4.1: Human reproduction
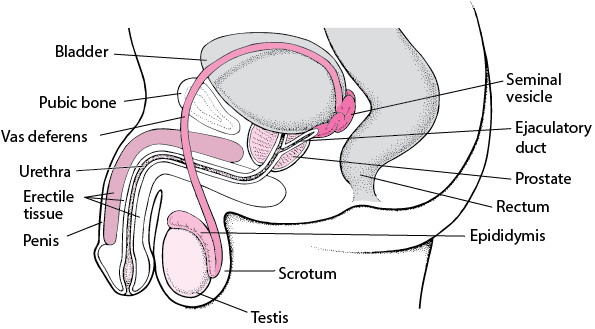
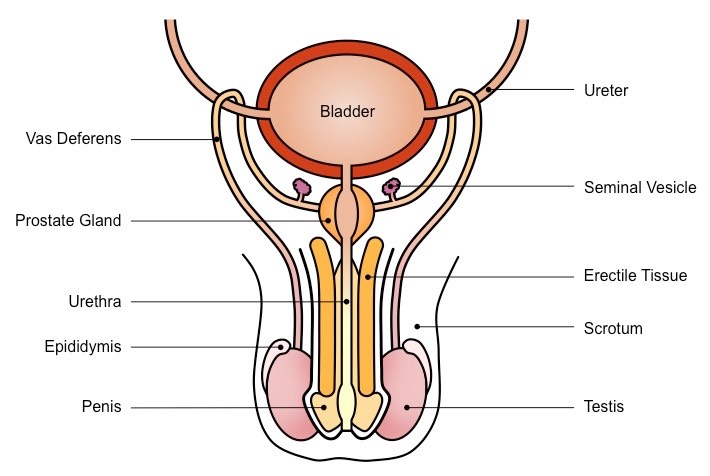
Male reproductive system
This consists of:
The penis.
A pair of testes contained in outer sacs known as scrotums.
Ducts connecting the testes with the penis.
Accessory glands, such as the pair of seminal vesicles, Cowper’s glands and the singular prostate gland.
They secrete fluids to mix with the sperm to make semen.
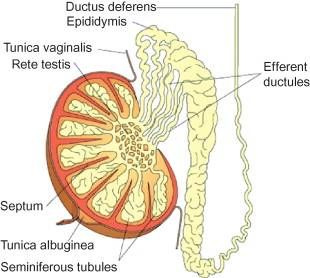
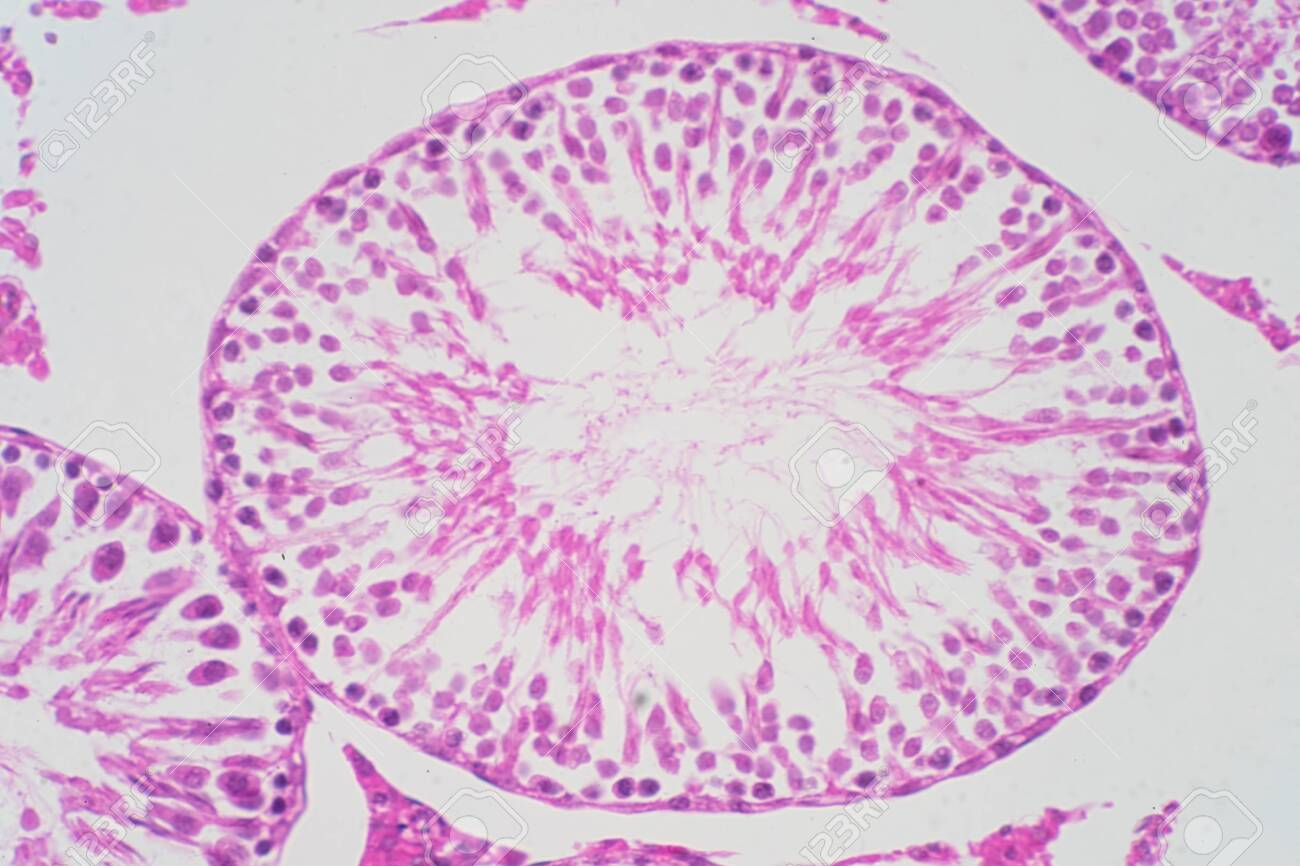
Testes
In each testis there are around a thousands coiled tubes known as seminiferous tubules.
