COMPETENCY APPRAISAL (PEDIA; 10/07/2023)
GROWTH AND DEVELOPMENT |
|---|
Growth | Increase in the physical size of an individual; a quantitative change. |
|---|
Parameters: weight and height |
|---|
Weight: The most sensitive measure of growth. Weight milestones: - 6 months: double
- 12 months: triple
- 24 months: quadruple
|
|---|
Height: Increases by 1" per month during the first 6 months
Average increase in height in 1 year = 50%. Height stops with the eruption of wisdom teeth. |
|---|
Development | Increase in skills or capability to function; a qualitative change; maturation or "readiness." |
|---|
Parameter: task completion
Indicators: - Fine motor
- Gross motor
- Language
- Social skills
|
|---|
Cognitive development: Ability to learn & understand from experience, acquire and retain knowledge, respond to new situations, and solve problems. |
|---|
Principles of Growth & Development | - G&D are continuous processes, beginning from conception until death
- Different children pass through stages at different rates (individual variation at regular direction).
- G & D proceed in an orderly sequence (e.g., sitting before creeping, standing before walking).
- All body systems do not develop at the same rate (asynchronous development).
|
|---|
RATES OF GROWTH AND DEVELOPMENT |
|---|
Fetal & infancy | Most rapid G & D; at risk for anemia. |
|---|
Toddler | Physiologic anemia due to being picky eaters. |
|---|
Toddler and preschool | Alternating rapid & slow growth. |
|---|
School age | Alower growth; least prone to anemia. |
|---|
Adolescence | Rapid growth due to puberty. |
|---|
FACTORS OF GROWTH |
|---|
Hereditary | Race, intelligence, nationality, sex (growth spurt M: 13 yrs; F: 11 yrs) |
|---|
Environment | Health, parent-child relationship, socioeconomic status, quality of nutrition |
|---|
DIRECTIONAL TRENDS IN DEVELOPMENT |
|---|
Cephalocaudal (Head to Tail) | Development progresses from the head towards the feet. - Infant can lift the head in the prone position in the first 2 months.
- Infant can lift the head and chest in the 3rd month.
- Infant can lift the head, chest, and abdomen by the 4th month.
- Infant can stand by 9-10 months.
|
|---|
Proximodistal | Development proceeds from the central part (proximal) of the body outward towards the extremities (distal). |
|---|
Symmetrical on Each Side | Development occurs uniformly on both sides of the body. |
|---|
Mass-Specific (Differentiation) | Progression from simple to complex tasks, differentiating abilities. |
|---|
Gross to Refined | Development process starts with gross movements and refines into more precise actions. |
|---|
Sequential | Development follows a sequential order or a specific sequence of milestones. |
|---|
Locomotion | Developmental stages may include the acquisition of locomotion skills (e.g., crawling, walking). |
|---|
Social | Social development is an integral part of overall development. |
|---|
Neonatal Reflexes | Neonatal reflexes must be lost or integrated before a child can progress to more advanced stages. - Plantar reflex should disappear before walking.
- Moro reflex should disappear before rolling.
- Persistent neonatal reflexes may indicate a neurological problem.
|
|---|
CONCEPTS OF DEVELOPMENT |
|---|
Behavior | Most comprehensive indicator. |
|---|
Play | Universal language. |
|---|
Practice | Learning skills and behavior. |
|---|
Time | Great factor for learning a skill. |
|---|
Reflexes | Neonatal reflexes must disappear before development starts. - Moro reflex should disappear before standing.
- Persistent neonatal reflexes may indicate a neuro problem or developmental delay.
|
|---|
DIVISION OF LIFE |
|---|
Prenatal: 20 weeks AOG to 28 days of life | Preschool: 4-6 years |
|---|
Neonate: First 28 days after birth | School Age: 7-12 years |
|---|
Infancy: 29th day to 1 year | Adolescence: 12-18 years |
|---|
Toddler: 1-3 years | |
|---|
DEVELOPMENTAL THEORIES |
|---|
Theories | Infant | Toddler | Pre-school | School Age | Adolescent |
|---|
Psychosocial (Erikson) | Trust vs. Mistrust | Autonomy vs. Shame and Doubt | Initiative vs. Guilt | Industry vs. Inferiority | Identity vs. Role Confusion |
|---|
Psychosexual (Freud) | Oral | Anal | Phallic | Latency | Genital |
|---|
Cognitive (Piaget) | Sensorimotor | Preoperational | Concrete Operational | Formal Operational |
|---|
Moral (Kohlberg) | Amoral | Pre-conventional | Conventional | Post-conventional |
|---|
Punish/Obedience orientation | Naive instrumentation orientation | Law and order |
|---|
Significant Person | Primary caregiver | Parents | Family | Teacher Peers | Peer Group Opposite Sex |
|---|
Fears | | | | | |
|---|
SIGNS OF SEXUAL MATURITY |
|---|
GIRLS | BOYS |
|---|
- Thelarche (enargement of boobs and genitals)
- Widening of hips
- Appearance of axillary and pubic hair
- Accelerated linear growth
- Growth spurt (age 9-11)
- Menarche (last sign of sexual maturity)
| - Testicular (testes and penis) enlargement
- Deeping of voice
- Development of muscles
- Appearance of axillary and pubic hair
- Growth spurt (age 12-14)
- Production of viable sperm (last sign of sexual maturity)
|
|---|
DEVELOPMENTAL MILESTONES
INFANCY |
|---|
Play | - Solitary plays (non-interactive).
- Prioritize safety: Toys must be size-appropriate, non-toxic, and non-detachable.
- Best toy: Rattle. Universal toy: Ball. Color: Red.
- Musical mobiles: Introduce at 2 to 4 months, placed 8 inches away.
|
|---|
Fear | - Stranger anxiety begins at 6 months, peaks at 8 months, and diminishes at 9-12 months.
|
|---|
Diet | - Starts at 4 to 6 months.
- Introduce foods one at a time to identify allergies.
|
|---|
Accidents | - Foreign body aspiration is a concern.
- Males are more prone to Sudden Infant Death Syndrome (SIDS).
|
|---|
Body Weight | - 6 months: Doubles.
- 12 months: Triples.
- 24 months: Quadruples.
|
|---|
TODDLER |
|---|
Play | - Parallel play: Two toddlers playing side by side but separately w/o sharing toys.
- Best toy: Wagon (push and pull)
|
|---|
Fear | - Separation anxiety begins at 9 months, and peaks at 18 months.
- 3 Phases Of Separation Anxiety: Protect, Despair, and Denial
- Don't prolong goodbyes.
- Say goodbye firmly to develop trust and mention when you will be back (meal times like lunch bc they dont have concept of time).
- Avoid yes or no questions.
|
|---|
Accidents | - Drowinging, burns, and poisoning.
|
|---|
Behavior | - Egotistic, RItualistic, Negativistic, and Temper tantrums.
|
|---|
Cues for toilet training | - Wake up or stays dry for 2 hours
- Able to sit, squat, and walk
- Able to communicate needs
- Able to sit on the toilet for 5-10 minutes
|
|---|
PRE-SCHOOLER |
|---|
Play | - Associative play: Makes believe toys are alive, imaginary friend, and dresses up.
|
|---|
Fear | - Mutilation or castration (bodily harm), ghost, monster, and dark places.
|
|---|
Accidents | - Drowinging, burns, and poisoning.
|
|---|
Behavior | - Curious, imaginative, and imitative.
|
|---|
Behavior problems | - Telling tall tales: due to overactive imagination.
- Imaginary friend: way to release tension and anxieties.
- Sibling rivalry: from jealousy towards a newly delivered baby.
- Regression: revert to earlier stages of development (thumb sucking).
|
|---|
SCHOOL AGE |
|---|
Play | - Indoor competitive play: Like tug of war, track and field, and basketball.
|
|---|
Fear | - Failure in school
- Fear of Death
- School Phobia
- Displacement from School
- Loss of Privacy
|
|---|
Accidents | - Poisoning and greenstick fracture
|
|---|
Behavior | - Industrious and modest.
