32. DMD Epidemiology 2025
Epidemiology of Infection
Objectives of the Lecture
Understand the concept of epidemiology of infections and the roles of:
Inoculum
Virulence
Host resistance
Describe the transmission of viruses and bacteria.
Discuss the seasonality of common infections.
Analyze patterns of bacterial and viral infections including terms such as:
Acute
Self-limiting
Latent
Reactivation
Chronic
Commensal
Opportunistic
Overview of the epidemiology of herpes viruses:
Herpes Simplex
Varicella virus
Cytomegalovirus (CMV)
Epstein-Barr Virus (EBV)
Define:
Virulence of microbes
Endemic and epidemic infections
Prevalence and incidence
Briefly describe the standard approach to outbreak investigation.
Fundamental Concepts of Epidemiology
Definition
Epidemiology is the study of the occurrence, determinants, distribution, and control of disease in populations.
5W
Infection risk is influenced by:
Individual susceptibility
Level of disease in the population
Herd immunity
Communicable period
Infectiousness
Patterns of Distribution in Epidemiology
Distribution can be analyzed by:
Age
Gender
Occupation/Hobby
Nutritional status
Season
Geography
Living conditions/Social behavior
Disease Metrics
Prevalence vs. Incidence
Prevalence: Cases per unit population at a given time. total compare to now
Incidence: Number of new cases per unit population.
Example: Acute self-limiting infections like influenza have high incidence (in winter) but low prevalence, whereas chronic infections like hepatitis B have high prevalence with low incidence (now have vaccination).
Factors Influencing Infection Risk
Key Influencers
Factors determining likelihood of infection include:
Inoculum (dose) - number organism
Virulence - ability to cause disease
Host resistance
Generally, a high dose coupled with high virulence and low host resistance increases the likelihood of disease.
Sources of Infection
Exogenous Infections
An exogenous infection is an infection caused by a microorganism from outside the body, such as the environment or another person
Most common sources are:
Human-to-Human
Zoonotic (from animals to humans)
Rarely from the environment.
Endogenous Infections
Infections arising from normal flora, including:
E. coli in gut → causing urinary tract infections
Oral streptococci → causing endocarditis
Staph aureus from the nose → causing wound infections.
Mixed oral flora including anaerobes → dental abscess
Commensals
(Commensal bacteria are microorganisms that live on the body's surfaces without causing harm. They are also known as normal microflora)
Many bacteria serve as normal flora and may protect against infection.
In certain conditions, commensals can become opportunistic pathogens/ endogenous infection leading to clinical infections such as:
Mucosal damage
Reduced immunity due to disease.
Opportunistic Infections by commensals
Infections that take hold due to reduced host immunity, often occurring in patients with:
Chemotherapy
Transplantation
Diseases like AIDS.
Examples include:
CMV causing systemic infections in transplant patients
EBV causing oral hairy leukoplakia in AIDS patients.
Transmission of Infections
Types - vertical and horizontal
Vertical Transmission: Mother to baby, routes include:
In utero (e.g., syphilis)
At birth (e.g., HIV)
Post-birth (e.g., HTLV).
Horizontal Transmission
Direct Transmission: Through activities like kissing, touching, or sexual contact.
Airborne: Inhalation of droplets from an infected individual (e.g., influenza).
Fomite: Contact with infected surfaces or instruments (e.g., dental equipment).
Vector-borne: Transmission via arthropods such as ticks or mosquitoes (e.g., Lyme disease, malaria).
Infectious Parameters
Definitions
Incubation Period: Time from inoculation (exposure to the infectious agent) to symptom onset.
Influenza has a short incubation period (1-4 days), while diseases like HIV can have much longer incubation periods.
Infectious Period: Time during which an infected person can spread the infection.
This may start before symptoms appear and last even after symptoms resolve, depending on the disease.
Systematic period The duration during which the infected individual experiences symptoms
infectiousness A measure of how easily a disease spreads from an infected individual to others. This depends on factors like the mode of transmission (e.g., airborne, droplet, contact), the dose required to establish infection, and host factors (e.g., immunity).
Case Study - Chickenpox
Timeline of infection stages:
Inoculation to shedding (day 13
Shedding to symptom onset (day 15)
Later reactivation can occur as shingles (zoster).
Infection Patterns
Categories
Acute-Self Limiting: E.g., Influenza.
Chronic: E.g., HBV, HCV, HIV, TB
Latent with Reactivation: E.g., Herpes viruses, VZV, TB.
General Infection Dynamics
Various outcomes from an acute infection can lead to:
acute infection →Viral clearance
acute infection →Chronic infection.
acute infection → Latency followed by reactivation
Herpes Virus Epidemiology
ALL HERPES VIRUS HAVE LATENCY
Varicella-Zoster Virus (VZV)
Initially causes chickenpox, followed by latency by sensory ganglion and potential reactivation as shingles.