The germinal epithelial cells lining these undergo spermatogenesis, and once matured they move towards the lumen and collect in the vasa efferentia.
This is another set of tubes which moves the sperm to the head of epididymis.
They remain here until they are motile.
They then move to the vas deferens during ejaculation.
Vas deferens
This carries sperm from the epididymis to the penis.
Seminal vesicles secrete mucus into the vas deferens, which contains chemicals such as fructose which is respired by the sperm for energy.
The spermatozoa and seminal fluid then move though the ejaculatory duct, which passes through the prostate gland.
This secretes prostate fluid containing zinc.
This fluid is then referred to as semen, containing spermatozoa, seminal and prostate fluids.
It is then carried through the penis via the urethra.
These secretions:
Maintain sperm motility.
Provide nutrients, such as fructose, amino acids and zinc ions.
Are alkaline, to:
Neutralise any remaining acidic urine in the urethra.
Neutralise the acidic vaginal tract.
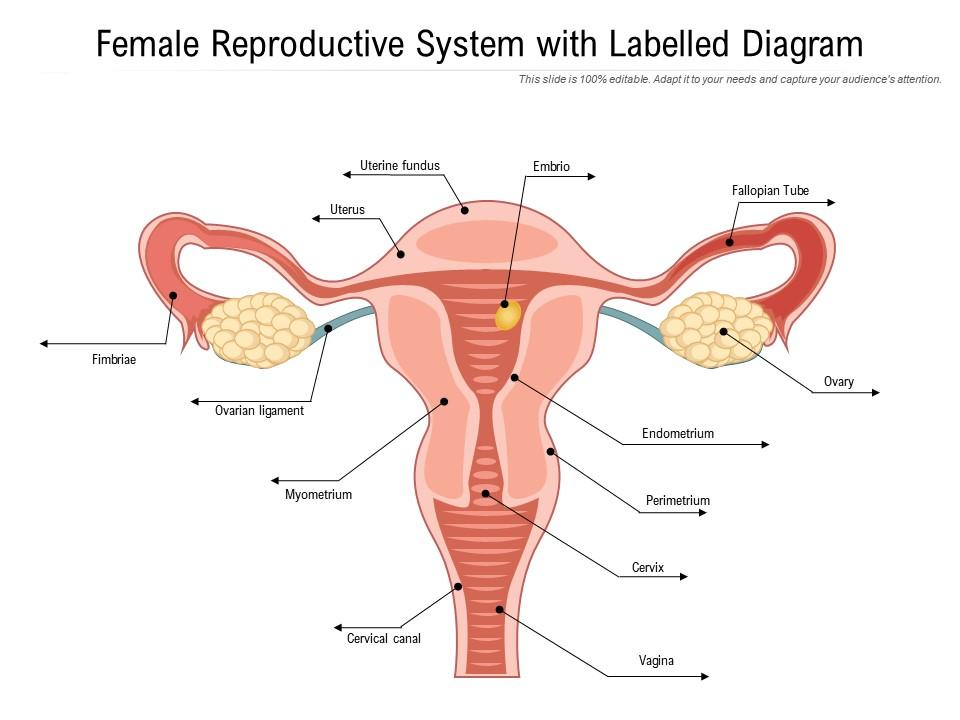
Female reproductive system
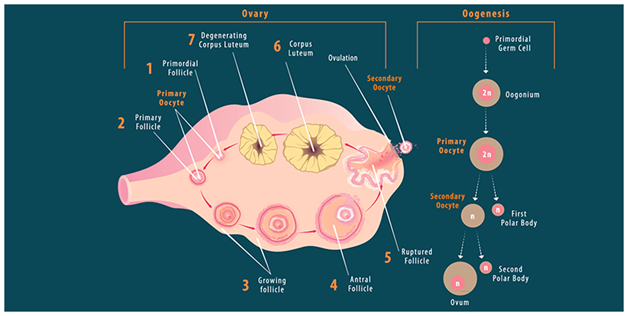
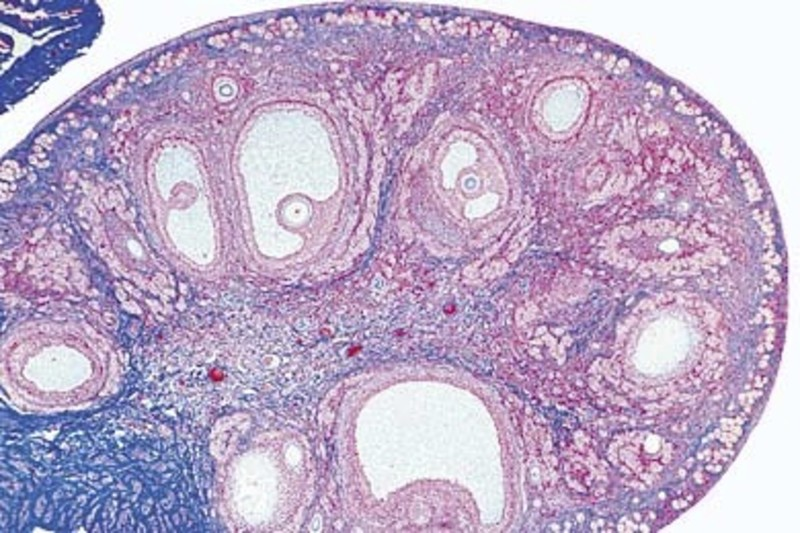
Ovaries
There are two, and they are inside the body.
