topic 9
Topic 9: Muscle Fatigue (Comparability model)
Fatigue = inability to generate required or expected force (maximal or submaximal)
2 general categories of fatigue: Central (nervous system) & Peripheral (muscle tissue)
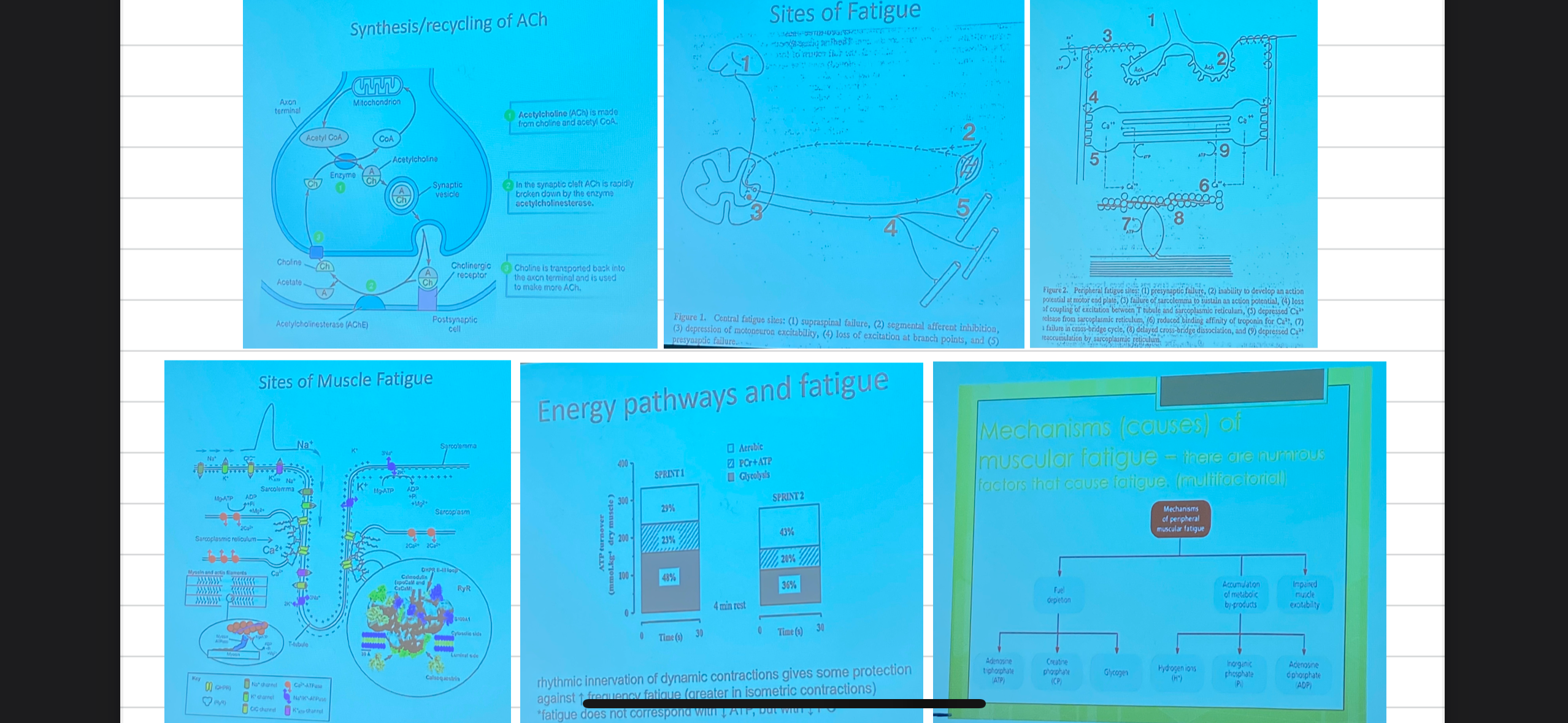
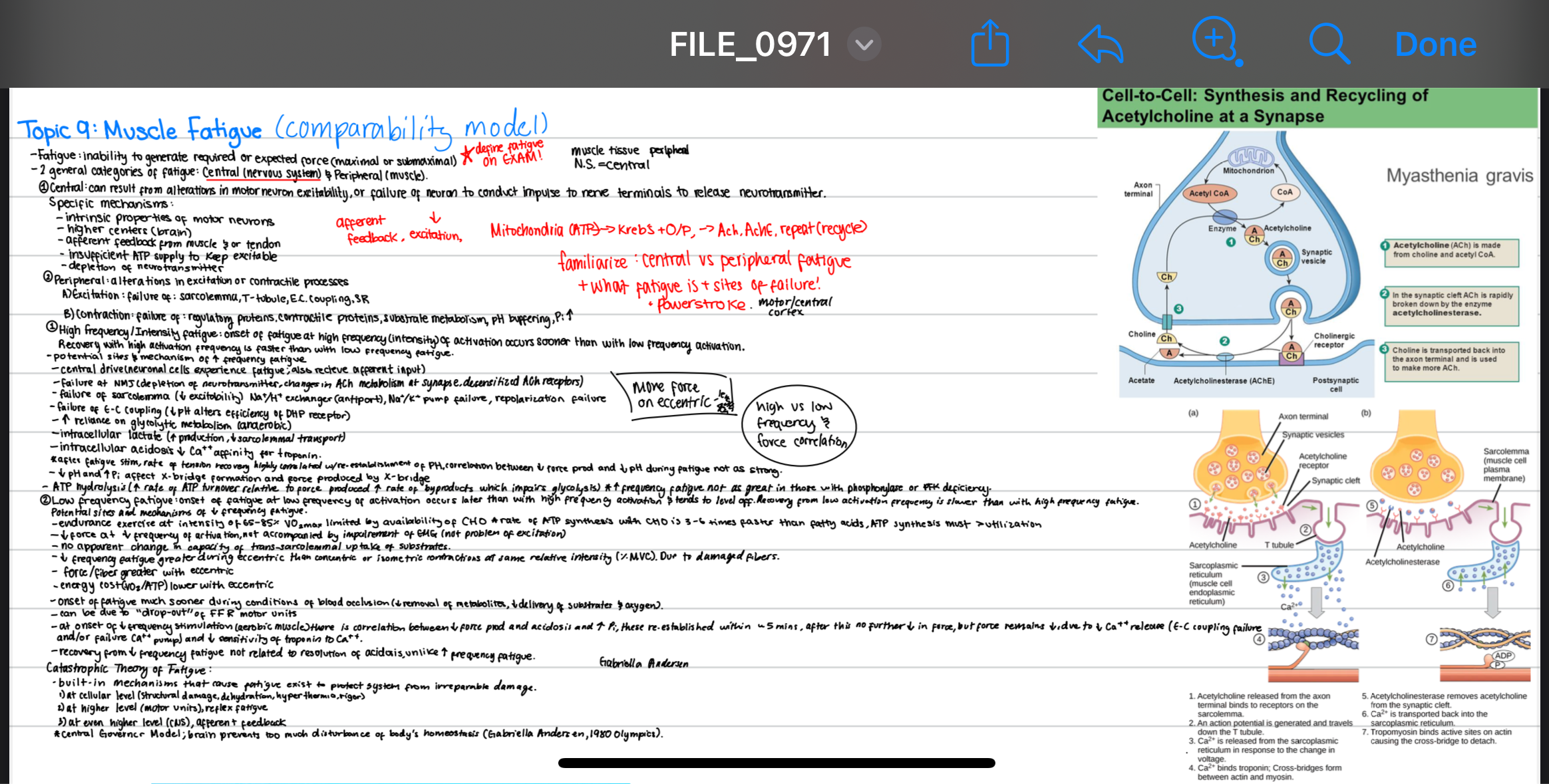
1) Central: can result from alterations in motor neuron excitability, or failure of neuron to conduct impulse to nerve terminals to release neurotransmitter.
intrinsic properties of motor neurons
higher centers (brain)
afferent feedback from muscle or tendon
insufficient ATP supply to keep excitability
depletion of neurotransmitter
^^^^^NERVOUS SYSTEM
2) Peripheral: alteration in excitation or contractile processes
→ Excitation: failure at sarcolemma, T-tubule, E-C coupling, SR
→Contraction: failure of regulatory proteins, contractile proteins, substrate metabolism, pH buffering, Pi inc.
