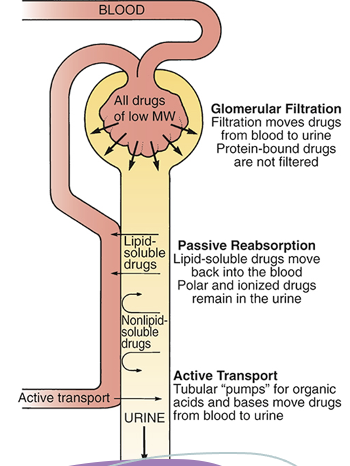
Renal Excretion
Steps in Renal Drug Excretion
- Glomerular filtration
- Passive tubular reabsorption
- Active tubular secretion
Factors that modify renal drug excretion
- pH-dependent ionization
- Competition for active tubular transport
- Age
Nonrenal Excretion
- Breast milk
- Other nonrenal routes of excretion
- Bile
- Enterohepatic recirculation
- Lungs (esepcially anesthesia)
- sweat/saliva (small amounts)
Body Weight & Age
- Body weight and composition
- Body surface area versus weight
- Age
- Significant variability with age in infants and older adults
- Infants: Organ immaturity
- Older patients: Organ degeneration
- Increased severity of illness, multiple pathologies, treatment with multiple drugs
- Significant variability with age in infants and older adults
Pediatric Patients
- All patients younger than 16
- Respond differently to medications than rest of population
- More sensitive to drugs than other patients are
- Show greater individual variation
- Sensitivity due mainly to organ system immaturity
- Increased risk for adverse drug reactions
- Two-thirds of drugs used in pediatrics have never been tested in pediatric patients
- Ongoing growth and development
- Different age groups have different challenges
- Two-thirds of drugs used in pediatrics have never been tested in pediatric patients
- Two laws:
- Best Pharmaceuticals for Children Act (2002)
- Pediatric Research Equity Act of 2003
- These laws were permanently reauthorized as part of the FDA Safety and Innovation Act (FDASIA) of 2012
Pharmacokinetics: Neonates and Infants
- Very young patients more sensitive to drugs
- Effects can be greater and more prolonged due to immaturity of protein binding and metabolism
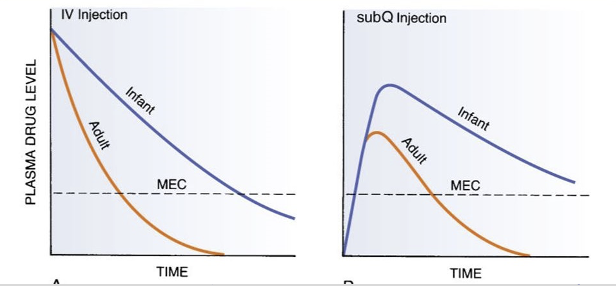
- Effects can be greater and more prolonged due to immaturity of protein binding and metabolism
- Absorption
- Oral administration
- Intramuscular administration
- Percutaneous absorption
- Distribution
- Protein binding
- Blood-brain barrier
- Hepatic metabolism
- The drug-metabolizing capacity of newborns is low
- Renal excretion
- Low renal blood flow, glomerular filtration, and active tubular secretion
Pharmacokinetiocs: Children Aged 1 year and Older
- Most pharmacokinetic parameters are like those of adults
- Drug sensitivity more like that of adults than for children younger than 1 year old
- One important difference:
- Children in this age group metabolize drugs faster than adults
- Markedly faster until the age of 2 years, then a gradual decline
- May need to increase dosage or decrease interval between doses
- Sharp decline at puberty
- Children in this age group metabolize drugs faster than adults
Adverse Drug Reactions
- Children are vulnerable to unique adverse effects related to organ immaturity and ongoing growth and development
- Age-related effects:
- Growth suppression (caused by glucocorticoids)
- Discoloration of developing teeth (tetracyclines)
- Kernicterus (sulfonamides)
- Age-related effects:
- Pediatric patients are subject to adverse reactions when drug levels rise too high.
- Pediatric patients are vulnerable to unique adverse effects related to organ system immaturity and to ongoing growth and development.