Oocytes mature in follicles, which develop from cells in the germinal epithelium.
Mature follicles then migrate to the surface of the ovary, and release a secondary oocyte at ovulation.
The ovary responsible alternates each month.
The cilia at the entrance of the oviducal funnel sweeps the secondary oocyte into the oviduct, AKA fallopian tube.
The ciliated epithelium throughout conveys the secondary oocyte to the uterus.
Uterus
The uterus has three layers:
Perimetrium, the outermost layer. A thin layer around the outside.
Myometrium, the muscle layer.
Endometrium, the innermost layer. A mucous membrane with a good blood supply. It is shed monthly unless an oocyte is fertilised.
The uterus then opens into the vagina through the cervix, a narrow ring of connective tissue and muscle.
Vagina walls are also muscular, and open at the vulva.
Gametogenesis
This is the term for the production of gametes.
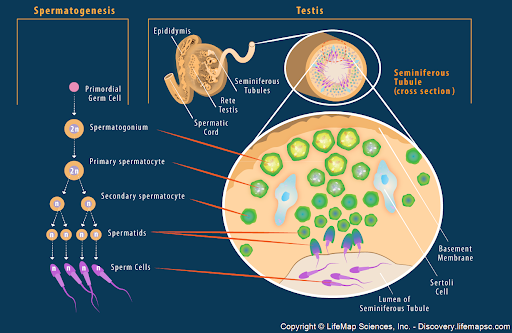
Spermatogenesis
The diploid germinal epithelium cells, which line testes, start by undergoing mitosis to make diploid spermatogonia and more germinal epithelial cells.
These diploid spermatogonia then divide many times by mitosis and enlarge, becoming primary spermatocytes and more spermatogonia.
Primary spermatocytes then undergo meiosis 1, which makes haploid secondary spermatocytes.
Secondary spermatocytes undergo meiosis 2, which makes haploid spermatids.
These spermatids mature into spermatozoa.
Also in the testes are sertoli cells, which secrete a fluid which nourishes spermatids and protect them from the male’s immune system.
Additionally, there are groups of cells known as interstitial cells, or Leydig cells. These secrete testosterone, which is the male sex hormone with roles in sperm formation and maturation, and the development of male secondary sex characteristics.
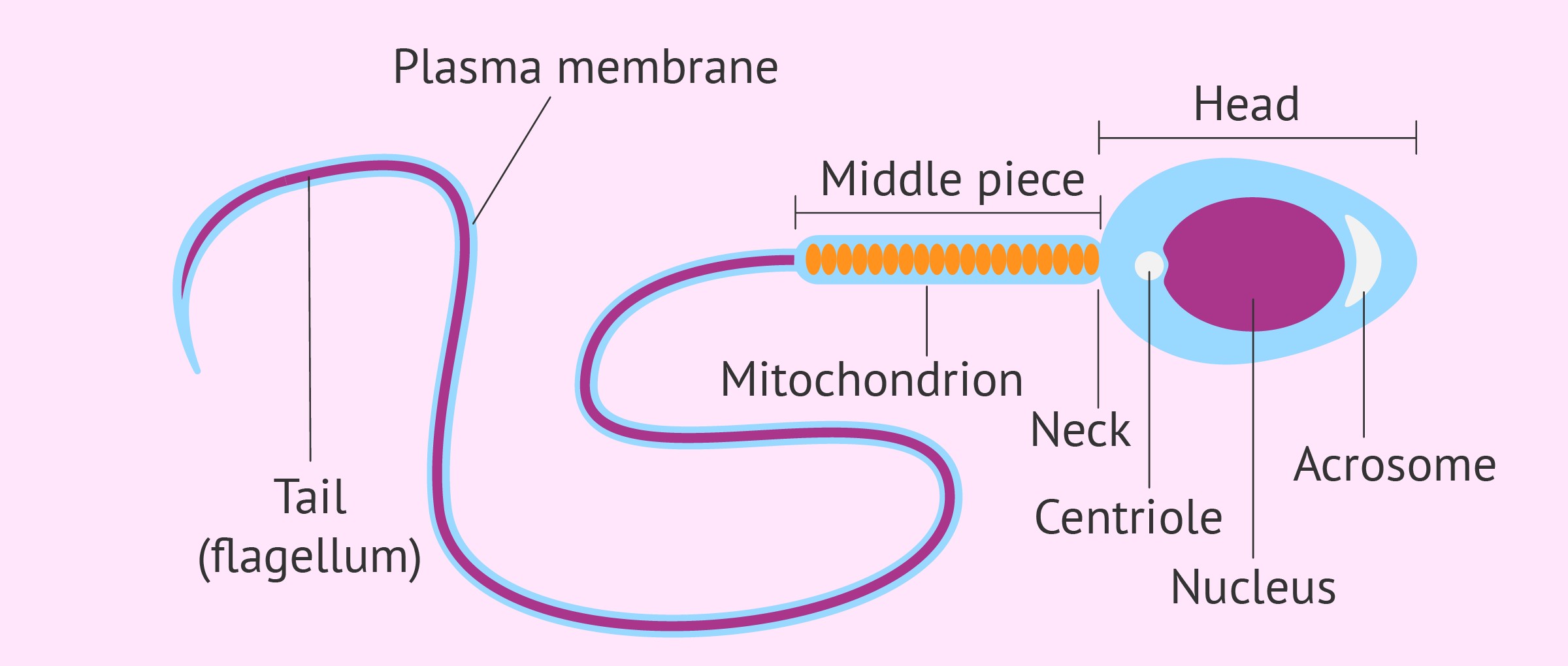
Sperm structure
Their head has a haploid nucleus, covered at the anterior end by a lysosome known as the acrosome, which contained enzymes for fertilisation.
