Special Senses - The Sensory Organs
5 Senses - Part of the PNS, and send information back to the brain for processing about what to do next
Sight - Visual System
Eyes and Optic Nerves (transmit info to the occipital lobe)
Hearing - Auditory System
Ears and auditory nerves (sends signals to the temporal lobe)
Touch - Somatosensory System
Specialized receptor cells, primarily in the skin that respond to different tactile stimuli and send info to the sensory cortex in the parietal lobe
Smell - Olfactory System
Begins with nerves in the nasal passages that analyze scents and passes info to the amygdala and hippocampus
Taste - Gustatory System
Taste buds on the tongue, sends input along the facial nerve to the primary gustatory cortex
The Organ of Sight - The Eye
Ambyl/o- | Dim, dullness |
Blephar/o- | Eyelid |
Conjunctiv/o- | Conjunctiva |
Cor/o- | Pupil |
Cycl/o- | Ciliary Body |
Dacry/o- | Tear |
Glauc/o- | Gray |
Irid/o- | Iris |
Lacrim/o- | Tear |
Mi/o- | Smaller |
Ocul/o- | Eye |
Ophthalm/o- | Eye |
Palpebr/o- | Eyelid |
Papill/o- | Optic Nerve |
Phac/o- | Lends of the eye |
Presby/o- | Old Age |
Retin/o- | Retina |
Scler/o- | Sclera |
Scot/o- | Darkness |
Uve/o- | Uvea |
Vitre/o- | Glassy |
-opia | Vision |
-tropia | To Turn |
Terms Related to Sight:
Ambylopia - Lazy eye, causing vision dullness
Ametropia - Eye refractive power defect
Aphakia - Absence of lens of the eye
Astigmatism - Abnormal curve of the cornea, causing light entering the eye to not focus on the retina and making vision out-of-focus
Blepharitis - Inflammation of edges of eyelid
Cataract - Opacity in or on the lens
Chalazion - Granuloma around a Subaceaous gland on the eyelid
Conjunctivitis - Inflammation of mucous membrane covering the eye and inside of eyelids
Cycloplegia - Paralysis of ciliary muscle
Dacryocystitis - Inflammation and obstruction of nasolacrimal duct
Dacryostenosis - Narrowing of the lacrimal duct
Diplopia - Double Vision
Ectropian - Eyelid eversion (turning outward)
Entropian - Eyelid inversion (turning inward)
Enucleation - Removal of an organ from a body cavity
Episclera - Connective covering of the sclera
Exenteration - Radical excision; removal of an organ in one-piece
Exophthalmos - Anterior protrusion of the eyeball out of the orbit
Glaucoma - Increased intraocular pressure
Hordeolum - Infection of a sebaceous gland on the eyelid, stye
Hypertropia -Farsightedness
Keratomalacia - Softening of the cornea due to Vitamin A deficiency
Keratitis - Inflammation of the cornea
Myopia - Nearsightedness
Nystagmus - Rapid, involuntary eye movements, usually caused by a brain tumor, inner ear condition, or adverse reaction to medication
Ophthalmologist - Physician who specializes in the diagnosis and treatment of diseases of the eye
Ophthalmoscope - Instrument used to examine interior portion of the eye
Papilledema - Swelling of the optic disk
Presbyopia - Farsightedness due to aging and progressive disease
Ptosis - Drooping of the upper eyelid
Retinopathy - Non-inflammatory, degenerative disease of the retina
Strabismus - Extraocular muscle deviation which causes unequal visual axis, also called being cross-eyed
Tarsorrhaphy - Suturing of eyelids together
Tonometer - Instrument measuring intraocular pressure
Trichiasis - Ingrown eyelashes; they can rub against the cornea, causing irritation
Uveal - Vascular tissue of choroid, ciliary body, and iris
Xanthelasma - Lipid disorder, yellow plaque on the eyelid
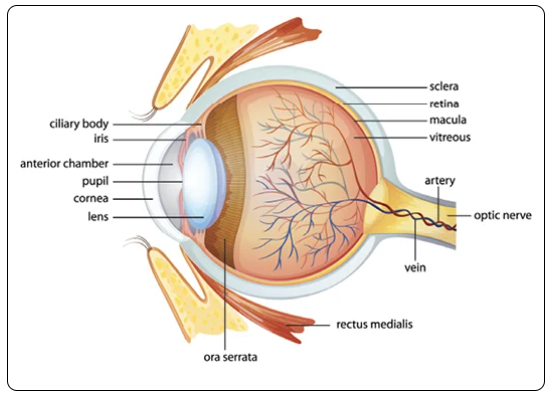
Eye Anatomy -
Eye sits in the orbital socket of the skull
Conjunctiva - Outermost layer of the eye, a clear membrane covering the front of the eye and inside surface of the eyelids
Sclera - the white, opaque, protective outer layer and provides a surface for the extrinsic muscles to attach to
Cornea - clear area of the sclera that allows light to pass through into the anterior chamber; the space filled with aqueous humor between the cornea and the lens.