Dosage Determination
- Dosing is most commonly based on body surface area
- Initial pediatric dosing is, at best, an approximation
- Subsequent doses need to be adjusted
- Approximate dosage for a child =
"Body surface area of the child × Adult dose " /"1.73 m²" - Most drugs used in pediatric patients have never been tested in children
- As a result, reliable information is lacking on which to base drug selection or dosgae
- Inital pediatric doses are at best approxination; therefore, subsequent doses must be adjusted based on the clinical outcome and plasma drug levels
Promoting Adherence
- Provide patient education in writing
- Demonstration techniques should be included as appropriate
- Effective education should include the following:
- Dosage size and timing
- Route and technique of administration
- Duration of treatment
- Drug storage
- The nature and time course of desired responses
- The nature and time course of adverse responses
Older Adult Patients
- Disproportionately high prescription drug use exists in the older adult population
- Older adult patients are generally more sensitive to drugs than are younger adults, and they show wider individual variation
- Individualization of therapy for older adult patients is essential
- Altered pharmacokinetics
- More sensitive to drugs than younger adults and with greater variation in pharmacokinetics
- Multiple and severe illnesses
- Severity of illness, multiple pathologies
- Multiple-drug therapy
- Excessive prescribing
- Poor adherence
- Individualization of treatment is essential
- Each patient must be monitored for desired and adverse responses
- Regimen must be adhered to
- Goals of treatment:
- Reduce symptoms and improve quality of life
Pharmacokinetics
- The rate of absorption may slow with age
- Increased percentage of body fat
- Decreased percentage of lean body mass
- Decreased total body water
- Reduced concentration of serum albumin
- Hepatic metabolism declines with age
- Reduced renal function, with resultant drug accumulation, is the most important cause of adverse drug reactions in older adults.
Pharmacokinetics: Absoprtion
- Altered gastrointestinal absorption is not a major factor in drug sensitivity
- The percentage of an oral dose that is absorbed does not change with age
- The rate of absorption may slow with age
- Delayed gastric emptying and reduced splanchnic blood flow also occur
Pharmacokinetics: Distribution
- Increased percentage of body fat
- Storage depot for lipid-soluble drugs
- Decreased percentage of lean body mass
- Decreased total body water
- Distributed in smaller volume; concentration increased and effects more intense
- Reduced concentration of serum albumin
- May be significantly reduced in malnourished patients
- Causes decreased protein binding of drugs and increased levels of free drugs
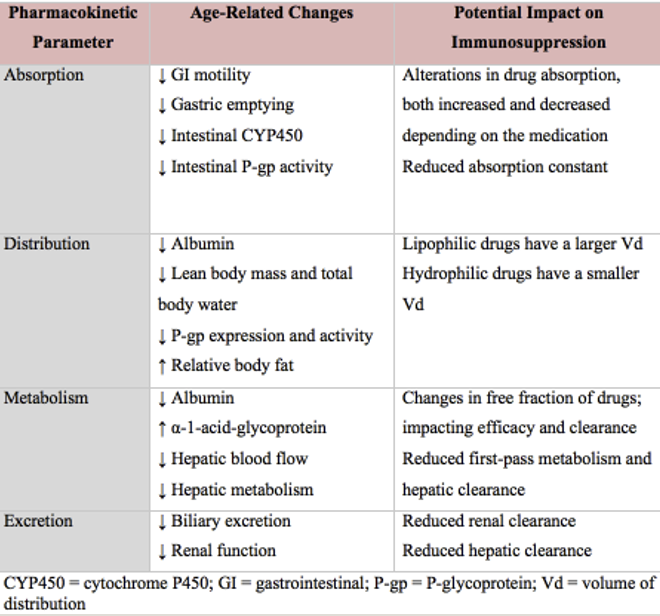
Pharmacokinetics: Metabolism
- Hepatic metabolism declines with age
- Reduced hepatic blood flow, reduced liver mass, and decreased activity of some hepatic enzymes occur
- The half-lives of some drugs may increase, and responses are prolonged
- Responses to oral drugs (eg, those that undergo extensive first-pass effect) may be enhanced