- Often love collecting items, such as stamps.
|
|---|
ADOLESCENT |
|---|
Play | - Outdoor competitive play: Like intrams and basketball.
|
|---|
Fear | - Rejection
- Body image (obesity and acne)
|
|---|
Accidents | - Motor vehicle accidents, smoking, drug addiction, and pre-marital sex.
|
|---|
Behavior | - Idealistic, Adventurous, Rebellious, and strives for independence.
|
|---|
INFANCY |
|---|
Neonate | Complete head lag |
|---|
1 Month | Look at mobile but at midline, only |
|---|
2 Months | Holds head up when prone. Social smile, baby coos "doing sound", cries with tears |
|---|
3 Months | Holds head and chest up when prone Follows object past the midline. |
|---|
4 Months | Turns front to back Makes bubbling sounds, laughs aloud |
|---|
5 Months | Can roll over Turns both ways due to developed abdominal muscles |
|---|
6 Months | Sits with support Says vowel sounds "ah" and "oh" |
|---|
7 Months | Transfers objects from hand to hand |
|---|
8 Months | Sits without support Plantar reflex disappears for walking preparation |
|---|
9 Months | Creeps or crawls Can stand with support |
|---|
10 Months | Pulls self to stand |
|---|
11 Months | Cruises |
|---|
12 Months | Can stand alone momentarily Walks with assistance |
|---|
TODDLER |
|---|
15 months | Walks alone. Lateness in walking may indicate mild mental retardation. |
|---|
18 months | Bowel control achieved (bowel before bladder). Can run and jump in place. |
|---|
24 months | Daytime bladder control achieved (before nighttime). "Terrible Two’s" phase. |
|---|
30 months | Begins brushing teeth. (Watch for tonsillitis, GABHS, rheumatic heart disease, Beta-hemolytic staph) Initial dentist visit is recommended when temporary teeth are complete. |
|---|
36 months | Nighttime bladder control achieved. Rides a tricycle. |
|---|
PRE-SCHOOLER |
|---|
4 years old | Can button buttons. Can jump and skip. |
|---|
5 years old | Can copy a triangle. |
|---|
6 years old | Can tie shoes and ride a bicycle. Has permanent teeth. |
|---|
SCHOOL AGE |
|---|
7 years old | Assimilation age Can copy a diamond Basic habits and hygiene Quieting down period |
|---|
8 years old | Expansive age Loves to collect objects |
|---|
9 years old | Coordination improves Hero worship |
|---|
10 years old | Can write legibly Joins organizations or groups Well mannered in front of adults |
|---|
11-13 years old | Secret language is common Sense of humor is present Share secrets with friends |
|---|
IMMEDIATE CARE OF NEWBORN |
|---|
Initiation and Maintenance of Respiration | How to initiate airflow: - Stimulate crying with a back rub or tangential slap.
- Remove secretions with a bulb syringe.
- Catheter suctioning:
- Place the head to the side to facilitate drainage of secretions and prevent aspiration.
- Suction the mouth first before the nose.
- Suctioning should last 5-10 seconds, be gentle and quick.
- Evaluate for patency by covering the nostril; additional suctioning may be needed if the baby struggles.
- Endotracheal tube is inserted and oxygen can be administered by a positive pressure bag and mask with 100% oxygen at 40-60 breaths per minute.
Nursing Alert in O2 Administration: - No smoking to prevent combustion.
- Always humidify to prevent drying of the mucosa.
- Avoid eye exposure to oxygen bc it can lead to scarring of the retina, leading to blindness (Retinopathy of Prematurity, ROP).
- When newborn is meconium stained, do not administer oxygen with pressure bc it can lead to aspiration.
|
|---|
Establishing Extra-Uterine Circulation | Circulation initiated by lung expansion, completed by cutting the cord. - Increased PCO2 stimulates the first breath.
- Lung expansion initiates lung circulation.
- Cutting the cord initiates adult circulation.
- Proper position: Right side-lying position.
3 SHUNTS: Openings to redirect blood flow to major body organs: - Ductus Venosus: Shunts between the umbilical vein and vena cava.
- *Foramen Ovale: Shunts between the left and right atrias of the heart.
- *Ductus Arteriosus: Shunts between the pulmonary artery and aorta.
|
|---|
Control of Body Temperature (Temperature Regulation) | Goal: Maintain temperature not less than 36.5°C (97.7°F) to prevent hypothermia and stress. - Factors leading to hypothermia: Immaturity, preterm or SGA babies, inadequate subcutaneous fat, wetness, and inability to shiver.
Types of heat loss: - Convection: exposed to cool air (aircon)
- Conduction: placed on cold surface (metal weighing scale)
- Radiation: near cool object or wall without contact (viewing window)
- Evaporation: through exposed skin (not clothed properly)
Prevention of Hypothermia: Dry and wrap the baby, use a radiant warmer, prevent unnecessary exposure, kangaroo care. |