Has 5 layers of flat cells
Touch and pain receptors
Only part of the body that is avascular (no blood vessels)
Choroid - Beneath the sclera. Middle layer. Vascular structure of the eye, providing blood and oxygen
Pupil - In front of the choroid. An opening that allows light to enter into the inner eye from the anterior chamber
Iris - Colored ring of muscles that contracts or dilates according to how much or how little light is present
During stressful situations, the sympathetic nervous system will cause pupils to dilate
Lens - Behind the pupil. Crystalline disc is biconvex (convex on both sides) and focuses the light coming in through the pupil onto the retina
Anterior side of the lens is slightly less curves than the posterior
Supersensory Ligaments - connect the lens to the ciliary muscles. Change the shape of the lens when the eye focuses on the nearby object
Posterior Chamber - The space behind the lens and is filled with vitreous humor
Vitreous Humor - Thick, gel-like substance that maintains the shape of the eye and aids in focusing light onto the retina
Retina - Inner most layer at the back of the eye. Has 2 types of photoreceptors:
Rods - sensitive to low light, do not detect color, contribute to peripheral vision
Cones - Respond to bright light and color.
Optic Disc - Around the spot where the optic nerve meets the retina. No rods or cones, considered the "blind spot" of the eye
Optic Nerve - Receives signals from the retina and transmits them to the occipital lobe of the brain
Aqueous Humor:
Location: This is a clear, watery fluid found in the anterior chamber of the eye, between the cornea and the lens.
Function: It helps maintain intraocular pressure, provides nutrients to the lens and cornea, and removes waste products. The aqueous humor is continuously produced and drained, keeping the eye's internal environment stable.
Vitreous Humor:
Location: This is a clear, gel-like substance that fills the vitreous cavity, which is the space between the lens and the retina.
Function: It helps maintain the shape of the eyeball, supports the retina in place, and acts as a shock absorber to protect the eye from injury. Unlike the aqueous humor, the vitreous humor is not continuously produced and typically remains the same throughout a person’s life.
Eye Pathologies:
Glaucoma - Increased intraocular pressure with multiple etiologies.
Can be caused by excess accumulation of aqueous humor in the anterior chamber, hypertension, edema, obesity, or decreased blood flow to the eye
Genetic Heredity could play a role
Open Angle Glaucoma - Most common type. The Trabecular Meshwork, the spongy tissue by the cornea with allows aqueous humor to drain out of the eye, doesn't drain properly. Causing buildup of fluid in the anterior chamber
Chronic & slower onset
Can be asymptomatic until loss of Visual Field is apparent
Closed Angle Glaucoma - When the iris is squeezed against the cornea, narrowing or blocking the drainage of aqueous humor.
Acute and painful - headaches, eye pain, visual halos
If left untreated, can damage the retina and optic nerve and eventually result in "tunnel vision" - where the patient has lost their peripheral field of sight
Treatment:
Iridectomy - create an opening for the aqueous humor to flow out of the eye.