Pharmacokinetics: Excretion
- Renal function undergoes progressive decline beginning in early adulthood
- Reductions in renal blood flow, glomerular filtration rate, active tubular secretion, and number of nephrons
- Drug accumulation as a result of reduced renal excretion is the most important cause of adverse drug reactions in older adults
- Renal function should be assessed with drugs that are eliminated primarily by the kidneys
- In patients who are older adults:
- Use creatinine clearance rather than serum creatinine to assess this, because lean muscle mass (source of creatinine) declines in parallel with kidney function
- Creatinine levels may be normal even though kidney function is greatly reduced
Pharmacodynamic Changes in Older Adult Patients
- Alterations in receptor properties may underlie altered sensitivity to some drugs
- Drugs with more intense effects in older adults
- Warfarin and certain central nervous system depressants
- Drugs with more intense effects in older adults
- Beta blockers less effective in older adults, even in the same concentrations
- Reduction in number of beta receptors
- Reduction in the affinity of beta receptors for beta-receptor blocking agents
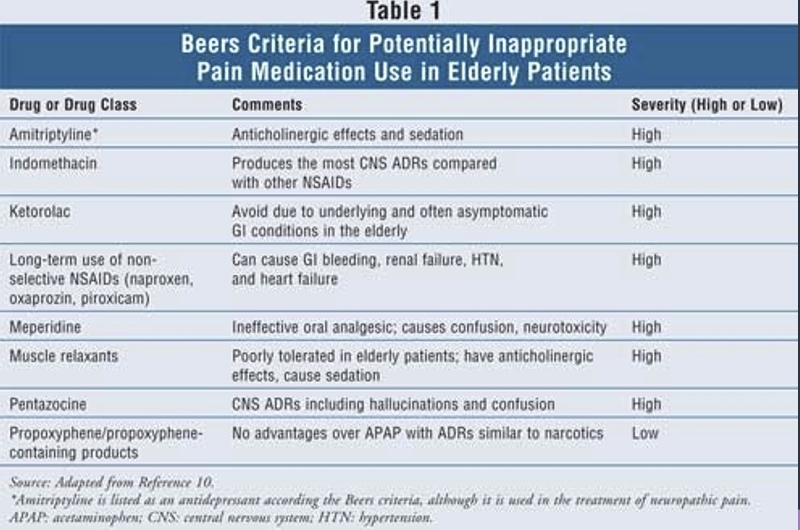
Adverse Drug Reactions in Older Adults (ADRS)
- 7 times more likely in older adults
- Drug accumulation secondary to reduced renal function
- Polypharmacy
- Greater severity of illness
- Multiple pathologies
- Greater use of drugs that have a low therapeutic index (eg, digoxin)
- Inadequate supervision of long-term therapy
- Poor patient adherence
Pathophysiology with Drug Reponses
- Kidney disease
- Reduced excretion and increased toxicity
- Liver disease
- Reduced metabolism and increased toxicity
- Acid-base imbalance
- pH changes that alter absorption, distribution, metabolism, and excretion of drugs
- Altered electrolyte status
Drug Tolerance
- Tolerance: Decreased responsiveness to a drug as a result of repeated drug administration
- Higher doses required
- Three types of drug tolerance
- Pharmacodynamic tolerance
- Metabolic tolerance
- Tachyphylaxis
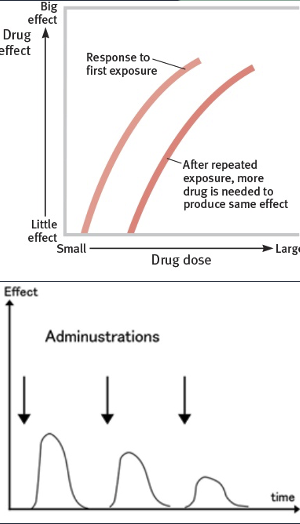
Three Types of Drug Tolerance
- Pharmacodynamic tolerance
- Long-term administration of drugs such as morphine and heroin
- Metabolic tolerance
- Results from accelerated drug metabolism
- Tachyphylaxis
- Reduction in drug responsiveness brought on by repeated dosing over a short time
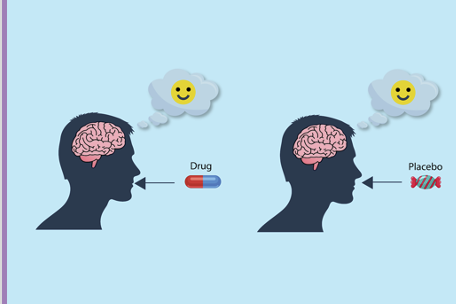
Placebo Effect
- Any response that a patient has to a placebo is based solely on his or her psychologic reaction to the idea of taking a medication and not to any direct physiologic or biochemical action of the placebo itself
- Nurses need to present a positive but realistic assessment of the effects of therapy
- Placebos are primarily used for the control groups in clinical trials
- Nocebo effect
Variability in Absoprtion
- Bioavailability
- Ability of the drug to reach the systemic circulation from its site of administration
- Occurs primarily with oral preparations rather than with parenteral administration