|---|
Establish Adequate Nutritional Intake | Physiology of breast milk production: Prolactin (stimulates acinar cells and alveoli to produce milk) and Oxytocin (triggers "milk ejection reflex" or "let-down reflex.") - Advantages of breastfeeding: Economical, bonding, uterine involution, higher IQ, antibodies.
- Disadvantages: Possibility of transmission of infections, lack of iron.
Stages of Breast Milk: - Colostrum: 2-4 days post-delivery
- Transitional milk: 4-14 days
- Mature milk: 14 days and beyond; Rich in linoleic acid, brain development
|
|---|
Establish Waste Elimination | Types of stool: - Meconium (physiologic stool, black, green, sticky, tar-like, odorless; normal).
- Transitional stool (4-14 days after birth, green, loose, shiny, due to breast milk).
- Breastfed stool (golden yellow, soft, mushy, sour milk smell, frequently passed).
- Bottle-fed stool (pale yellow, formed, hard, bad odor, seldom pass/constipated).
- Supplementary stool (4-6 months old with food added, brown, and odorous).
|
|---|
ASSESSMENT FOR WELL-BEING
APGAR SCORE |
|---|
Scoring parameter | Score 0 | Score 1 | Score 2 |
|---|
Appearance | Blue/pale | Acrocyanosis | Pinkish |
|---|
Pulse rate *most important | Absent | <100 (Slow) | >100 (Strong) |
|---|
Grimace | No Response | Grimace or weak cry | Cough or strong Cry |
|---|
Activity | Flaccid extremities | Some flexion | Well flexed |
|---|
Respiration | Absent | Slow, irregular, weak | Good, strong cry |
|---|
0 - 3: Severely depressed, requiring CPR and NICU admission. 4 - 6: Moderately depressed, needing additional interventions like suctioning and oxygen administration. 7 - 10: Indicates good health |
|---|
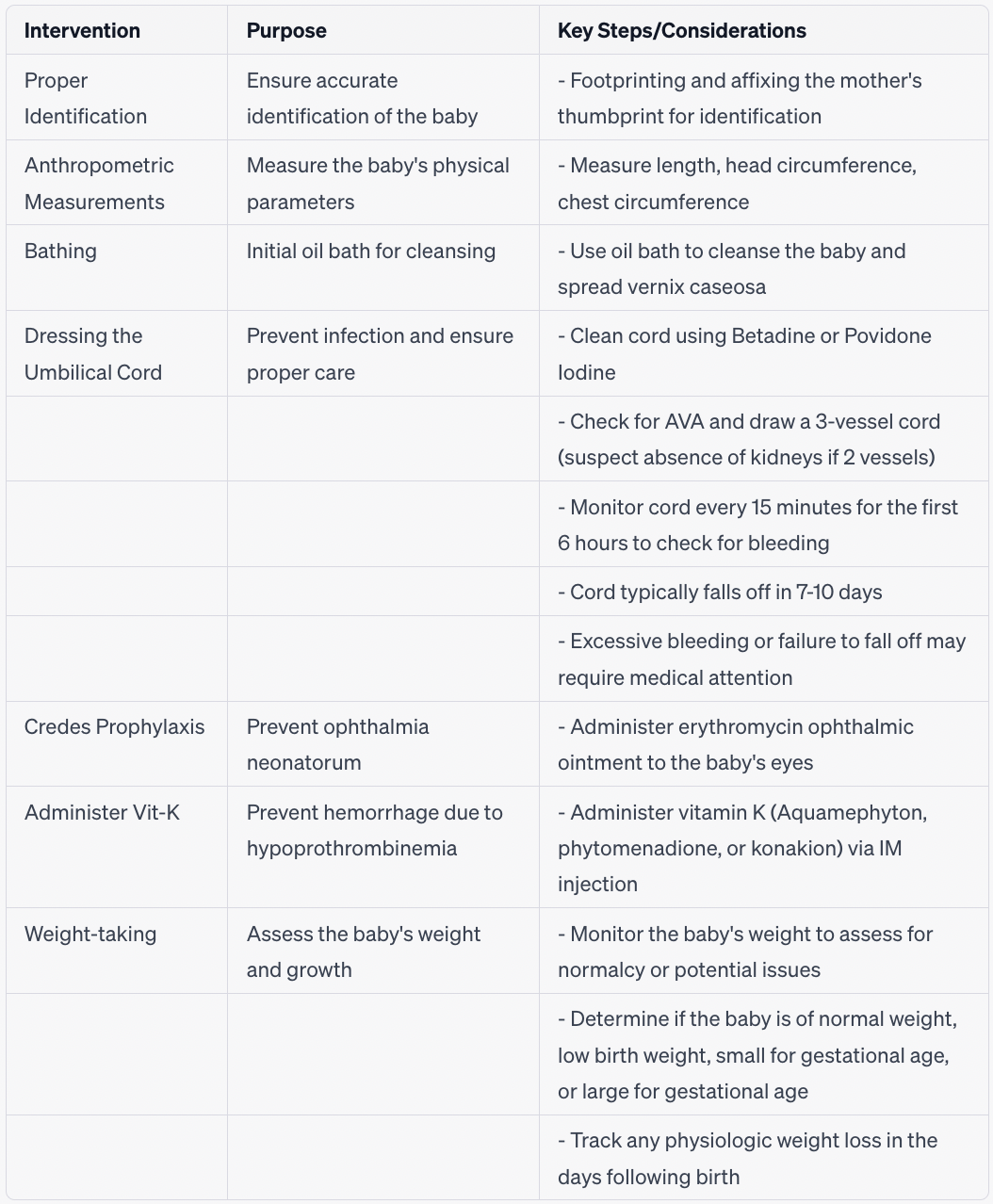
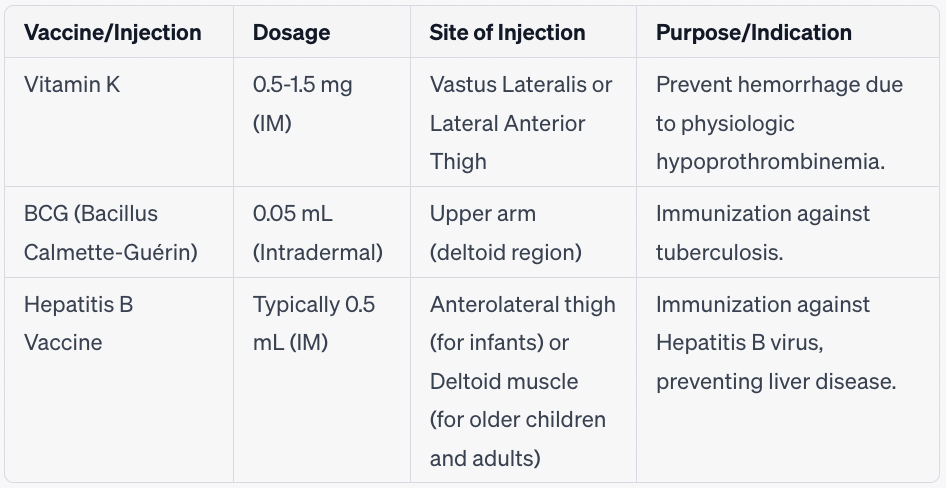
ROUTINE NEWBORN CARE IN THE NURSERY
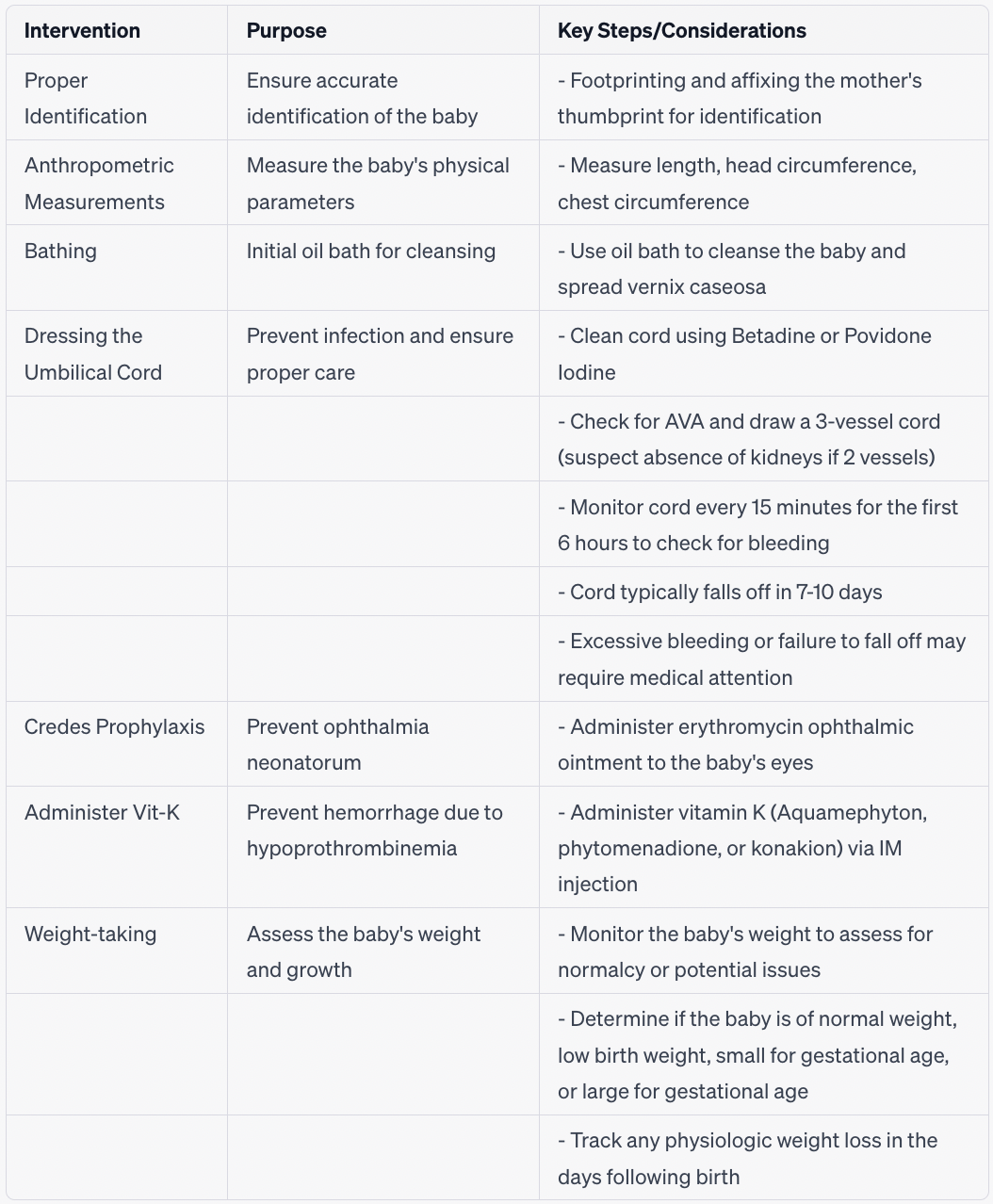
VACCINE AND INJECTIONS
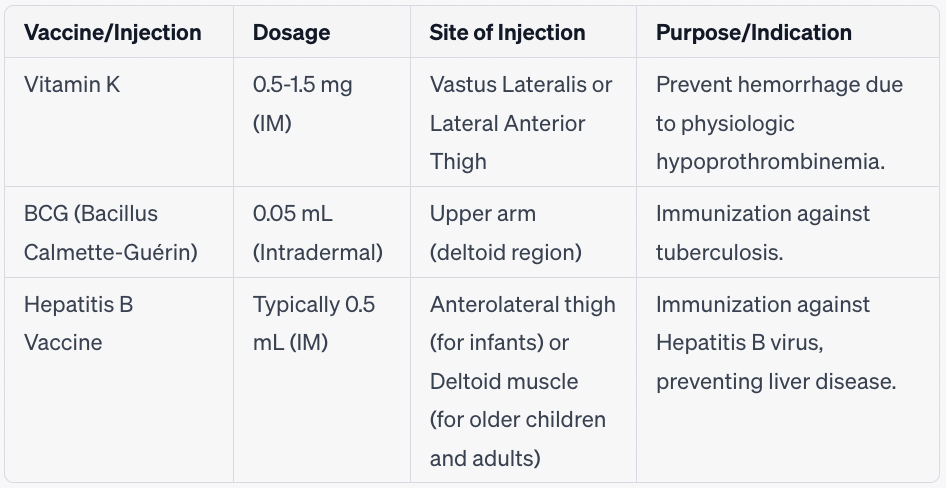
PHYSICAL ASSESSMENT |
|---|
Body Part | Normal | Abnormal |
|---|
Head | - Easy for head to mold
- Anterior fontanel: diamond shape, closes at 12-18 months
- Posterior fontanel: triangle shape, closes at 2-3 months
- Caput succedaneum (edema/fluid): Swelling crossing over the suture line, disappears in 3 days
- Cephalohematoma (blood): Collection of blood causing increased ICP, disappears in 3-6 weeks
| - Abnormal head shape
- Fontanel abnormalities
|
|---|
Eyes | - Administer 0.5% erythromycin or 1% tetracycline to prevent ophthalmia neonatorum
- Strabismus (cross-eyed) is normal until 6 months
| |
|---|
Ears | | - Low set may indicate Down syndrome (trisomy 21)
|
|---|
Nose | - Should be symmetrical with no deformities
- Nostrils should be patent
| - Flaring indicates respiratory distress
|
|---|
Mouth | - Intact palate, lips, and pink gums - Epstein pearls (white)
| - Koplik spots (measles)
- Cleft palate and lip
|
|---|
Chest | - Symmetrical and normal shape - Smaller than the head by 1-2 cm
- Witches milk may be present
| - Chest abnormalities
- Intercostal retraction (indicates respiratory distress)
|
|---|
Abdomen | - Abdominal circumference < head circumference
- Meconium passed within 24 hours
- Umbilical cord with clamp
- Bowel sounds present after 1 hour
| |
|---|
Skin | - Acrocyanosis (pink chest and bluish extremities)
- Physiologic jaundice (peaks at 5th day of life, lasts 10-14 days)
| - Skin abnormalities
- Pathologic jaundice
- Other skin issues
|
|---|
Genital region | - Female: pseudomenstruation (pink discharge) - Male: descended testes - First void within 24 hours
| - Genital abnormalities (cryptorchidism, hypospadias, epispadias, phimosis, hydrocele)
|
|---|
Back | | - Dimpling or sac (indicates spina bifida)
|
|---|
Extremeties | - Symmetrical arms and legs
| - Asymmetrical arms and legs
- Ortolani’s click (indicates congenital hip dysplasia)
|
|---|
PEDIATRIC DISORDERS
CEREBRAL PALSY |
|---|
Description | Neuromuscular disorder with no muscle coordination |
|---|
Causes | - Brain anoxia due to prolonged labor/cord prolapse)
- Infection: cytomegalovirus
- Toxoplasmosis due to mother gardening or touching feces of cats
|
|---|
Types | Spastic, Athetoid, Ataxic |
|---|
Factors | Only recognizable as child begins to learn how to walk and attempt complex motor skills |
|---|
Sign and symptoms | Infant: - Abnormal posturing
- Difficulty feeding
- Persistent primitive reflexes
- Delayed development
According to type: - Spastic: Excessive muscle tone, Scissor gait
- Athetoid: Worm-like, Limp or flaccid
- Ataxic: Awkward wide gait
|
|---|
Diagnostics | Inspection |
|---|
Nursing management | - Health teaching: CP is nonprogressive. It is a disorder that can be cncite during physical therapy.