Prescriptions:
Pilocarpine can open the angel of the anterior chamber of the eye (closed angle) or contract the ciliary muscles to increase outflow of the aqueous humor (open angle).
Prostaglandins (travoprost, latanoprost, bimatoprost) can encourage fluid drainage to decrease intraocular pressure
Beta blockers (betaxolol & timolol) reduce the amount of aqueous humor the eye produces
Cataracts - Cloudiness or opacity of the lens. Causes hazy or blurry vision.
Caused by:
Aging, from the breakdown of proteins and fibers in the lens itself.
Can be congenital with bilateral opacity present at birth.
Heat-induced cataracts due to exposure to radiation
Traumatic cataracts are result of injury to the eye
Senile Cataracts - age related, usually on the interior lens
Type of cataract is classed by morphology: size, shape, site, and etiology
Treatment:
New prescription eyeglasses
Anti-flare sunglasses
Use of magnifying lenses
Surgery (when vision is too impaired)
Phacoemulsification - Most common type of surgery. A tiny incision is made in the eye, and an ultrasonic device vibrating at a high frequency is inserted. Softening and breaking the lens up into smaller pieces, that are then suctioned out
Extracapsular - surgery consists of an incision made into the eye so the nucleus of the lens can be removed all in one place. The posterior half of the lens' outer cover is left in place.
Intracapsular - rarely performed. Reserved for advanced cataract development or trauma, since the entire lens and its capsule are removed through one larger incision
Macular Degeneration - the destruction of the fovea centralis, the small depression in the retina where visual acuity is highest.
Caused by: Age, UV exposure, drugs, or heredity
As the disease progresses, the central field of vision is lost
Wet Macular Degeneration - caused by new vascularization and blood or fluid leaking into the macula.
Treatment - Photocoagulation therapy using a laser to seal the blood vessels and stop them from leaking
Dry Macular Degeneration - the atrophy and deterioration of the macula. No known treatment.
Retinal Detachment - When the layers of the retina separate from one another. Vitreous humor leaks behind the retina, causing the retina to pull away from the choroid, resulting in a blind spot
If pressure continues, patient will go blind
Cause: age, eye injury, diabetic retinopathy, or macular degeneration
Symptoms: sudden appearance of floaters, seeing "static" or snow, sudden flashes of light, or a shadow in the field of vision
Treatment - Surgery is needed quickly to save vision
Photocoagulation - Laser surgical procedure used for minor cases. The eye is numbed, laser focused on the site of the tear, burning the area around the tear and causing a scar. Scar prevents further detachment.
Pneumatic Retinopexy - Treat medium to large tears. A gas bubble is injected into the eye and exerts pressure on the tear. Retina is pushed back towards its proper place in the eye. Surgeon uses a freezing device to seal the retina back against the choroid
Scleral Buckle - treat large tears. Once the surgeon has reattached the retina, a band of silicone is stitched around the circumference of the sclera. Decreases eye circumference and helps hold the retina in place
The Organ of Hearing - The Ear
Adit/o- | Hearing |
Audi/o- | Hearing |
Aur/o- | Ear |
Auricul/o | Ear |
Cochle/o | Cochlea |
Myring/o- | Tympanic Membrane |
Ossicul/o- | Ossicle |
Ot/o- | Ear |
Salping/o- | Eustachian Tube |
Staped/o- | Stapes |
Tympan/o- | Tympanic Membrane |