- Tablet disintegration time, enteric coatings, and sustained-release formulations affect this
- Other causes of variable absorption
- Changes in gastric pH, diarrhea, constipation, and food in the stomach
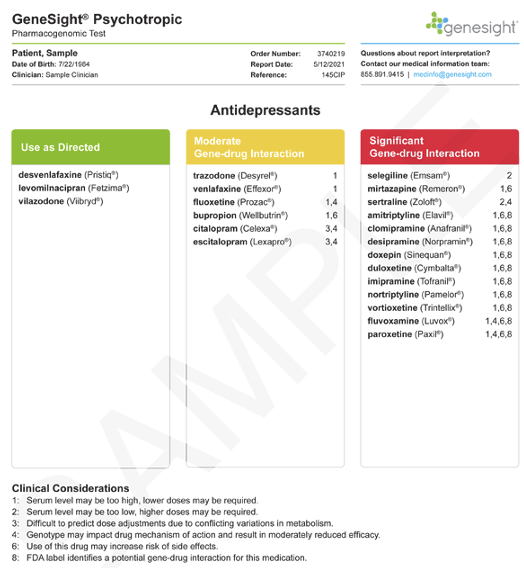
Genetics and Pharmacogenomics
- Pharmacogenomics: Study of how genes affect individual drug responses
- Altered drug metabolism
- May accelerate or delay the metabolism
- Warfarin, succinylcholine, isoniazid, cytochrome P450
Variations
- Altered drug targets
- Genetic variations alter the structure of drug receptors
- Other ways genetics can influence drug responses
- Some genetically determined drug responses are based on factors other than changes in drug metabolism or drug targets
- Gender
- Alcohol is metabolized more slowly by women than by men
- Certain opioid analgesics are much more effective in women than in men
- Quinidine causes greater QT interval prolongation in women than in men
- Race
- Genetic variations
- Psychosocial factors Comorbidities
- Increased likelihood of drug interactions
- Diet
- Starvation can reduce protein binding of drugs
- Monoamine oxidase inhibitors: Malignant hypertension triggered by foods that contain tyramine
- Genetic variations
- Psychosocial factors Failure to take medicine as prescribed
- Issues include manual dexterity, visual acuity, intellectual capacity, psychologic state, attitude toward drugs, and ability to pay for medication
- Drug interactions
- One drug alters the effects of another
Gender & Race Variations
- Gender
- Alcohol is metabolized more slowly by women than by men
- Certain opioid analgesics are much more effective in women than in men
- Quinidine (antiarrhythmic agent) causes greater QT interval prolongation in women than in men
- Race
- Genetic variability
Other Variations
- Comorbidities
- Increased likelihood of drug interactions
- Drug interactions
- One drug alters the effects of another
- Diet
- Starvation can reduce protein binding of drugs
- Monoamine oxidase inhibitors: Malignant hypertension triggered by foods that contain tyramine
Failure to Take Medicine as Prescribed
- Issues include manual dexterity, visual acuity, intellectual capacity, psychologic state, attitude toward drugs, and ability to pay for medication
- Promote adherence:
- Simplified drug regimens
- Clear and concise verbal and written instructions
- Appropriate dosage form
- Clearly labeled and easy-to-open containers
- Daily reminders
- Support system
- Frequent monitoring
Promoting Adherance with Unintentional Nonadherance
- Simplified drug regimens
- Clear and concise verbal and written instructions
- Appropriate dosage form
- Clearly labeled and easy-to-open containers
- Daily reminders
- Support system
- Frequent monitoring
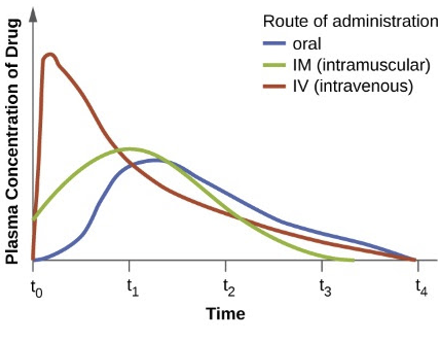
Question 1
A nurse is preparing to administer epinephrine to a patient who is having a severe allergic reaction. Which route of administration should the nurse use to provide the fastest and most complete abiosprtion of epinephrine
- Intravenous
- Intramuscular
- Subcutaneous
- Oral
Rationale: Intravenous administration results in the fastest and most complete absorption of a drug.