- Prevent contractures by doing exercise
- Promote mobility and self-help skills
- Promote ambulation
- Encourage play with other children
|
|---|
Medical management | - Baclofen: muscle relaxant that reduces muscle spasticity.
- Use of assistive devices
- Therapy (pt, ot, speech)
|
|---|
HYDROCEPHALUS |
|---|
Description | Excessive accumulation of cerebrospinal fluid (CSF) in subarachnoid space due to the anterior fontanel remaining open after 18 months. |
|---|
Causes | - Birth trauma
- Infection (encephalitis or meningitis)
- Brain tumor
- Excessive CSF production
|
|---|
Types | - Communicating – Excessive CSF production. Fluid may still flow.
- Non-communicating: The CSF flow is impeded or obstructed.
|
|---|
Factors | - Open fontanelle: can accommodate
- Close fontanelle: increased chance of brain damage
|
|---|
Sign and symptoms | Infant: Toddler: |
|---|
Nursing management | - Assess head circumference daily
- Protect head with egg mattress
- Induce hypocapnia (increased O2) for cerebral vasoconstriction
- Limit fluid intake to 1200-1500 mL per day
- Prevent increased ICP:
- Prevent crying
- No restraints
- No valsava maneuver
- Padded side rails for seizures
|
|---|
Medical management | - Osmotic diuretics (mannitol)
- Loop diuretics (furosemide; potassium wasting)
- Corticosteroids (dexamethasone)
- Analgesics
|
|---|
Surgical management | - Ventriculostomy: To relieve pressure
- Ventriculoperitoneal shunt: To bypass fluid to peritoneum and so capillaries absorb the fluid
|
|---|
Contraindications | - Aspirin and ibuprofen bc increases risk for bleeding
- DOC: acetaminophen
|
|---|
NEURAL TUBE DEFECT |
|---|
Description | Complete closure of spinal column |
|---|
Causes | - Folic acid deficiency during pregnancy
- Drugs (antidepressants), radiation (x-ray), and hereditary.
|
|---|
Types | - Spina bifida (occult)
- Spina bifida cystica
- Most common
- With sac (thin and transparent)
- Types of spina bifida cystic
- Meningocele: with CSF and meninges
- Myelomeningocele: with CSF, meninges, and spinal cord
|
|---|
Sign and symptoms | - Flaccid paralysis of legs
- Altered bowl and the bladder
- Hip and joint deformities
|
|---|
Diagnostics | Assessment and inspection |
|---|
Nursing management | - Protect sac
- Cover with moist sterile gauze (nonadhesive and with PNSS)
- Place in prone position
- Use aseptic technique
- Monitor for signs of rupture
- Goal: no pressure, no injury, no infection
|
|---|
Medical management | - Surgical closure with 24-48 hours after birth
- Post-surgical management
- Rehabilitation
- Bowel and bladder elimination
- Proper growth (pt and to)
|
|---|
SEIZURES |
|---|
Description | - Involuntary contractions of muscles
- Caused by abnormal electrical brain discharges (excitable? tremors?)
- Increase CNS stimulation
|
|---|
Causes | - Idiopathic
- Infection (Meningitis); Brain is irritated
- Trauma
- Hypoglycemia (cold stress hypothermia)
|
|---|
Sign and symptoms | - Newborn
- Difficult to recognize
- Abscenciet/Blak - twitching
- Seizure - Slight? cyanosis? (mouth)
- Apnea
- Limp? / flaccid
- Infant/toddler
- Infantile Spasm
- Myoclonic Seizure
- Slump forward
- Falls from standing position
- Rapid movement of the trunk?
- Stiffening? Contraction of the body
- 3 years old and above
- Febrile
- Fever is cured
- Seizure
- Can last 1-2 minutes
- TSB Fields: VT?
- 5x: diarrhea
- Cool down?
|
|---|
Diagnostics | - CT
- Electroencephalography
- EEG = Brain activity
- Decreased oxygen in the brain
|
|---|
Nursing management | - Maintain the patient's airway and promote safety
- Clean the area of objects
- Protect the head
- No restraint bc it can lead to fracture
- Loose clothing
- Face head to the side after the episode
- Note the time of seizure
- Seizure:
- Suction (machine)
- Oxygen (mask)
|
|---|
MENINGITIS |
|---|
Description | - Infection of cerebral meninges
- Irritated brain and spine
|
|---|
Causes | - Bacterial
- Streptococcus
- Pneumonia
- E. Coli
- Viral
- Haemophilus Influenzae
|
|---|
Sign and symptoms | - Upper respiratory tract infection
- Headache
- Opisthotonus (arching back)
- Seizures
- (+) Kernig’s Sign
- Knee (pain, resistance?, spasm)
- Cranial Nerve Paralysis
|
|---|
Diagnostics | - Lumbar Puncture
- CSF Analysis
- Increased WBC = increased cloudiness and protein
- Blood culture: To figure out what organism
|
|---|
Nursing management | - Place a patient on respiratory precautions for 24 hours after the start of antibiotic therapy
- Enclose, protect airway, and promote safety measures to prevent seizures
- Monitor and control temperature to prevent febrile seizures
- Perform neurological assessment
- Assess for changes in LOC and irritability
- Monitor intake/output
- Assess nutritional value and food
|
|---|
Medical management | - Antibiotics
- Cefoxitin
- Drink for allergy
- 3rd cephalosporin
- Penicillin G
|
|---|
SICKLE CELL ANEMIA |
|---|
Description | - Clumping of hemoglobin
- Hemoglobin A is replaced by hemoglobin S
|
|---|
Causes | - Autosomal recessive inherited disorder
|
|---|
Factors | - Fever, stress, dehydration
- Sickle cell crisis
|
|---|
Sign and symptoms | - Pain
- Tachycardia
- Murmur
- Cardiomegaly
- Chest pain (blocked heart)
- Dyspnea (blocked lungs)
- Jaundice (blocked liver)
|
|---|
| - Sickle Cell Crisis
- RBC destruction
- Enlarged liver and spleen
- Hemolytic crisis: RBC destruction
- Aplastic anemia - severe
|
|---|
Diagnostics | Sickle Diagnostics - blood test |
|---|
Nursing management | - Pain relief
- Inhalation
- Oxygenation
- Health education
- Adequate hydration
- Bed rest for decreased oxygen needs
- Prevent infection
|
|---|
Medical management | - Blood transfusion (PRBC)
- Acetaminophen / Narcotic analgesic
- Hydroxyurea: increase hemoglobin production
|
|---|
HEMOPHILIA |
|---|
Description | - Disorder in blood coagulation
- Client is prone to bleeding
|
|---|
Causes | - Sex-linked recessive trait
- Mother is the carrier
- Son is affected
- Father transmits to the daughter
|
|---|
Types | - Type A: factor VIII (most common)
- Type B: Christmas disease (factor IX)
- Type C: Factor XI
|
|---|
Sign and symptoms | - Early
- Continuous bleeding in the umbilical cord
- Can also be seen in early circumcision
- Late
- Bruising
- Gum bleeding
- Epistaxis
- Hemarthrosis (bleeding in the joint with pain, usually in the knees; defining sign)
|
|---|
Diagnostics | - Low level of partial thromboplastin time
- Normal level of platelet
|
|---|
Nursing management | - PGoals: control bleeding
- Hemarthrosis management
- Immobilize joint (using splint)
- Perform passive ROM for distal parts to prevent muscle contracture
- Contraindicated: ibuprofen, aspirin due to increased risk of bleeding
- DOC: Acetaminophen (hepatotoxic)
- One blood draw only
- WOF: Hepatitis in factor 8 medication administration
- Sports recommend: Swimming
- Soft-bristled toothbrush
- Protective gear
|
|---|
Medical management | - Transfusion: Factor VIII (principle: missing factor to transfuse)
- Cryoprecipitate, platelet concentration
- Desmopressin: stimulates the release of factor VIII
- Acetaminophen for pain relief
|
|---|
LEUKEMIA |
|---|
Description | - Abnormal proliferation of immature WBC (high innmats WBC)
- Cancer in the blood
- High WBC is infection; Low WBC is immunocompromised
- Bone marrow produces too much immature WBC thus produces less RBC and Platelet.