Vestibul/o- | Vestibule |
-acusis | Hearing |
-meter | Instrument to measure |
-otia | Ear Condition |
Hearing Medical Terms
Audiology - Study of hearing disorders
Apicectomy - Excision of portion of temporal bone
Aural Atresia - Congenital absence of external auditory canal
Cerumen - Earwax
Cholesteatoma - Abnormal, noncancerous growth that forms in the middle ear
Cochlear Implant - Electronic device implanted in the cochlea that stimulates the auditory nerve to provide hearing sensations
Exostosis - Bony overgrowth in the ear canal
Fenestration - creation of a new opening in the middle ear's inner wall
Labyrinthitis - Inflammation of labyrinth
Macrotia - Condition of having abnormally large ears
Myringoplasty - Surgical repair of tympanic membrane
Myringotomy/Tympanotomy - Surgical incision into the eardrum to allow for drainage
Ossicles - 3 small bones in middle ear (malleus, incus, stapes)
Otalgia - Ear pain
Otorhinolaryngologist - Ear, nose, and throat specialist
Otologist - Physician who specializes in diseases and treatment of the ear
Otopyorrhea - Pus drainage from the ear
Otosclerosis - Abnormal bone growth inside the ear
Otoscope - Instrument used to examine the eardrum and ear
Serous Otitis Media - Noninfectious inflammation of the middle ear; accumulation of serous fluid due to dysfunctional or obstructed Eustachian tube(s)
Stapedectomy - Removal of the stapes and replacement with a prosthesis, performed to correct hearing loss due to otosclerosis
Tinnitus - Ringing of the ear
Tympanolysis - Freeing of tympanic membrane adhesions
Tympanostomy Tube Placement - Placement of tube in the tympanic membrane to relieve fluid build up
Vertigo - Feeling of dizziness or the room spinning, caused by disturbance of equilibrium in the labyrinth
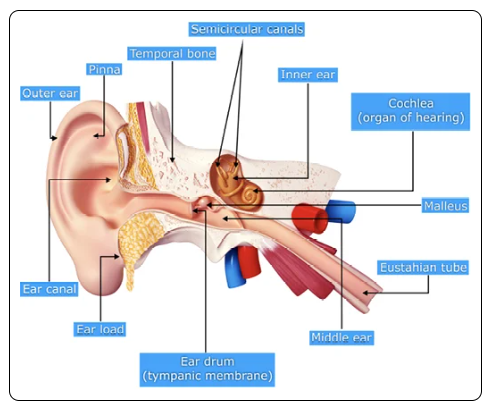
Ear Anatomy & Physiology - Ear is divided into 3 sections:
Outer Ear: This includes the pinna (or auricle) and the ear canal. The pinna captures sound waves and directs them into the ear canal toward the eardrum.
Middle Ear: This section contains the eardrum (tympanic membrane) and three tiny bones called ossicles (malleus, incus, and stapes). These bones amplify and transmit sound vibrations from the eardrum to the inner ear.
Inner Ear: This part consists of the cochlea (which converts sound vibrations into nerve signals) and the vestibular system (which helps with balance). The cochlea sends the auditory signals to the brain via the auditory nerve.
External Auditory Canal - The outer ear.
The auricle or pinna (ear lobe), collects sound and focuses it into the auditory canal
Where cerumen is produced and connects the outer ear to the tympanic membrane
Tympanic Membrane (Eardrum) - Middle Ear
Transmits vibrations from the auditory canal to the middle ear
3 layers: Inner mucous membrane, fibrous middle layer, outer cutaneous layer. All held in place with a ring of cartilage
Behind they tympanic membrane are the Ossicles - 3 tiny bones of the middle ear:
Malleus (hammer) - bone attached to the tympanic membrane that passes the vibrations on to the incus
Incus (anvil) - send the signals to the stapes
Stapes (stirrup) - pump against the oval window, sending the sound onward to the inner ear.
Eustachian Tubes connect the middle ear to the pharynx and equalizes pressure on both sides of the eardrum
Cochlea - Inner Ear - a fluid-filled compartment housing the organ of Corti.
Organ of Corti - sensitive element, housing over twenty thousand hair cells and each hair cell contains forty to one hundred hairs each.