Question 2
When preparing to administer a sustained-realease capsule to a patien, the nurse understands that which of the following is ture for sustained-release capuskles?
- They are usually most costly than pills
- They are rapiudly absorbed
- They need to be crushed for appropriate absorption to take place
- They need to be taken at regular intervals throughout the day
Rationale: A capsule may cost more than a pill. Sustained-release formulations are capsules filled with tiny spheres that contain the actual drug; the individual spheres have coatings that dissolve at variable rates. Because some spheres dissolve more slowly than others, drug is released steadily throughout the day. These capsules should not be crushed. The primary advantage of sustained-release preparations is that they permit a reduction in the number of daily doses. These formulations have the additional advantage of producing relatively steady drug levels over an extended time (much like giving a drug by infusion). The major disadvantages of sustained-release formulations are their high cost and their potential for variable absorption.
Question 3
The nurse identifies which patient as being at highest risk for slow drug metabolism?
- 2-year-old boy who is prescribed an oral antibiotic
- 14-year-old girl who takes four prescription drugs
- 56-year-old man who has chronic hepatic disease
- 76-year-old woman who has an elevated temperature
Rationale: Drug metabolism, which is also known as biotransformation, is the enzymatic alteration of drug structure. Most drug metabolism takes place in the liver.
Question 4
Dignozin has a half-life of 36 to 48 hours. Because of the length of the hald-life, the nurse expects dosing to occur how often?
A.4 times per day
B.3 times per day
C.2 times per day
D.Once a day
Rationale: The concept of the half-life tells us that, no matter what the amount of drug in the body may be, half (50%) will leave during a specified period of time (ie, the half-life). The actual amount of drug that is lost during one half-life depends on just how much drug is present: The more drug that is in the body, the larger the amount lost during one half-life. If a long dosing interval were used, drug levels would fall below the minimum effective concentration between doses, and therapeutic effects would be lost. Conversely, if a drug has a long half-life, a long time can separate doses without a loss of benefits.
Question 5
A patient with cancer is receiving morphine for pain control. The patient calls the nurse to report that the morphine is no longer controlling his pain. What is the most appropriate response by the nurse?
- “Increasing the dose of morphine will make you so sleepy that you will not be able to function.”
- “This means that you have developed a psychologic addiction to morphine.”
- “You have developed a tolerance to morphine and will need a higher dose.”
- “It is recommended that we wait to increase the morphine until the pain is more severe.”
Rationale: Tolerance is a decreased responsiveness to a drug as a result of repeated drug administration. Patients who become tolerant to a drug require higher doses to produce effects equivalent to those that could be achieved with lower doses before the tolerance developed.
Question 6
The nurse is preparing to administer warfarin [Coumadin] to a patient. The nurse notes that the patient has altered CYP2D6 genes. It is most important for the nurse to do which of the following?
- Check for signs of a transient ischemic attack.
- Monitor for ST-segment elevation or depression.
- Observe the patient’s legs for symptoms of a blood clot.
- Examine the patient’s stools for the presence of blood
Rationale: Variants in the gene that codes for CYP2C9 can increase the risk of toxicity (ie, bleeding) when taking warfarin [Coumadin], an anticoagulant with a narrow therapeutic index. The nurse should assess the patient for the presence of bleeding.
Question 7
A patient was discharged from the hospital with instructions to take an antibiotic for 7 days to treat a bladder infection. Twelve days later, a home care nurse visits the patient and finds that the symptoms have not resolved. What is the most important question for the nurse to ask?
A.“Do you think you have another bladder infection?”
B.“Have you taken all of the antibiotics as directed?”
C.“How much water have you been drinking each day?”
D.“What antibiotic do you usually take to treat an infection?”
Rationale: The failure to take medications as directed is a common cause of persistent infection.
Question 8
The nurse provides teaching for the caregiver of a 2-month-old infant and a 3-year-old child. Both children will be taking oral ampicillin (an acid-labile drug) to treat a bacterial infection. The nurse determines that teaching is successful if the caregiver makes which of the following statements?
- “The dose will not be different, but the baby will take the drug for 7 days instead of 10 days.”
- “The dose will be higher for the baby, because the infection is more serious.”
- “The dose will be the same, because my children have the same infection.”
- “The dose will be smaller for the baby, because the drug will be absorbed better in the stomach.”
Rationale: Children between the ages of 1 and 12 years metabolize drugs faster than adults. They may need an increase in dosage or a reduction in dosing interval for drugs that are eliminated by hepatic metabolism.