|
|---|
Causes | - Unknow
- Common: Acute lymphocytic anemia
|
|---|
Types | - Radiation
- Chemical exposure
- Genetic factor
- Common among boys
|
|---|
Sign and symptoms | - Low RBC production (anemia)
- Pallow, low-grade fever, lethargy
- Low platelet (bleeding)
- Bleeding
- Low mature WBC (infection)
- Fever, infection
|
|---|
Diagnostics | - Bone marrow aspiration at the posterior iliac crest
- WBC: normal
- HgB: low
- Platelet: low
|
|---|
Nursing management | - Anemia management
- Rest in between breastfeeding
- Oxygen therapy using sterile humidifier and face mask
- Bleeding management
- Soft bristle toothbrush
- Prevent bruising
- No aspirin or ibuprofen
- Infection management (pts who are immunocompromised)
- Isolation
- No fresh fruits, vegetables, and flowers
- Avoid crowds
- Wear surgical mask
- Proper handwashing (>20 secs; soap and water)
|
|---|
Medical management | - Chemotherapy: to target rapidly producing cells
- Alopecia (buy a wig; after 3-6 months the hair will grow back)
- Nausea and vomiting
- Fatigue
- Bone marrow transplantation
|
|---|
VENTRICULAR SEPTAL DEFECT |
|---|
Description | - Opening between right and left ventricle (goes back to right)
|
|---|
Sign and symptoms | - Brow sweating during feeding or when crying
- Mild: usually asymptomatic, with splitting s2 sounds
- Moderate: sweating during feeding, tachypnea, failure to thrive, and tachycardia
- Severe: with frequent respiratory infection
|
|---|
Diagnostics | - 2D echo (size, structure, and blood flow)
- Chest xray
|
|---|
Medical management | - Diuretics
- ACE inhibitors (prevent hypertension and decrease afterload)
- Inotropes (digoxin)
|
|---|
Surgical management | - Pulmonary artery banding
- Transcatheter closure
- AKA cardio catheterization
- Can be diagnostic and therapeutic
- Site of insertion: femoral artery
- Flat on bed for 4-6 hours after the procedure
- Prone to bleeding
|
|---|
ATRIAL SEPTAL DEFECT |
|---|
Description | - Opening between right and left atrium.
- Failure of foramen ovale to close
- Systemic congestion to the right side will lead to JVD
|
|---|
Sign and symptoms | - Swelling of the legs and feet
- Increase palpitation
- Neck vein distention
- Shortness of breath
- Heart murmur
- Fatigue
- Failure to thrive
|
|---|
Diagnostics | - 2D echo (size, structure, and blood flow)
- Chest xray
|
|---|
Medical management | - Aspirin: Prostaglandin inhibitor to close the structures (ductus arteriosus and foramen ovale)
- Prostaglandin keeps the structures open
|
|---|
Surgical management | - Open heart surgery
- Percutaneous catheter closure through femoral artery
|
|---|
PATENT DUCTUS ARTERIOSUS |
|---|
Description | - Opening between the pulmonary artery and aorta
- Blood goes back to the heart and causes lung congestion
|
|---|
Sign and symptoms | - Tachypnea
- Diaphoresis
- Difficulty feeding
- Heart murmur
- Weight loss
- *Machinery like murmur”
|
|---|
Diagnostics | - 2D echo (size, structure, and blood flow)
- Chest xray
|
|---|
Medical management | - NSAID: prostaglandin inhibitor
- Indomethacin administered intravenously 10-14 days of life
- Ibuprofen
- Digoxin and diuretics
- Give aspirin
|
|---|
Surgical management | - Surgical ligation
- Cardiac catheterization
|
|---|
COARCTATION IN THE AORTA |
|---|
Description | |
|---|
Sign and symptoms | - High BP in upper extremities
- Low BP in the lower extremities
- Bounding pulse in the arms (carotid pulse)
- Weak or absent pulse in the femoral pulses
|
|---|
Diagnostics | - 2D echo (size, structure, and blood flow)
- Chest xray
|
|---|
Nursing management | - Take 2 BPs; 1 arm and 1 leg
|
|---|
Medical management | - Alprostadil ICV maintains patency of ductus arteriosus before surgery
- Digoxin improved ventricular systolic function
- Betablocke (metoprolol) treats preoperative hypertension
- ACE inhibitors (for hypertension)
- Vasodilators (nittroprusside)
|
|---|
Surgical management | - Resection and end to end anastamosis
- Balloon angioplasty
|
|---|
TETRALOGY FALLOT |
|---|
Description | - 4 defining structural problems (VROP):
- Ventricular septal defect (VSD open)
- Right ventricular hypertrophy (RV mataba)
- Overriding Aorta
- Pulmonary stenosis (maliit na PA)
|
|---|
Sign and symptoms | - Overall cyanosis: low circulating oxygenated blood
- Blue baby
- Tet spells: position in knee to chest or squats
- Clubbing of fingers
- Main problem is hypoxia
|
|---|
Diagnostics | - 2D echo (size, structure, and blood flow)
- Chest xray
|
|---|
Medical management | - Alprostadil IV maintains patency of ductus arteriosus before surgery
- Beta-blocker: reduces RV spasm
- Oxygen
- Sedation using Morphine sulfate IV
|
|---|
Surgical management | - Blalock Taussig procedure: a small tube that connects the pulmonary artery and pulmonary vein to allow more blood flow to the lungs.
|
|---|
TRANSPOSITION OF GREAT ARTERIES |
|---|
Description | - Right ventricle – aorta — systemic
- Left ventricle – pulmonary artery – pulmonary circulation
- Needs patent foramen ovale and ductus arterioles to provide mixing of blood
|
|---|
Sign and symptoms | - Excessive left and right ventricular workload
- Cyanosis shows within hours after birth
- Signs of congestive heart failure
- Pulmonary hypertension
|
|---|
Diagnostics | - 2D echo (size, structure, and blood flow)
- Chest xray
|
|---|
Medical management | - Alprostadil IV maintains patency of ductus arteriosus before surgery
|
|---|
Surgical management | - Atrial switch operation
- Heart transplant.
|
|---|
TRANSPOSITION OF GREAT ARTERIES |
|---|
Description | - One trunk - pulmonary artery and aorta combine
- Noted with VSD
- Commonly seen in DiGeorge Syndrome
|
|---|
Sign and symptoms | - Cyanosis shows within horse after birth
- Signs of congestive heart failure
- Polycythemia vera
|
|---|
Diagnostics | - 2D echo (size, structure, and blood flow)
- Chest xray
|
|---|
Medical management | - Digoxin, diuretics, ace inhibitors
|
|---|
Surgical management | - Corrective surgery
- VSD patch
|
|---|
RHEUMATIC HEART DISEASE |
|---|
Description | - Autoimmune inflammatory disease of the connective tissue
|
|---|
Causes | - Group A beta-hemolytic streptococcus (also causes strep throat and acute glomerulonephritis)
|
|---|
Factors | - Strep throat 4-6 weeks ago
|
|---|
Sign and symptoms | - Musculoskeletal, cardiac muscle, skin, and CNS
- Aschoff bodies round nodules in the mitral valve (LA and LV) thus backflows to the lungs
|
|---|
Diagnostics | - Jones criteria
- Major
- Polyarthritis: multiple joint pain
- Chorea: involuntary purposeless movement of hand and shoulder, accompanied by grimacing (CNS involvement)
- Carditis: signs of tachycardia
- Erythema marginatum: muscular rashes on the skin
- Subcutaneous nodules (mitral valve prolapse)
- Minor
- Low-grade fever
- Diagnostic exams (blood test)
- Antibody
- C reactive protein
- ESR
- Anti streotiysin titer
- Presence of 2 major or 1 major and 2 minor plus a history of sore throat will confirm the diagnosis
|
|---|
Nursing management | - Decrease O2 demands of the heart (+ carditis)
- CBR (complete bed rest)
- O2
- Prevent further cardiac damage
- Safety precautions for chorea
- Safe environment
- Do not restrain
- Seizure precaution (CNS is irritable and excitable)
- Health hisory: ask if infant had strep throat 4-6 weeks ago
|
|---|
Medical management | - Penicillin: for the bacteria
- Aspirin or salicylate: RHD anti-inflammatory
- Question before giving aspirin: No history of viral infection (chicken pox or flu)
- SE and WOF: Reye’s syndrome is encephalopathy accompanied by infiltration of organs (heart and liver)
|
|---|
ASTHMA |
|---|
Description | - Hypersensitive response to allergens causing inflammation of the airway
- Exposure to allergens leads to the release of mast cells
|
|---|
Factors | - Pollen, molds, house dust, and food
- Exposure to cold air or changing temperature, irritating odors
- Cigarette smoke
- Aspirin
- Stress
- Strenuous activities
|
|---|
Sign and symptoms | - Pathognomonic/hallmark sign: Wheezing on expiration
- Central cyanosis in the mouth
- Inflammation (swelling and edema)
- Bronchoconstriction (CO2 trapping)
- Increased mucus production
|
|---|
Diagnostics | - Hx taking
- Skin test of different allergies
- Pulmonary function test: to check for lung vital capacity.
|
|---|
Nursing management | - Monitor breath sounds
- Upright position (high or semi-fowlers)
- Absent breath sounds (mother may think the baby is okay so auscultate again)
- Good: effective treatment
- Bad: total bronchoconstriction
- WOF: Status asthmaticus (no medication works at all)
- Emergency
- Carbon dioxide narcosis can cause death due to a lack of oxygen in the brain
- Will undergo mech vent
- The best sport for pt with asthma is swimming
|
|---|
Medical management | - Bronchodilator
- Mild: Albuterol (prevent bronchospasm)
- Moderate: Albuterol + cromolyn sodium (mast cell stabilizer)
- Sever: Bronchodilator, Corticosteroid (presence of inflammation, given first to open airway) + Albuterol
- IV fluids
- Metered dosed inhaler (MDI)
- Upright position
- Exhale completely
- Attach MDI to mouth
- Press and inhale
- Hold breath 5-10 secs
- Do not exhale right away
- Exhale slowly
- If corticosteroids:
- Nursing intervention: gargle after administration
|
|---|
CYSTIC FIBROSIS |
|---|
Description | - Thick, sticky fluid is seen in the lungs, GIT, and reproductive system.