The middle section is filled with mitochondria, which provide ATP for movement.
They spiral around microtubules, which extend from centrioles into the axial filament in the tail.
The tail, or flagellum, makes lashing movements to move the sperm.
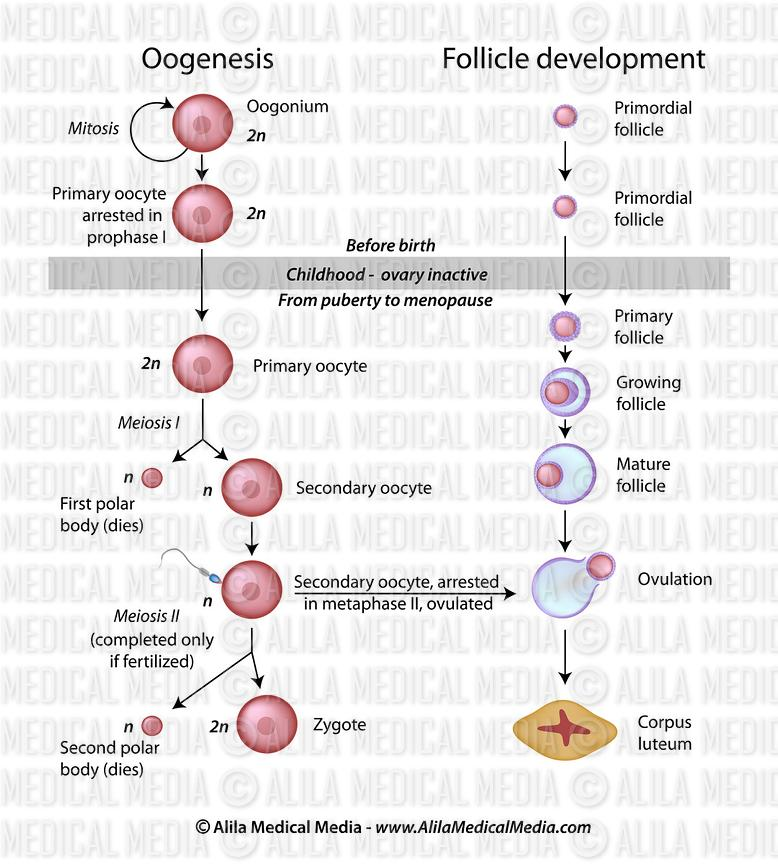
Oogenesis
Oogenesis occurs over two time periods in women:
Pre-birth:
In the developing foetus, diploid germinal epithelial cells in the ovary undergo mitosis to make diploid oogonia and more germinal epithelial cells.
These oogonia divide many times by mitosis and enlarge, making diploid primary oocytes and more oogonia.
Primary oocytes begin meiosis 1 but stop at prophase 1 - a girl is born with millions of primary oocytes at prophase 1 in her ovaries.
Germinal epithelial cells then divide to form diploid follicle cells, which surround primary oocytes to make primary follicles.
Puberty and onwards:
Hormones stimulate primary follicles to develop further.
Just before ovulation, a primary oocyte completes meiosis 1 and becomes a haploid secondary oocyte.
There is also a secondary product known as the first polar body, which is much smaller and extrodes from the end of the secondary oocyte. The secondary oocyte has most of the cytoplasm.
The primary follicle develops into a secondary follicle, called a Graafian follicle, when it is mature.
It then migrates to the surface of the ovary where it bursts and releases the secondary oocyte - a process known as ovulation.
Each month several primary follicles start to develop, but normally, only one matures into a fully developed Graafian follicle.
The secondary oocyte then begins meiosis 2, but stops at metaphase 2.
After fertilisation, meiosis 2 is completed, making an ovum containing most of the cytoplasm.
The other product is the second polar body.
After ovulation the Graafian follicle becomes the corpus luteum, AKA yellow body. If fertilisation occurs it produces hormones, otherwise it regresses.
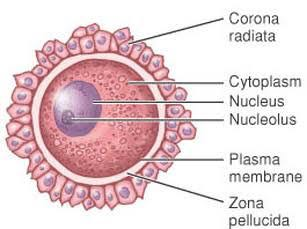
Secondary oocyte
From outside to inside:
The follicle is made up of the antrum, which is a fluid filled space. It also has an outer layer, theca cells, which are essential in fertility.
Corona radiata cells surround the secondary oocyte and provide nutrients. This is partly made up of cumulus cells.
It is surrounded by a clear glycoprotein layer known as zona pellucida which surrounds the cell membrane of the secondary oocyte.
The cytoplasm periphery has cortical granules - secondary organelles that prevent the entry of more than one sperm.
The chromosomes are at metaphase 2 - meaning they are at the equator, attached to the microtubules that make the spindle apparatus.
Sexual intercourse
Physical and psychological effects cause arterioles entering the penis and dilate, causing a build up of blood in penile spaces causing it to become erect.
It then enters the vagina, and movements cause the walls of the smooth muscle in the head of epididymis, vas deferens and penis, which causes semen to be ejaculated into the vagina.
The force is enough to propel some sperm through the cervix into the uterus, and the remainder is deposited at the top of the vagina.
Pregnancy formation
Fertilisation
Fertilisation has multiple stages and can take many hours:
Sperm attempting to reach the secondary oocyte take about five minutes after being deposited to respond to the oocyte chemoattractants and swim through the cervix, then the uterus to the oviduct.