Hairs transduce the mechanical sound vibrations into electrical impulses, that are sent to the temporal lobe via the auditory nerve
Vestibules - complex set of fluid filled channels that contribute to balance and equilibrium
Contains the cochlea, labyrinth of the inner ear, and the semicircular canals
Semicircular canals (3 of them) - filled with fluid that regulate balance and sense of the head's position
Coder Note: 2 types of services pertaining to the ear - Audiometry services & Surgical Services
|
Ear Pathologies -
Hearing Loss - When the patient is not able to hear as well, and the degree of loss can be mild, moderate, profound
Conductive Hearing Loss - due to a defect in one or more of the sound conducting apparatuses such as impacted cerumen, scar tissue on the tympanic membrane, otitis media, or otosclerosis
Treatment - Hearing Aids
Sensorineural Hearing Loss - caused by a lesion on the cochlea or central neural pathways. Or due to a defect in the cochlear receptor or transducing mechanism (cochlear), a defect proximal to the cochlea (retrocochlear), or to presbycusis (age related hearing loss)
Treatment - Surgery to remove lesions and/or cochlear implants
Ototoxic Hearing Loss - caused by ingesting toxins that damage the inner ear
Treatment - Not reversible. Sometimes requires hearing aids or cochlear implants to mitigate
Meniere's Disease (Idiopathic Endolymphatic Hydrops) - Disturbance of the inner ear. Increased hydraulic pressure within the inner ear causes vertigo, tinnitus, hearing loss, and aural fullness (the feeling of fullness or pressure on the ears)
Treatment - Relieving symptoms
Diuretics - Reduce overall fluid levels
Motion Sickness medications may help with episodes of vertigo
Antihistamines may help with vertigo
Intratympanic steroid injections deliver steroids to the middle ear, reducing inflammation and increase circulation in the labyrinth
Otitis Media - Infection of the middle ear.
During upper respiratory infection, the Eustachian tube can become blocked by mucous, providing a breeding ground for bacteria. Making the tympanic membrane become red and inflamed and cause otalgia.
Can be unilateral or bilateral
Treatment - antibiotics. Chronic infections can cause adhesions and hearing loss, often treated by implantation of drainage tubes
Otitis Externa - Swimmers ear. Infection of the external auditory canal and auricle. Caused by bacteria or fungus, causing otalgia and discharge.
Treatment - Antibiotics
The Organ of Touch - Skin
Hyper- | High, beyond, excessive |
Hypo- | Under, beneath |
-algesia | Pain |
-esthesia | Feeling, sensation |
Touch Medical Terms:
Afferent Neurons - Sensory nerves, responsible for bringing sensory information to the brain
Efferent Neurons - Motor nerves, responsible for carrying signals from the brain to the rest of the body to perform an action
Haptic Perception - Perception of touch
Nociception - Perception of pain
Proprioception - perception of body movement and where it is in the environment
Thermoception - Perception of temperature
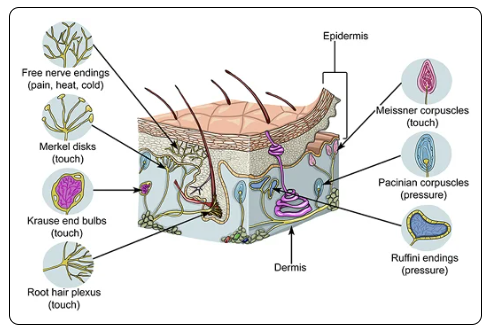
Touch Anatomy & Physiology
Somatosensory System - Sense of touch. Widespread neural network that bring sensory input from the body to the brain.
4 types:
Mechanoreceptors - detect pressure and texture
Thermoreceptors - senses change in temperature
Proprioceptors - Detect movement and position of the body
Nociceptors - sense pain
Sensory receptors transmit information via afferent neurons to the brain. Brain gives them instructions on how to respond to given stimuli via efferent neurons
Touch Pathologies:
Hyperalgesia - Abnormally heightened sensitivity to pain. Can be caused by damage to nociceptors or peripheral nerves, or from long-term opioid use.
Treatment - No sure. Managed with NSAIDs, glucocorticoids, gabapentin, NMDA receptor antagonists, or atypical opioids
Hypoesthesia - Numbness. Mainly caused by nerve damage and blood vessel blockage.