95% of adults are seropositive for VZV.
Approximately 40% experience shingles.
Herpes Simplex Virus (HSV)
Initially causes gingivostomatitis , followed by latency by trigenminal ganglion and potential reactivation as cold sore (herpes labialis)
85% of adults are seropositive.
~20% develop recurrent cold sores.
Cytomegalovirus (CMV)
Infection incidence is ~1% annually; 20% of young adults seropositive.
Transmission through salivary contact, usually asymptomatic except in pregnancy or immunosuppression.
retinitis, pneumonia, encephalitis
incurabe - Life long infection - shed in saliva
Epstein-Barr Virus (EBV)
Salivary transmission; most people are IgG positive by age 25.
Can cause infectious mononucleosis (glandular fever) in teenager, viral meningitis, nasopharyngeal cancer, often asymptomatic in children.
Dynamics of Diseases
Outbreak Classifications
Endemic Infections: Stable incidence within a population.
Outbreaks: Clusters of cases or increases in incidence.
Epidemic: Increased incidence over a larger region.
Pandemic: Spread across multiple continents.
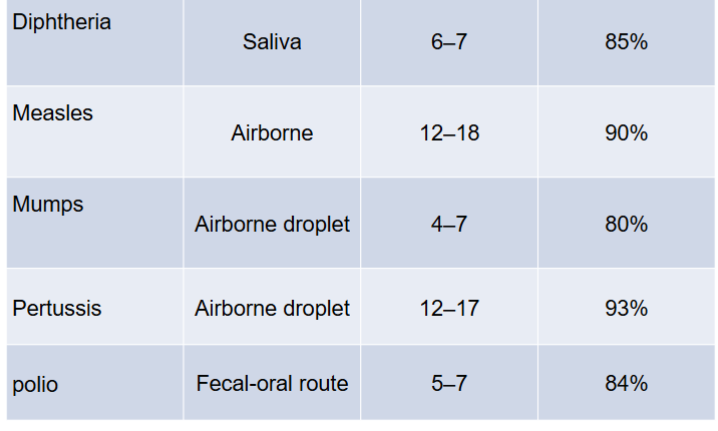
Reproductive Rate (Ro) and R
R₀ – Basic Reproduction Number
It’s the average number of people that one sick person will infect in a completely susceptible population (meaning no one has immunity — no vaccine, no prior infection).
It shows how contagious a disease is in ideal conditions.
Examples:
Measles has a high R₀ (~12–18): super contagious.
COVID-19 (original strain) had an R₀ around 2–3.
R – Effective Reproductive Number
This is the actual number of people one sick person infects in real-world conditions (where some people are vaccinated, recovered, or immune).
So R can be less than R₀ if immunity or control measures (like masks, distancing, etc.) are in place.
Key point:
If R > 1 → the disease is spreading.(epidemic)
R=1 endemic - disease is stable
If R < 1 → the outbreak is shrinking, reduce transmission
Term
Meaning
Conditions
R₀
How contagious a disease is without any immunity or control
Idealized situation (no protection)
R
How contagious a disease is right now in the real world
Includes effects of immunity, measures
Sentinel GP Consultation Data
Trends
Consultation rates for flu-like illnesses are tracked from 2010 to 2013, showing fluctuations over the weeks each year.
allow hospital to prepare and plan
Herd Immunity
Concept
Resistance of a population to the spread of an infectious agent based on a high proportion of immune individuals.
Critical for discussions on vaccine effectiveness and strategies.
Disease transmission R0 Herd immunity threshold
Seasonality of Infections
General Patterns
Compare
UTI incidence remains stable throughout the year.
Higher respiratory infections in winter.
Example of seasonal variations:
Summer: faeco oral infection , Enteroviruses, Hepatitis A. Barbecue weather?
Winter: respiratory infection , Influenza.
Spring: Varicella (chicken pox)
Reason for seasonality may include:
Environmental factors (humidity UV) affecting survival of pathogens.
Indoor crowding effects.
weather related mucosal change
Vectors - survival in different weather
Outbreak Control Steps
Procedures
Determine if an outbreak is occurring.
Form an Outbreak Control Team (OCT) if necessary.
Develop case definitions for identification.
Collect and analyze data to create epidemic curves.
Conduct analytical studies of the outbreak.
Implement control measures to mitigate the outbreak such as:
Removing the source of infection.
Protecting at-risk individuals.
7. come up plans to prevent recurrence
Tools for Infection Control
Management Strategies
Infection control strategies include:
Preventing direct transmission for infection control
Treatment or prophylaxis with antimicrobials.
Utilizing vaccines for prevention.
Applying immunoglobulin where necessary.
Conducting environmental cleaning.