Sperm are viable for 2-5 days, but are at their most fertile 12-24 hours after ejaculation. After ovulation, a secondary oocyte remains viable for 24 hours unless fertilised.
Millions of sperm are deposited, but only about 200 reach the secondary oocyte.
Capacitation:
Sperm undergo this in the uterus or vagina to fertilise a secondary oocyte.
Cholesterol and glycoproteins are removed from the sperm head over the acrosome.
Over several hours, the membrane becomes more fluid and permeable to calcium ions.
Acrosome reaction:
The acrosome releases proteases, which digest corona radiata cells.
Once the zona pellucida is reached the acrosome membrane ruptures and releases another protease, acrosin, is released which hydrolyses the zona pellucida.
Sperm head entry:
Cell membranes of the secondary oocyte and sperm fuse, with the sperm head sinking into the cytoplasm of the secondary oocyte.
The secondary oocyte now becomes known as an ovum.
This triggers the second meiotic division to finish, releasing the second polar body.
Cortical reaction:
When the sperm attaches to the secondary oocyte, the secondary oocyte’s smooth ER releases calcium ions into the cytoplasm.
This causes cortical granules to fuse with the cell membrane and release their enzyme contents via exocytosis.
This chemically modifies, expands and hardens the zona pellucida, making a fertilisation membrane which prevents more sperm from entering and polyspermy from occurring.
After:
Within the first 24 hours, the first mitosis combines the genetic material of the parents to make embryo diploid cells - with the sperm chromosomes joining the ovum chromosomes on the cell equator.
This is now a zygote.
Until around 10 weeks, when organs develop, it is an embryo.
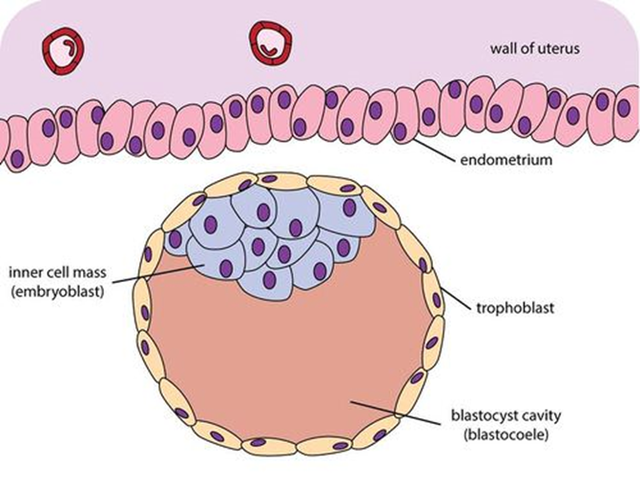
Implantation
In preparation for this process, the endometrium thickens and gets an increased blood supply to prepare it to receive an embryo. This occurs after ovulation.
There is then an implantation window between 6-10 days after ovulation.
The embryo then moves down the oviduct, dividing many times by mitosis. This occurs over days:
1-3: The embryo divides several times by mitosis, a sequence known as cleavage, which ends with the formation of the blastocyst.
At 3 days, a solid ball of 16 cells is formed known as a morula.
4-7: The embryo continues to divide by mitosis.
On day 7, the cell ball becomes hollow (the blastocoele) and is known as a blastocyst, with cells on the outside known as trophoblasts, which divide to make an inner cell mass on one side.
This moves from the oviduct into the uterus.
After around 9 - Protrusions from trophoblasts, known as trophoblastic villi penetrate the endometrium, a process known as implantation.
These increase surface area for nutrient absorption.
80% of blastocysts implant within 8-10 days.
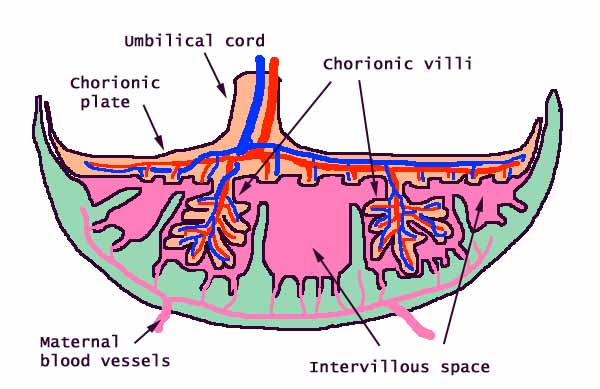
Placenta
The placenta is an organ grown by the mother during pregnancy, around 22 cm long, 2 cm thick and weighs about 500 g.
It connects the embryo and foetus to the uterine wall, and is made from tissues derived from the foetus and the mother:
The trophoblast develops into the chorion, an outer membrane which surrounds the embryo.
Cells of this chorion move into trophoblastic villi and form the much larger chorionic villi.
These form blood capillaries, which are connected to the umbilical artery and vein.
These are the blood vessels that connect the embryo to the uterus wall through the umbilical cord.
Projections from the endometrium between chorionic villi are the maternal tissues of the placenta.
It’s major roles are:
To produce hormones to support pregnancy, making it an endocrine organ. Produces human chorionic gonadotropin, oestrogen and progesterone.
Exchange of materials between the mother and foetus’ blood, such as nutrients, waste products and respiratory gases.
Chorionic villi are surrounded by intervillous spaces, known as lacunae, which contain the mother’s blood.
Chorionic villus cells have microvilli for increased diffusion with the mother’s blood, with around a 5 um distance between them for efficient facilitated diffuse, active transport, pinocytosis and osmosis. There is also a counter current flow.
It acts as physical barrier between the two circulations, in order to protect the fragile foetal capillaries from damage by the higher pressure capillaries of the mother, and from the mother’s blood pressure changes.