Treatment - aimed at the underlying diagnosis
The Organ of Smell - The Nose
Nas/o- | Nose |
-osmia | Smell |
Rhin/o- | Nose |
Sinus/0 | Sinus cavity |
Smell Medical Terms:
Anosmia - Loss of sense of smell
Dysosmia - Distortion of smells
Hyperosmia - Overly acute sense of smell
Hyposmia - Decreased sense of smell
Parosmia - All substances smell bad
Phantosmia - Smelling things that aren't there
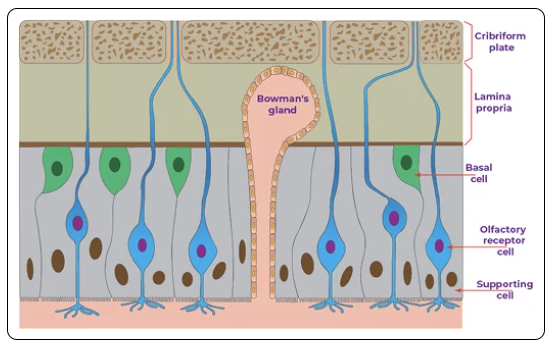
Smell Anatomy & Physiology - Smells enter nasal cavity
Nasal Epithelium - covers the upper portion of the nasal cavity and is full of olfactory receptors
Olfactory Receptors - Responsible for detecting smell. Have 2 ends:
Peripheral dendrites that reach the surface of the epithelium and end in very fine filaments (hairs)
Filaments analyze smell very quickly as the scent molecules come in contact with them, then transmit that signal along the olfactory tract to the bulb
Long nerve fiber that extends into the olfactory bulb
Olfactory Bulb - the neural structure located in the forebrain that receives input from the olfactory receptors and passes them on to the amygdala and hippocampus
Sense of smell is the only sense that bypasses the thalamus altogether - which is the relay station of the brain. Which is why a scent can instantly bring to mind a vivid memory connected to it.
Smell Pathologies:
People often lose their sense of smell during or following a viral upper respiratory infection
COVID - can cause anosmia or parosmia due to continuing viral presence, lingering inflammation, and damage to the olfactory epithelium
The Organ of Taste - The Tongue:
Acet/o- | Sour |
Acri/o- | Bitter |
-geusia | Taste |
Gloss/o- | Tongue |
Glyc/o- | Sweet |
Gust/o- | Taste |
Lingu/o- | Tongue |
Or/o- | Mouth |
Palat/o- | Palate |
Salin/o- | Salty |
Stomat/o- | Mouth |
Taste Medical Terms:
Ageusia - Lack of sense of taste
Dysgeusia - Distorted sense of taste
Hypogeusia - Decreased sense of taste
Taste Anatomy and Physiology:
Tongue - The only skeletal muscle in the body with sensory capabilities
A large part of taste is related to smell
When food is chewed, air is force into the nasal cavity carrying odorants from the food
Can detect 5 flavors:
Salty
Sour
Bitter
Savory
Sweet
Vallate Papillae - located on the anterior dorsum (back) of the tongue
House 50% of all tastebuds
Foliate Papillae - rough, close folds on the sides of the tongues posterior and contain several hundred tastebuds
Fungiform Papillae - mushroom shaped structures. Roughly 200-400 of them, concentrated on the sides and tip of the tongue. Each one has 3-5 taste buds, as well as mechanoreceptors and thermoreceptors
Filiform Papillae - Most numerous structures on the tongue. Have mechanoreceptors but no tastebuds. Food comes in contact with the tastebuds and enters the pores
Gustatory Cells - detect flavor present. Signal travels along the sensory nerve fibers to cranial nerves 7 and 9, to the insular cortex
Taste Pathologies:
Ageusia - Lack of taste. Rare, but can also be caused by upper respiratory infections, covid, head trauma, or salivary gland infections
Treatment - addressing underlying condition causing the issue
Dysgeusia - Distorted taste. Patient will complain food tastes bitter or metallic, or a lingering unpleasant taste in the mouth even without having eaten anything. Side effect of medications or pregnancy, or related symptom to conditions with smell
Treatment - addressing the underlying condition causing the issue
 Knowt
Knowt