- Defective chromosome 7 (exocrine).
- Lots of secretions in the lungs can lead to pneumonia and respiratory disease.
|
|---|
Cause | - Autosomal recessive disorder
|
|---|
Sign and symptoms | - Respiratory
- Frequent pneumonia
- Persistent cough with mucus
- Wet cough
- Wheezing
- Digestive (- lipase, - amylase)
- Steatorrhea (excessive amount of fats in the poop)
- Absent pancreatic enzymes (- lipase, - amylase)
- Diabetes (high glucose in blood vessels): if prolonged absence of lipase and amylase this can lead to diabetes. if not treated, can lead to nephropathy and retinopathy.
- Malnutrition
- Meconium Ileus: was not able to pass the first stool or constipated due to the poop being too thick.
- Reproductive
- Infertility
- Ectopic pregnancy
- Oligospermia (low sperm count)
- Delayed pub
|
|---|
Diagnostics | - Sweat test: high NaCl in sweat
- Normal: 40-60 mEq
- High: (+) sweat test
- Endoscopy: absence of pancreatic enzymes in the pancreatic and common bile duct.
|
|---|
Nursing management | - Respiratory management
- Principle of Pulmonary hygiene:
- Liquify, mobilize, and expectorate tenacious secretions
- Hydration
- Deep breathing and CPT
- Coughing and suctioning
- CPT: before postural drainage
- O2 suction
- Postural drainage
- 2-3 hours before meal to prevent vomiting
- Digestive management
- High protein, high calorie, low fat
- WOF: absence of steatorrhea
- Increase OFI
|
|---|
Medical management | - Respiratory
- Bronchodilators
- Antibiotics
- Mucolytics (decrease mucus production)
- Digestive
- Cotaym (synthetic pancreatic enzymes; given after every meal; if effective (-) steatorrhea)
- Multivitamins: ADEK (K is for coagulation; D is for synthesizing calcium; A is for color blindness; E is for the skin)
- Reproductive
- In Vitro Fertilization (3-5 eggs)
|
|---|
SUDDEN INFANT DEATH SYNDROME (SIDS) |
|---|
Description | - Sudden death of a HEALTHY infant less than 1 year old
|
|---|
Factos | - 1-6 months (learns turning and may suffocate)
- Preterm (immature lungs)
- Sleep position (prone position)
- Nicotine exposure
- Socioeconomic
- Bedding (too much bedding)
- Lack of knowledge of the parents (health teaching)
|
|---|
Sign and symptoms | |
|---|
Diagnostics | - Sweat test: high NaCl in sweat
- Normal: 40-60 mEq
- High: (+) sweat test
- Endoscopy: absence of pancreatic enzymes in the pancreatic and common bile duct.
|
|---|
Nursing management | - Sleep in a supine position
- Bedding
- Firm mattress
- No toys, blankets, or pillows
- Avoid overdressing
- Avoid smoking
- No co-bedding (parent sleeps beside the infant)
- Normal room temperature
- So not leave a bottle of milk
- Educate parents during postpartum (educate abt the risk)
- For grieving parents
- Allow expression of feelings and concerns (therapeutic communication; the goal is converse)
- Let them hold the baby (to overcome denial)
- WOF mother’s feelings of guilt (may lead to depression and suicide)
|
|---|
FOREIGN BODY ASPIRATION |
|---|
Description | - Inhalation of foreign body in the airway
|
|---|
Factors | - Infants and toddlers bc site of gratification is mouth
- Presence of small objects
- Crawling by 9 months
- Unsupervised
|
|---|
Sign and symptoms | - Chocking
- Hard forceful cough
- Airway obstruction: cough with no sound
- Stritor indicates partial obstruction
- Cyanotic
- Inability to cry
|
|---|
Nursing management | - Infant
- Back thrusts
- Prone over your arm and administer 5 quick back blows forcefully between the infant’s shoulder blades using the heel of the hand.
- Child
- Subdiaphragmatic abdominal thrusts
- Adolescent
- If able to cough, encourage
- If cannot cough, do abdominal thrusts
|
|---|
CLEFT LIP AND CLEFT PALATE |
|---|
Description | - Congenital anomaly: failure of soft tissue or bony structure to fuse during embryonic development
|
|---|
Factos | - Genetic
- Radiation
- Rubella virus (german measles; rubella is measles) infection that commonly causes cleft lip.
- Medication (valproic; anti manic or mood stabilizer)
- Male: lip
- Female: palate
|
|---|
Sign and symptoms | - Frequent infection
- Dry mucus membrane
- Mild retained in folds
- Milk, aspirated, airways
|
|---|
Diagnostics | - In utero sonogram
- Inspection lip.
|
|---|
Nursing management | - Focus on aspiration of milk and nutrition.
- Asses ability to suck, swallow, and breathe during breastfeeding
- Monitor weight due to risk of malnutrition (-) breastfeeding
- Modifying feeding technique
- Use enlarged nipple bottle (block the opening of lip or palate to direct milk to the esophagus)
- Hold upright
- Direct bottle to the side of buccal mucosa and black of the mouth
- Burp after feeding
|
|---|
Medical management | - Lip: Cheiloplasty
- Palate: Palatoplasty
|
|---|
Category | CLEFT LIP | CLEFT PALATE |
|---|
Gender | Boys | Girls |
|---|
Clinical Findings | Dry mucous membrane Accumulation of dry milk in folds | Dry mucous membrane Accumulation of dry milk in folds |
|---|
Feeding | Using a rubber medicine dropper | Using a big nipple feeding bottle |
|---|
Repair Timing | Can be done by 2 ½ to 3 months | Can be done by 12-18 months |
|---|
Surgical Procedure | Cheiloplasty | Palatoplasty |
|---|
Checklist for Surgery | 10 weeks old 10 hemoglobin level 10 lbs in body weight Suture is outside | Done before speech development (>6 months) After palate development Suture in inside |
|---|
Position Post-op | Supine | Side lying or pillow at the back to reduce the risk of aspiration |
|---|
Watch Out For | NONE | Bleeding symptoms such as frequent swallowing and stained red |
|---|
Post-op Care | Restrained elbow (to prevent traumatizing suture line) Use Logan bar (to ensure suture is kept intact and prevent it from opening) | Restrained elbow (to prevent traumatizing suture line) Use Logan bar (to ensure suture is kept intact and prevent it from opening) |
|---|
Post-op Risks | Otitis media Improper teeth growth | Otitis media Improper teeth growth |
|---|
Follow-up | Child psychologist Speech therapist Ear, nose, and throat doctor Orthodontist for teeth | Child psychologist Speech therapist Ear, nose, and throat doctor Orthodontist for teeth |
|---|
TRACHEOESOPHAGEAL FISTULA |
|---|
Description | - Abnormal connection between esophagus and trachea
- Risk for aspiration for all types of tracheoesophageal fistula
|
|---|
Factos | - During pregnancy: polyhydramnios (increase in amniotic fluid)
- If has large stomach but AOG is far (polyhydramnios) which means the baby is unable to swallow the amniotic fluid.
|
|---|
Sign and symptoms | - Seen typically during breastfeeding:
- Coughing
- Choking
- Cyanosis
|
|---|
Diagnostics | - During insertion of NGT there is the coiling of catheter bc may ending
- Xray
- Ultrasound
|
|---|
Nursing management | - Pre-op management
- Suctioning
- Place on NPO (placed on TPN and D5LR when baby is malnourished and dehydrated)
- Offer pacifier (decrease stress when mouth us busy)
- WOF: aspiration
- Complication: pneumonia
- MEasurement of NGT
- Adult: ear, nose, xiphoid process
- Infant: nose to xiphoid process
- Must have water or saliva to swallow during insertion
|
|---|
Medical management | - Repair bc airway is a concern
- Nutrition: TPN or gastrostomy tube
- Surgery
- Anastamosis: stitching of two closed endings to create a passageway
- Closure of fistula: close the connection between the esophagus and trachea
|
|---|
PYLORIC STENOSIS |
|---|
Description | - The pyloric sphincter is the opening between the lower portion of the stomach and the beginning portion of the small intestine (duodenum).