Provides the foetus with passive immunity, as maternal antibodies cross the placenta and attack pathogens in the foetus, but do not attack foetal cells, even though they carry the father’s antigens.
Protects the foetus from the mother’s immune system, as an immune response should be triggered due to the foreign genes from the father.
This is due to the syncytium - formed by the cells of the walls of the chorionic villi fusing so there is no space between them.
This prevents migratory immune cells from getting through the foetal blood.
This is not always complete protection:
Spontaneous abortions can be equivalent to rejections of organ transplants.
Rhesus disease in a foetus occurs when antibodies are made by a Rhesus blood negative mother (a blood type) against a rhesus positive foetus.
This gets worse for each successive Rhesus positive foetus.
Women can sometimes develop pre-eclampsia, which is abnormally high blood pressure. This can be caused by an immune response towards the placenta.
Additionally, the Rubella virus, nicotine and heroin can cross the placenta into the foetus.
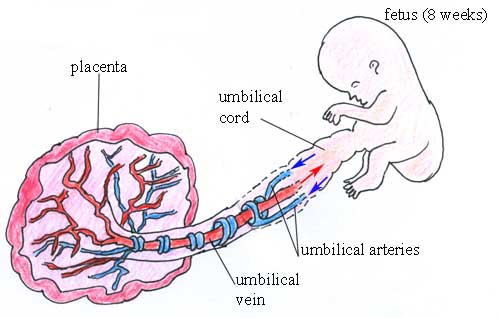
Umbilical cord
This develops from the placenta and is around 60 cm long.
It transfers blood between the foetus and the mother.
The blood of the foetus arrives at the placenta via two umbilical arteries, which both carry blood which is deoxygenated and low in nutrients.
It then exchanges materials with the mother’s blood at the chorionic villi and the blood returns to the foetus via the single umbilical vein.
Menstrual cycle
Most mammals, such as dogs, have an oestrus cycle.
This comprises of a period of sexual activity known as being ‘in heat‘.
If no embryo is replanted, the endometrium is reabsorbed and an anoestrus period follows.
Most primates have a menstrual cycle, which hormonal and physiological changes reoccurring.
This occurs monthly from the first period to menopause.
In the absence of a period, the endometrium is shed, which appears as bleeding through the vagina.
The cycle itself consists of positive and negative feedback in the brain, ovaries and uterus, with four key hormones:
Anterior pituitary hormones:
Follicle stimulating hormone (FSH).
Luteinising hormone (LH).
Ovarian hormones:
Oestrogen.
Progesterone.
It is shown as 28 days, but can vary considerably between women, and even vary between the months.
Hormone cycle
The cycle starts at day one, which is the first day of a period.
During this time, levels of all four hormones are low.
Gonadotropin (GnRH) is secreted by the hypothalamus, which stimulates the anterior pituitary gland to release FSH.
This stimulates the development of a primary follicle into a secondary follicle, or a Graafian follicle.
The follicle forms a fibrous outer layer, the theca, and secretes fluid into the antrum, a cavity. It is around 10 mm in diameter.
These thecal cells then produce oestrogen.
Oestrogen production:
Stimulates LH production in the pituitary gland via positive feedback.
Inhibits FSH secretion via negative feedback.
Triggers the rebuilding of the endometrium.
Around half way through the cycle:
LH stimulates the Graafian follicle to release the secondary oocyte via ovulation.
It also stimulates FSH, which inhibits oestrogen.
The corpus luteum formed by ovulation releases progesterone and oestrogen.
Progesterone maintains the endometrium, so implantation can occur if the secondary oocyte is fertilised. It also inhibits LH.
FSH and LH levels fall due to inhibition by oestrogen and progesterone respectively, causing the corpus luteum to degenerate.
This lowers progesterone and oestrogen, causing the endometrium to break down and shed.
This is only prevented if implantation occurs.
Around 20-70% of fertilised secondary oocytes fail to divide, implant incorrectly or simply fail to implant (the most common cause).
Pregnancy
A pregnancy is officially defined from the day of the last period until birth, even though embryonic development is only possible after ovulation.
It lasts around 39 weeks, or nine months.