Question 9
A 2-year-old child is prescribed an oral drug that is eliminated by metabolism in the liver. Based on the child’s age, the nurse would expect to make which adjustment?
- The drug may need to be administered more frequently.
- The dosage of the drug may need to be decreased.
- The route should be changed from oral to intramuscular.
- The drug should be administered on an empty stomach.
Rationale: Children between the ages of 1 and 12 years metabolize drugs faster than adults. They may need an increase in dosage or a reduction in dosing interval for drugs that are eliminated by hepatic metabolism.
Question 10
A 15-month-old patient develops chemotherapy-induced nausea and vomiting. Which medication, if ordered by the healthcare provider, should the nurse question?
- Ondansetron [Zofran]
- Dexamethasone [Decadron]
- Promethazine [Phenergan]
- Metoclopramide [Reglan]
Rationale: Certain drugs can cause unique adverse effects in pediatric patients of various ages. These drugs should be avoided in patients whose age puts them at risk. Promethazine is contraindicated in children younger than 2 years old because pronounced respiratory depression may occur.
Question 11
A toddler has been prescribed a medication that does not have an established pediatric dose. To calculate the appropriate dose for the child, the nurse should consider what information?
- The child’s weight is 26 pounds.
- The child’s height is 32 inches.
- The child’s body surface area is 0.52 kg/m2.
- The child’s age is 24 months.
Rationale: For drugs without an established pediatric dose, the dose is based on the child’s body surface area. The most commonly used formula is as follows: Approximate child’s dose = (Body surface area of the child × Adult dose)/1.73 m2.
Question 12
The nurse is assessing an 82-year-old patient before the administration of medications. Which laboratory result would provide the best index of renal this patient’s function?
- Serum creatinine
- Blood urea nitrogen
- Urinalysis
- Creatinine clearance
Rationale: In older adults, the proper index of renal function is creatinine clearance. Serum creatinine levels do not reflect kidney function in older adults, because the source of serum creatinine—lean muscle mass—declines in parallel with the decline in kidney function. As a result, creatinine levels may be normal even though renal function is greatly reduced.
Question 13
An older adult patient is taking a new prescription medication. After reviewing the patient’s medical record, the nurse is most concerned about an adverse drug reaction if what is documented?
- The patient is currently taking eight prescription medications.
- The patient’s urinary creatinine clearance is 70 mL/min/1.73 m2.
- The patient regularly takes herbal and dietary supplements.
- The patient takes a medication with a high therapeutic index.
Rationale: Drug accumulation secondary to reduced renal function in older adults is the most important factor in adverse drug reactions. The best indicator of renal function is urinary creatinine clearance. Urinary creatinine clearance of less than 105 to 110 mL/min/1.73 m2 indicates reduced renal function.
Question 14
The nurse instructs an 82-year-old patient about over-the-counter medications that are generally safe for older adults. The nurse should intervene if the patient makes which of the following statements?
- “I can take chlorpheniramine [Chlor-Trimeton] for a cold.”
- “If I have a headache, I should take acetaminophen [Tylenol].”
- “Cetirizine [Zyrtec] would be safe to take for my allergies.”
- “I should avoid taking diphenhydramine [Benadryl] for hives.”
Rationale: The Beers list identifies drugs with a high likelihood of causing adverse effects in older adults. Drugs on this list should generally be avoided. Chlorpheniramine is on the Beers list, and it has anticholinergic effects (eg, constipation, urinary retention, blurred vision). The Beers list is available online at http://archinte.ama-assn.org/cgi/reprint/163/22/2716.
Question 15
An older adult patient frequently forgets to take an oral medication that has been prescribed to be taken 3 times a day. Which action by the nurse is best?
- Assess the patient’s ability to swallow the medication.
- Arrange for a neighbor to call the patient 3 times a day.
- Call the prescriber for a sustained-release form of the drug.
- Give the patient verbal and written instructions about the drug.
Rationale: If the patient forgets to take a prescribed medication that is scheduled throughout the day, simplifying the regimen by reducing the number of doses per day may improve adherence. Enlisting the aid of a friend, relative, or visiting healthcare professional 3 times a day may be helpful, but it is not realistic. In addition, the patient should retain as much independence as possible in his or her self-care. Explaining the treatment plan using clear and concise verbal and written instructions will not directly correct the problem of forgetfulness. Difficulty swallowing may be a reason for nonadherence, but it is not related to the problem of forgetfulness.