^^^^^^IN THE MUSCLE ITSELF
think sprinting
1) High frequency/intensity fatigue: onset of fatigue during high frequency (intensity) activation occurs sooner than with low frequency activation.
Recovery with high stimulation frequency is faster than with low stimulation frequency.
Potentials sites & mechanism:
Central drive (neuronal cells experience fatigue, also receive afferent input)
brain or spinal cord is not sending as strong or as frequent signals to muscles.
afferent feedback from muscles also affects central drive and may contribute to fatigue.
Failure at NMJ (depletion of neurotransmitter, changes in Ach metabolism at synapse, desensitization of Ach receptors)
Failure of sarcolemma (↓ excitability) Na⁺/H⁺ exchanger (antiport), Na⁺/K⁺ pump failure, repolarization failure
Failure of E-C coupling (↓ pH alters efficiency by DHP receptor)
(DHP) receptor, which is essential for releasing calcium from the sarcoplasmic reticulum into the muscle
increased reliance on glycolytic metabolism (anaerobic)
leads to the production of lactate (which can further contribute to fatigue).
Intracellular lactate (inc lactate production, dec sarcolemmal transport)
Decreased sarcolemmal lactate transport means that lactate accumulates in the muscle, which exacerbates fatigue.
Intracellular acidosis decrease Ca²⁺ affinity for troponin
impairs cross-bridge formation
POST FATIGUE
after fatigue stimulation, rate of tension recovery highly correlated with reestablishent of PH
correlation between decrease force production and dec pH during fatigue not as strong
low pH and high Pi affect x-bridge formation & force produced
ATP hydrolysis (inc. rate of ATP turnover relative to force produced increases rate of byproducts which impairs glycolysis)
high frequency fatigue not as great in those with phosphorylase or PFK deficiency
they are less reliant on glycolysis
think marathon
2) Low frequency fatigue: onset of fatigue slower at lower frequency of activation occurs later than with high frequency activation &tends to level off. recovery slower than with high frequency fatigue
Potential sites and mechanisms:
endurance exercise at intensity of ~60-85% VO₂max limited by availability of CHO
rate of ATP synthesis with CHO is 3 – 6x faster than fatty acids,
ATP synthesis must > utilization.
↓ Force at low frequency of activation, not accompanied by impairment of EMG (not problem of excitation)
no apparent change in capacity of trans-sarcolemmal uptake of substrates
low frequency fatigue greater during eccentric than concentric or isometric contractions at same relative intensity (%MVC) due to more damaged fibers
because force/ fiber greater with eccentric
energy cost (Vo2/atp) lower with eccentric
onset of fatigue much sooner during conditions of blood occlusions (↓ removal of metabolites, ↓ delivery of substrates & oxygen)
LFF can be due to “drop out” of FFR motor units
at onset of low frequency stimulation (aerobic muscle) there is correlation between ↓ force production and acidosis and increase pi
these reestablished within ~5 min, after this no further ↓ in force but force remains low
due to ↓ ca release from SR (EC coupling) and/or failure ca pump and ↓ sensitivity of troponin to Ca
recovery from low frequency fatigue not related to resolution of acidosis, unlike high frequency fatigue - does not recover even after pH recovers
Catastrophic Theory of Fatigue:
built on mechanisms that cause fatigue exist to protect system from irreparable damage
at cellular level (structural damage, dehydration, hyperthermia(excess heat), rigor (stiff due to lack of atp)
at higher level (motor units) reflex fatigue - prevents further stress
at even higher level (CNS) afferent feedback
**central governor model: brain prevents too much disturbance of body’s homeostasis