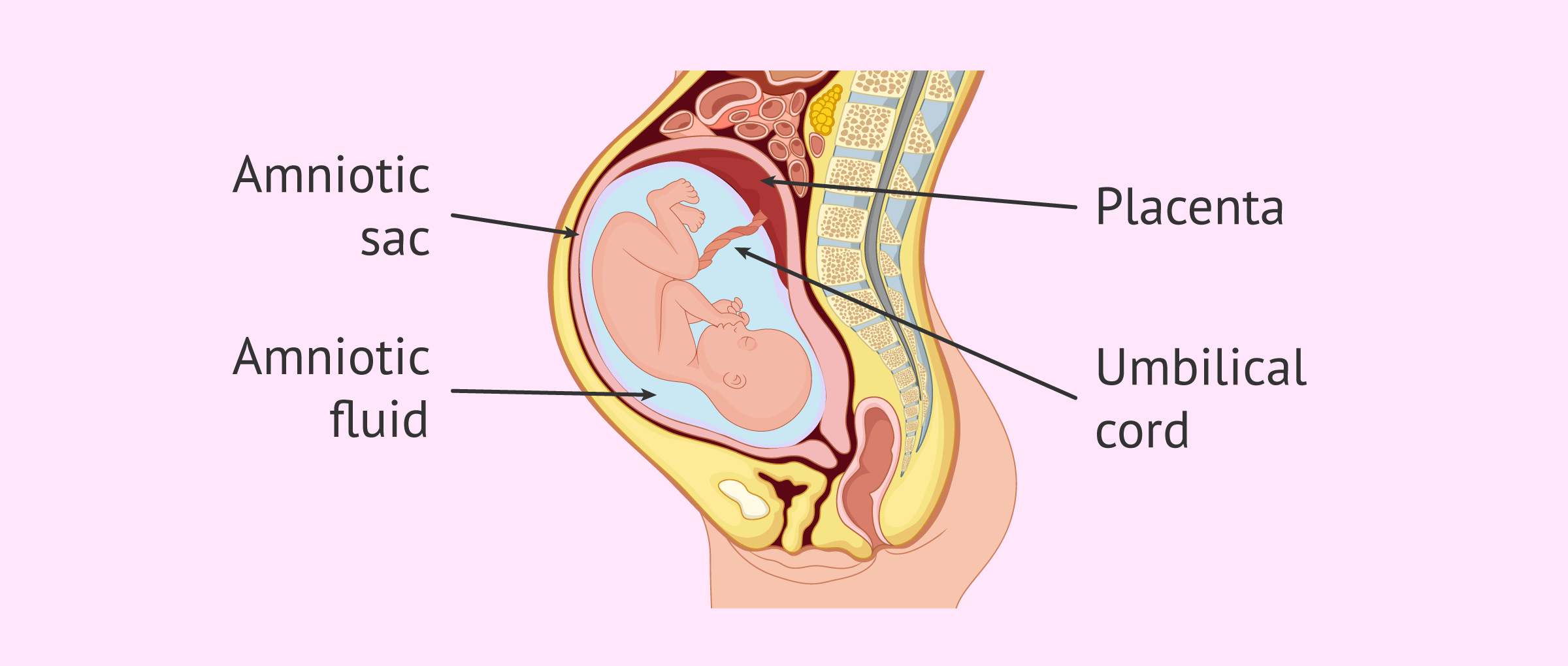
Amnion
The foetus develops and grows in the uterus and is enclosed in the amnion, a membrane derived from the inner cell mass of a blastocyst.
Initially the amnion is in contact with the embryo, but around 4-5 weeks amniotic fluid accumulates and increases in volume for 6-7 months.
It is initially made by the mother, although from 4 months the foetus contributes urine towards it.
This fluid pushes the amnion out as far as the chorion - the inner placenta layer.
Amniotic fluid is made up of 98% water, and then a solution of urea, salts, a little protein, trace amounts of sugar and some foetal cells that sloughed off the foetus.
The foetus swallows about 500 cm3 of this fluid a day, and the volume of the fluid is used to indicate that the foetus can normally swallow.
The fluid also:
Maintain foetal temperature.
Provide lubrication to prevent webbed toes and fingers, which can occur if too little amniotic fluid circulates.
Contributes to lung development.
Allows movement so muscles and bones can function before birth.
Acts as a shock absorber to protect the foetus from external injuries.
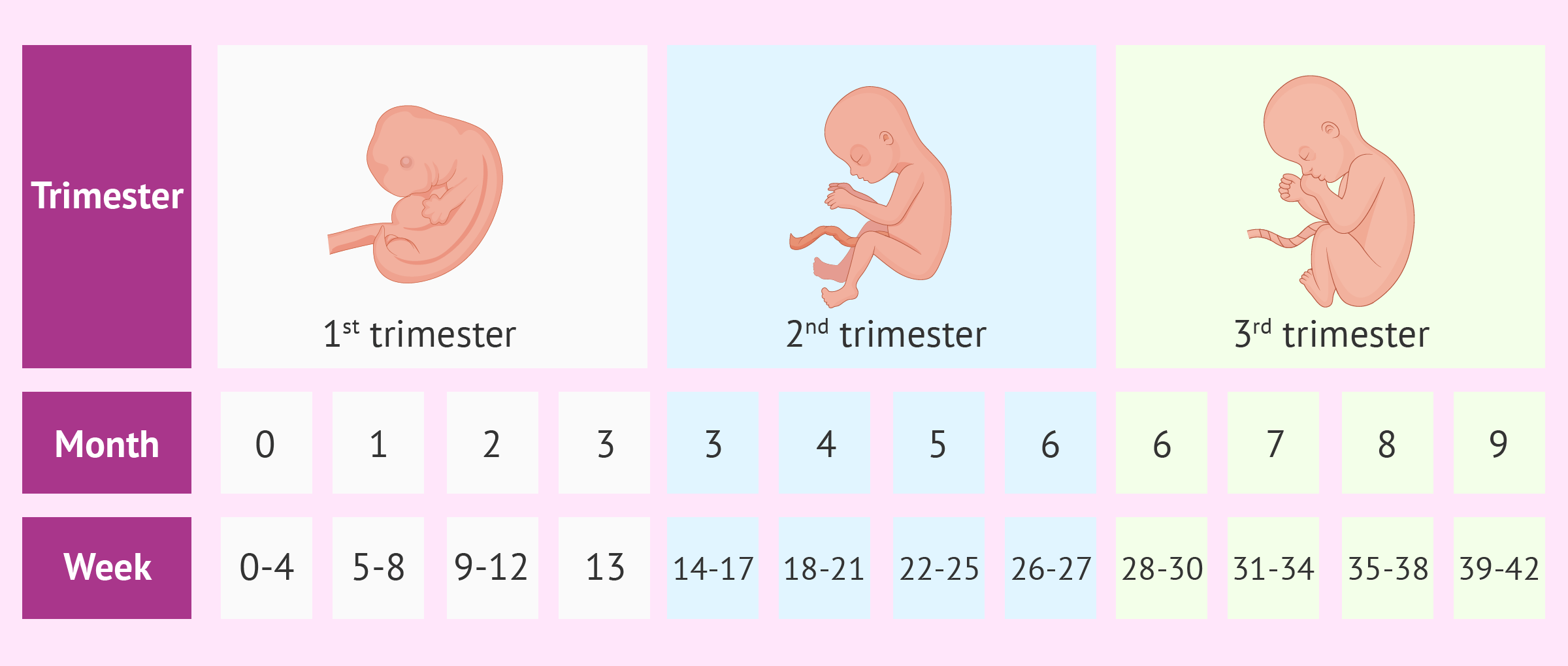
Stages
Pregnancy has three trimesters.