- Any stricture that causes it to tighten
|
|---|
Factos | - During pregnancy: polyhydramnios (increase in amniotic fluid)
- If has a large stomach but AOG is far (polyhydramnios) which means the baby is unable to swallow the amniotic fluid.
|
|---|
Sign and symptoms | - Hallmark: olive-shaped mass at epigastrium
- Visible peristaltic wave
- Accumulated food in the stomach
- Projectile vomiting
- No bile in vomitus
|
|---|
Nursing management | - Common complication of vomiting is diarrhea
- Give hydration and IV
- Monitor for signs of dehydration
- Oliguria (oliguria; low UO and anuria; no UO)
- Fluid volume deficit
- Dry mucus membrane, skin tenting sunken fontanelles, fever, decrease urine output, and weight loss.
- WOF: hypokalemia (due to vomiting)
- WOF: signs of metabolic alkalosis leading to hypochloremia, hypokalemia, and starvation
- Withhold oral feeding
- Provide pacifier
|
|---|
Medical management | - IV fluids
- Pylorotomy: incision through muscle fibers of the pylorus through laryngoscopy
|
|---|
INTUSSUSCEPTION |
|---|
Description | - Telescoping of the intestine usually in the junction of the large and small intestine
- Distal ileum (small intestine) and proximal colon
|
|---|
Sign and symptoms | - Hallmark sign:
- Sausage shape mass
- Currant jelly stool: mucus and blood (due to frequent friction when telescoping leads to scraping of cells and bleeding. To lessen the friction and protect the lining, the stomach releases mucus)
- Vomiting with bile (after if the vomit has bile)
- Distened abdomen
- Abdominal pain
|
|---|
Diagnostics | - Ultrasound: to visualize telescoping
|
|---|
Nursing management | - Post-op; WOF: short bowel syndrome (small intestine cannot absorb enough nutrients)
- Diarrhea
- Dehydration
- Complication: enterocolitis due to collection of meconium ileus (no passage of 1st stool). Leads to sepsis
- Fever, bleeding, bloody diarrhea, or explosive diarrhea
- Diet: low-residue diet
- Temporary treatment is abdominal wall stoma.
- Colostomy care:
- Pink is normal
- Red is infection
- Purple is no blood supply
|
|---|
Medical management | - Barium enema introduces force and lengthens the intestine which results in explosive diarrhea
- Bowel resection: surgery to remove part of the small intestine, and large intestine or both.
- Temporary colostomy in the abdominal wall
- Abdominoperineal pull-through (12-18 months)
|
|---|
HIRSCHSPRUNG’S DISEASE |
|---|
Description | - Aganglionic megacolon: lowers motility usually in the sigmoid colon due to the absence of ganglionic innervation
- No nerves in the sigmoid colon (last part of the large intestine in the left side of the abdomen) leading to no peristalsis and constipation
|
|---|
Sign and symptoms | - Hallmark sign: Ribbon-like stool due to smaller and twites rectum and anus
- Newborns: failure to pass meconium with 24 hours
- Constipation
- Distended abdomen
|
|---|
Diagnostics | - Abdominal x-ray
- Barium enema (chalky white substant which is secreted via stool
- Provide Health teaching that the stool will be white after the procedure until all for the substance is excreted
|
|---|
CELIAC DISEASE |
|---|
Description | - Against gluten food for life
- Gluten spruce
- GLuten intolerant
- Ingestion of gluten leads to intestinal villi atrophy
- Undigested fats and protein
|
|---|
Sign and symptoms | - Diarrhea
- Steatorrhea (high-fat content in stool; poops float)
- Anorexia (due to no absorption of nutrients)
- Abdominal pain and distention (bc gusto iexcrete agad)
- Deficiency in vitamin ADEK
- Ricketssia: brittle bones that can lead to fracture due to vitamin d deficiency
- Low platelet count: bleeding management due to vitamin K deficiency
|
|---|
Diagnostics | - History (food diary, what the person ate)
- Biopsy of the intestinal mucosa (damage due to prolonged intake of gluten)
|
|---|
Nursing management | - WOF: celiac crisis
- Factor: infection
- Complication:
- Frequent: metabolic acidosis and hyperkalemia due to diarrhea and vomiting.
- Hyperkalemia is due to the exchange of hydrogen and vit k. Vit k goes to the blood as a coping mechanism.
- Health teaching:
- Avoid: baked goods, bread, crackers, pasta, breading.
- Monitor growth
- School-age children teach them to read the ingredients
|
|---|
Medical management | - Celiac diet
- NO BROW (barley; bread, rye; beer, oat; oatmeal, and wheat; wheat bread)
- IV fluids to control the electrolyte imbalances
|
|---|
PHENYLKETONURIA |
|---|
Description | - Problem in metabolism of phenylalanine (type of amino acid which is from protein; typically found in milk)
- Phenylalanine is needed for thyroxine (can affect IQ) and melanin (white skin; prone to skin cancer)
|
|---|
Sign and symptoms | - Thyroxine deficiency
- Low IQ
- Melanin deficiency
- Non pigmented skin, skin rash
- Blond hair, fair, skin, blue eyed
- High unconverted phenylalanine
- Incerease phenylalanine can lead to the production of pyuric acid leads to metabolic acidosis
- High fat (lipoprotien) breakdown leads to ketones which are the byproduct
|
|---|
Diagnostics | - Guthrie test
- Heel prick in the side
- 24 hours after birth
|
|---|
Nursing management | - Phenylalanine free diet
- No dairy
- High protein food like meat and eggs
- Aspartame (artificial sweeteners)
- Allowed: vegetable, fruits, low protein
- Milk replacement: Lofenalac
|
|---|
NEWBORN SCREENING |
|---|
Congenital adrenal hyperplasia | - Decreased cortisol, serve salt loss.
- Inability to utilize an essential amino acid, leading to dehydration.
- If not treated can lead to death in 9-13 months
- Treatment: NaCl supplement (tablet or food like canned food)
|
|---|
Galactosemia | - Inability to metabolize galactose in milk
- Signs and symptoms: Vomiting, diarrhea, liver damage
- Complications: cataract, growth failure, and brain damage (due to storage)
- Treatment: No animal source milk and No breastfeeding
- So instead give soy formula: Isomil, nursery, prosobee
|
|---|
Phenylketonuria (PKU) | - Inability to metabolize phenylalanine, leading to mental retardation if not treated.
- Phenylalanine is converted to tyrosine, which is essential for melanin production (may cause hypopigmentation).
- Treatment: Special formula (e.g., Lofenalac/Phenalac)
|
|---|
G6PD (Glucose-6-Phosphate Dehydrogenase) Deficiency | - Breakdown of RBC causing anemia
- Treatment: avoid triggers like beans, naphthalene, sulfate
|
|---|
Congenital hypothyroidism (cretinism) | - Deficiency in thyroid hormones causing physical, developmental, and mental delays.
- Treatment includes thyroid hormone supplements for life (e.g., Synthroid).
|
|---|
NEPHROTIC SYNDROME |
|---|
Description | - Nephrosis
- Acute glomerular permeability (colloids)
- Acts like a filter of glucose and protein
|
|---|
Cause | |
|---|
Factors | - 3 years old
- Common in boys
- SLE (systemic lupus erythema)
- Sickle cell anemia
|
|---|
Sign and symptoms | - Severe proteinuria (albumin; connected to edema bc it keeps water inside blood vessel)
- Edema (extreme) due to colloid oncotic pressure (usually albumin)
- Hypoalbuminemia and Hyperlipidemia
- Cause of liver production of lipoprotein
- Arteriosclerosis: spasm of blood vessel
- Atherosclerosis: caused by high cholesterol
|
|---|
Diagnostics | - Renal biopsy
- CBC: low level of protein
- Urinalysis: high level of protein
|
|---|
Nursing management | - Edema care
- Risk for pressure or skin ulcers
- Edema goes to prominent boney parts
- Diet: high protein, low sodium diet (where salt goes, water follows)
- Health teaching for corticosteroid therapy
- Do not stop abruptly (weaning: lower dosage and frequency)
- Side effects: Moon face (cushing syndrome
- Long term immunisuppresion may occur
- Facemask
- Hand washing
- NO fresh flowers or fruits
|
|---|
Medical management | - IV corticosteroids: treatment edema and protien loss (prednisne)
- IV albumin
- Cyclophosphamide, cyclospoine (pathophysio autoimnesI: immunosuppresors
- Anticholesterol: atorvastatin
|
|---|
NEPHRITIC SYNDROME |
|---|
Description | - Inflammation of glomeruli of kidney
|
|---|
Cause | |
|---|
Factors | - 5-10 years old
- Common in boys
- History of sore throat or tonsillitis
|
|---|
Sign and symptoms | - Hematuria: “tea-colorer” or smokey urine
- Some protein
- Oliguria
- Hypertension
- Increased BUN and Crea (more sensitive) in blood levels
|
|---|
Diagnostics | - Kidney function test
- Anti-streptolysin titer
- 24-hour total urine
|
|---|
Nursing management | - Health teaching: self-limiting disease for 1-2 weeks
- Monitor weight
- Diet: high protein and low salt
- Bed rest
- Antihypertensives
- Skincare
- WOF: congestive heart failure
- Treatment: Diuretics, oxygen, digoxin
- Fluid accumulation
- FVE, crackles, JVD, HTN, bounding pulse.
|
|---|
Medical management | - Diuretics
- Antibiotics: penicillin
- Antihypertensives
|
|---|
NEPHROBLASTOMA |
|---|
Description | - Most common intraabdominal and kidney tumor
- Cancer of children
|
|---|
Cause | - Genetic
- Congenital abnormalities
|
|---|
Factors | |
|---|
Sign and symptoms | - Swelling or mass within the abdomen
- Urinary retention
- Hematuria
- Anemia: pallor, anorexia, lethargy
- Hypertension (secretion of renin; ace inhibitor angiotensin receptor)
|
|---|
Diagnostics | |
|---|
Nursing management | - Avoid palpation of the abdomen
- WOF: the rupture of tumor
- Pre-op:
- Monitor vital signs
- Measure abdominal girth once daily
- Post-op:
- Monitor temp and blood pressure
- Monitor for signs of hemorrhage and infection
- Strict I&O
- Monitor for abdominal distention
- Monitor for intestinal obstruction
|
|---|
Medical management | - Surgery: partial or total nephrectomy
- Chemotherapy
|
|---|
CONGENITAL HIP DYSPLASIA |
|---|
Description | - Head of femur is above the acetabulum
|
|---|
Cause | - Inherited
- Mechanical breech position
- Presence of relaxin hormone (relaxes pelvic joints and causes waddling gait)
|
|---|
Factors | - Girls
- Sociocultural methods of carrying
|
|---|
Sign and symptoms | - Affected leg is shorted
- Galeazzi sign: one knee is lower
- Ortolani’s sign: clicking
- Barlow’s sign: Feeling of the femur head slipping out
- Unequal number of skin folders on thigh and glutes
|
|---|
Diagnostics | |
|---|
Nursing management | - Position
- Hip and legs are flexed and are abducted (externally rotated)
- Initial intervention
- Two or three diapers
- Carrting at the hip
- Cast care (Hip spica cast)
- Neurovascular check
- WOF: Compartment syndrome (pallor, paresthesia, pain, pulselessness, poikilothermia)
|
|---|
Medical management | - Frejka splint
- Pavlik harness
- Spica cast
|
|---|
SCOLIOSIS |
|---|
Description | - Skeletal disorder; curvature of the spine
|
|---|
Factors | - Family history
- Common in adolescent girls
|
|---|
Sign and symptoms | - Kyphosis: Excessive outward curvature of the spine; hunched back
- Lordosis: Excessive inward curvature of the spine; swayback appearance
- Uneven length in bra straps
- Uneven length in skirt
|
|---|
Diagnostics | |
|---|
Nursing management | - Usuall diagnosed by the school nurse:
- Adam’s test: bending down infront of nurse
- Starts at 8 years old
- Sports recommended: yoga and swimming
- Common problems: body image and low self esteem
- Bawal shoulder bags
- Post op care:
- Log rolling technique (pt is imobalized and is moved in one go)
- Flat on bed
|
|---|
Medical management | - Milwaukee breace
- For mild scoliosis (more than 20 degrees)
- Worn 16-23 hours per day (except during sleep)
- Do not loosen
- Thin clothing
- Halo traction
- For severe scoclosis
- Corrective surgery
- Use of pins, rods, and screws
|
|---|
FRACTURE |
|---|
Description | - Break in the continuity of the bone
|
|---|
Factors | - Age (preschool to school age)
- More porous and bone immaturity
|
|---|
Sign and symptoms | - Pain, swelling
- Deformity
- Uneven gait
|
|---|
Diagnostics | |
|---|
Nursing management | - Thorough assessment (rule out abuse)
- IV line access (increased bleeding and open fracture)
- Reduce anxiety of client
- WOF complications:
- Fat embolism (long bone fracture)
- Compartment syndrom
- Health teaching on spleent or cast care
- Keep dry; do not sue hair dryer in warm setting (use palm not fingers)
- Do not insert objects
|
|---|
Medical management | - Initial intervention
- RICE:
- Rest (immobalize)
- Ice with first 24 hours (reduce swelling) (hot after 24 hours for increased blood prefusion)
- Compression (reduce bleeding)
- Elevate (reduce edema)
- Tetanus shot
- Splint
- Cast
|
|---|
PEDICULOSIS CAPITIS (LICE) |
|---|
Description | - Infestation of lice in hair and scalp
|
|---|
Cause | - Lice
- Female eggs on hair shaft
- Incubation: 7-10 days
- Transmission: direct (person to person) or indirect contact (hygeine items like combs)
|
|---|
Factors | |
|---|
Sign and symptoms | - Common site:
- Occipital
- Behind ears
- Eyebrows and eyelashes
- Scratching
- Pruritus
- Irritability
|
|---|
Diagnostics | |
|---|
Nursing management | - Have family checked
- Health teaching
- Use fine tooth comb
- Do not share items
- Bedding anf clothing should be laundered in hot water
- Keep non-essential clothes and toys for 2 weels
- Daily vaccuming
|
|---|
Medical management | - Pediculicide (death)
- Contraindicated for 6 months and below
|
|---|
SCABIES |
|---|
Description | |
|---|
Cause | - Sarcoptes scabiei (itch mite)
- Incubation:
- Eggs hatch:
- Mode of transmission: contact
|
|---|
Factors | |
|---|
Sign and symptoms | - Pruritic papular rash
- Burrow into the skin
|
|---|
Diagnostics | |
|---|
Nursing management | |
|---|
Medical management | - Lindane shampoo
- Contraindicated: 2 years old and below
- Adverse effece: seizure and neurotoxicity
- Permethrin (lotion)
- Applied to cool dry skin
- Applied on all skin
|
|---|
LEAD POISONING |
|---|
Description | |
|---|
Cause | - Exposure to dust, soil
- Adults: plumber, smoker, mechanic
- Near cars and highways
- Pencils, paint, and crayons
|
|---|
Factors | - Toddlers with pica (eating anything edible or not; paint chips)
|
|---|
Sign and symptoms | - CNS
- Permanent cognitive impairment
- Mental retardation
- Renal
- Renal failure: oliguria and hematuria
- Hematology
- Anemia: fatigue, forgetfulness, fainting
- Pallow
|
|---|
Diagnostics | - Blood test
- Normal: 5 mcg/dL
- Toxic: 15 mcg/dL
|
|---|
Nursing management | - Before therapy
- Check for kidney function (BUN and Crea) bc lead is excreted via the urine
- Adequate hydration
- Provide health teaching
- Supervision in playgrounds
- Safe toys
- Monitor children with pica
|
|---|
Medical management | - Chelation therapy
- Calcium disodium edetate
- Succimer
- Based on british anti lewisite:
- Route: IM or IV
- Contraindicated: pt with peanut allergy, G6PD
- Ethhelynneediamine tatraacetic acid (EDIA)
|
|---|
ACETAMINOPHEN OVERDOSE |
|---|
Description | - Acetaminophen is hepatoxic
|
|---|
Cause | - Toxic dose of 150 mg/kg or higher in children
|
|---|
Factors | - Amount ingested
- Length of time before treatment
- Intentional
- History of liver failure
|
|---|
Sign and symptoms | - First 2-4 hours
- Malaise (generalized fatigue)
- Nausea and vomiting
- Sweating, pallor, weakness
- Hepatic
- RUQ pain
- Jaundice
- Confusion and stupor (hepatic encephalopathy)
- Elevated liver enzymes
- Prolonged Prothrombin time (low levels of vit K)
|
|---|
Diagnostics | - Blood test
- Rumack Matthew Nomogram: test for acetaminophen
- What was ingested?
- What time ingested?
- What time was seen on the flood?
|
|---|
Medical management | - Less than 4 hours: paracetamol at 4 hours post-ingestion
- 4-8 hours post-ingestion: N-Acetylcysteine, add to juice or soda
- If unconscious use gastric lavage and activated charcoal
|
|---|
ACETYLSALICYLIC ACID (ASPIRIN) |
|---|
Cause | - Household cleaners, detergents, bleach, paint, batteries
|
|---|
Sign and symptoms | - WOF: airway patency
- Burned Mouth, Throat, and Stomach:
- Edema in tongue, lips, pharynx
- Vomiting
- Drooling and inability to clear secretions
|
|---|
Nursing management | - Emergency Room:
- Assess the child:
- Terminate exposure to the poison
- Identify the poison
- Take measures to prevent absorption of the poison
- Document event and assessment findings
- At Home:
- Move the child away from harm
- Call Poison Control Center
- Inform (if known):
- Substance ingested
- Time seen
- Signs and symptoms
|
|---|
Medical management | - Dilution of corrosive water or milk: To reduce the corrosive's strength.
- Contraindicated:
- Induced vomiting
- Neutralization (No activated charcoal, as it can cause burns)
|
|---|