First:
This includes conception, implantation and embryogenesis.
All major organs are laid down.
At 22 days there is a heart beat and two brain trimester.
From weeks 5-6 there is some electrical activity in the brain, but no evidence of conscious thought.
At week 10 eyes, mouth and ears are visible and the heart can beat. The foetus will make involuntary movements.
This trimester has the highest risk of miscarriage, around 15% in those who know they are pregnant miscarry at this stage.
After week 10 it is much less prone to miscarriage, is 30 mm long and described as a foetus.
Second:
Week 18 is where some foetus’s can open their eyes.
Week 20 is where foetal movements can be felt.
Third:
All major structures are complete, and this is a period of growth.
Fat is laid down, the foetus’ mass is tripled and the length doubles.
At 28 weeks, more than 90% of premature babies survive.
There is evidence that senses, such as hearing, develop.
At 33 weeks, the foetus spend 90% of it’s time asleep while it lays down millions of neurons each minute.
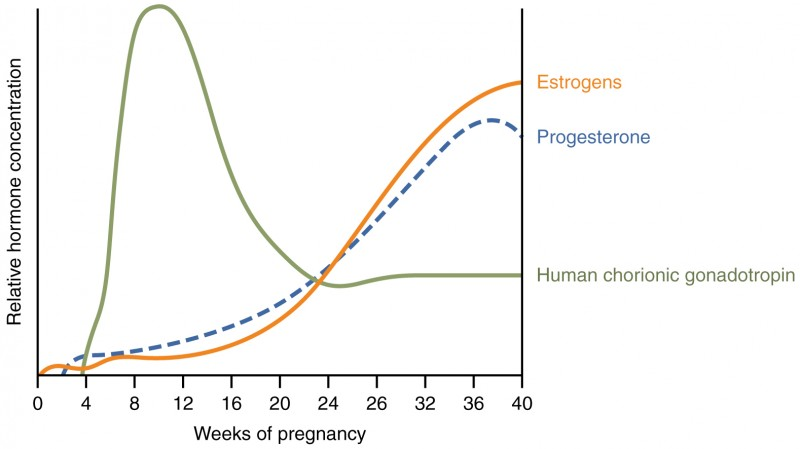
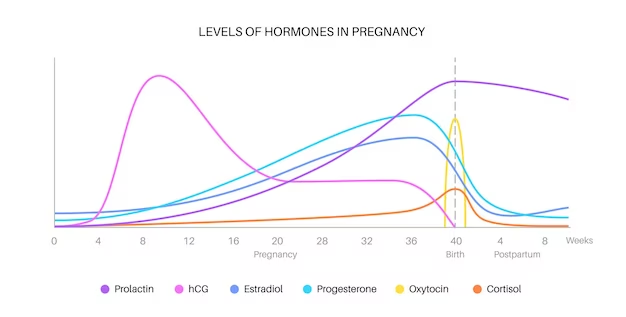
Placental hormones
Human chorionic gonadotropin (hCG) is secreted from the blastocyst, around 6 days after fertilisation.
It is made by the chorion, which makes up the inner layers of the placenta.
It is a glycoprotein and maintains the corpus luteum for progesterone secretions for the first 16 weeks of pregnancy.
This is because progesterone maintains the endometrium, which is necessary for embryonic development as it is necessary for the development of the placenta.
Oestrogen - Secreted from the corpus luteum, and then the placenta until the end of pregnancy. It:
Inhibits FSH to prevent follicles maturing.
Prolactin, to prevent milk production.
Stimulates the growth of the uterus to fit the foetus.
Stimulates mammary gland growth and increases their blood supply, especially in the third trimester.
Progesterone - Secreted from the corpus luteum, and then the placenta until the end of pregnancy. It:
Inhibits LH, so ovulation cannot occur.
Inhibits prolactin, to prevent milk production.
Inhibits oxytocin, to prevent myometrium and milk duct muscles from contracting.
Birth
It is in the mother’s best interest to give birth as soon as possible, and in the foetus’ to stay as long as possible.
They release conflicting hormones, until at 39 weeks when the mother’s prevail.
In the last 3 months of pregnancy, oestrogen increases by more than progesterone. Just prior to birth, progesterone concentration in the plasma declines.
This is due to foetal hormones in the mother’s bloodstream decreasing progesterone concentrations in the plasma.
The high concentrations of oestrogen and progesterone inhibited prolactin and oxytocin, and once produced:
Oxytocin - Released in the posterior pituitary gland, and causes myometrial contractions.
These begin mild, but these contractions stimulate more oxytocin via positive feedback. They therefore become stronger and more frequent.
They occur from the top down to allow the foetus to be pushed through the cervix.
Prolactin - Released in the anterior pituitary gland, and stimulates glandular tissue in the mammary glands to synthesise milk.
It is released when oxytocin causes the muscles around the milk duct to contract.
The secretion of this hormone continues after birth, for as long as milk is needed.
Male hormones
FSH is used in sperm development.
LH stimulates Leydig cells.
Testosterone is released in Leydig cells, and supports sperm development and secondary sexual characteristics.