Degenerations and Dystrophies: Conjunctiva
Dystrophies: conditions that are inherited
Degenerations: something that occurs due to some type of noxious influence (e.g., aging, nutrient intake, inflammation).
Dystrophies and Degenerations of the Conjunctiva
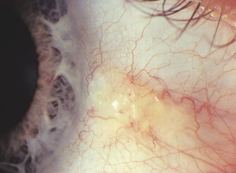
Pingueculae
Definition: Degeneration of the conjunctiva.
Appearance: Yellowish gelatinous nodule on the bulbar conjunctiva near the nasal and temporal limbus.
Pathology: Hyaline degeneration with elastic fibers being laid down.
Causes: Associated with chronic UV exposure and chronic irritation from wind and dust.
Prevalence: Ubiquitous in Australia, benign, usually asymptomatic, and of little significance (no threat to sight).
management: reassurance, advice on UV protection, tear supplements can be used to reduce dryness/ irritation. Surgery is rarely required.
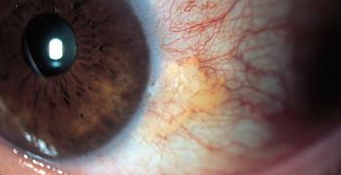
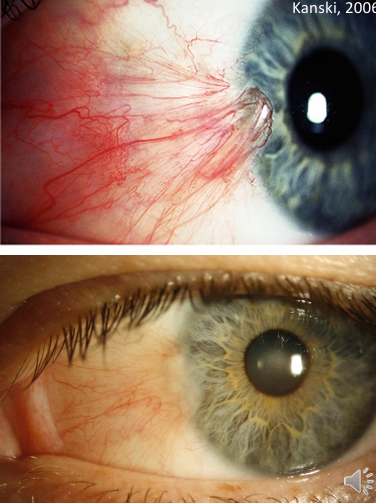
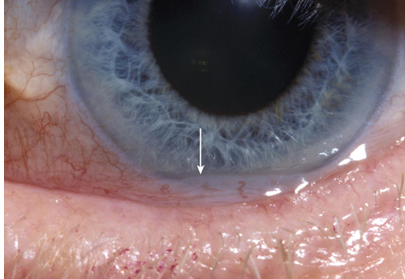
Pterygium
Definition: Wing-shaped vascularized growth extending onto the cornea.
Risk Factors:
More common in hot climates.
Chronic UV exposure, ocular dryness, and irritation.
Common Locations: Most commonly nasal; rare temporal pterygium.
Associated Signs: Stocker’s line - iron line in corneal epithelium forward of the apex.
Symptoms:
Ocular surface irritation.
Dryness and foreign body sensation.
Potential for pterygium to cause dellen (localized corneal depression due to chronic disruption of tear film).
Impact on Vision: Can affect vision by increasing astigmatism (worse with the trend towards regular astigmatism) and irregular corneal distortion.
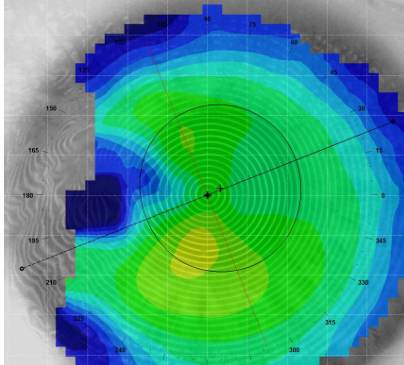
Topography Pterygium
corneal topography can be a useful tool
establishes a baseline for pterygium size and effects on corneal shape and astigmatism (WTR increase)
allows precise monitoring for future follow-up
useful for illustrating to patients the effects of the pterygium
Management of Pterygium
Prevention and Advice:
Advise on UV protection.
Use of eye lubricants for irritation symptoms.
Acute Management: Redness/inflammation can be treated with anti-inflammatory drops (e.g., FML).
Indications for Surgical Removal:
Visual acuity concerns.
Irregular astigmatism (distorted keratometer mires).
Cosmetic reasons.
Persistent inflammation/redness.
Pterygium size - if it extends more than halfway between the pupil margin and the centre of the cornea, consider referral.
Surgical Treatment of Pterygium
Procedure: Surgical removal of pterygium; bare sclera covered with an autoconjunctival graft.
Benefits: Reduces recurrence rates (0.5-5%, depending on specific surgical technique).
Additional Therapy: Mitomycin C used post-op can aid in reducing recurrence.
Post-Surgery Care:
Discomfort, photophobia, and blurred vision expected for the first week.
Application of antibiotic (Chloramphenicol) and steroid (Predforte) eye drops every 4 hours during the first month.
Gradual return of corneal curvature to normal in the months following surgery.
Pterygium and Ocular Surface Complications
Research Findings: Higher rates of ocular surface squamous neoplasia found in pterygium specimens (13.3%) than expected based on clinical exam.
Caution: Temporal pterygium may indicate squamous dysplasia or squamous cell carcinoma.

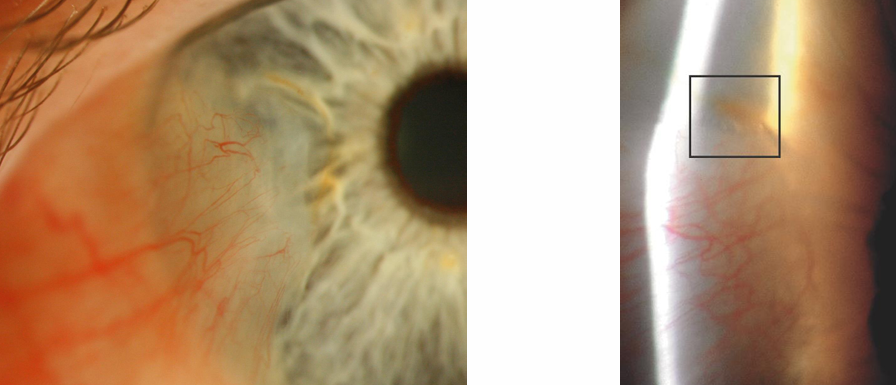
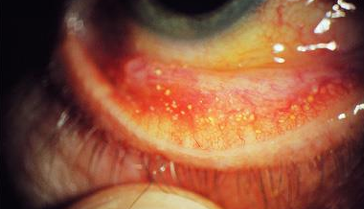
Concretions (Lithiasis)
Definition: Small punctate, hard yellow deposits in the conjunctiva. Made up of degenerating epithelial cells and proteins that become trapped in the conjunctiva and then undergo calcification over time.
Common Location: Typically found in the inferior palpebral conjunctiva.
Prevalence: Very common in elderly patients, generally asymptomatic as they usually sit under the epithelium.
Symptoms: typically, asymptomatic. Can lead to irritation or foreign body sensation if large concretion erodes through the epithelium.
Management for Irritation:
Removal using a bent 25-gauge needle at the slit lamp with local anaesthetic.
Followed by prophylactic coverage with broad-spectrum topical antibiotic (e.g., Tobradex or Chloramphenicol).
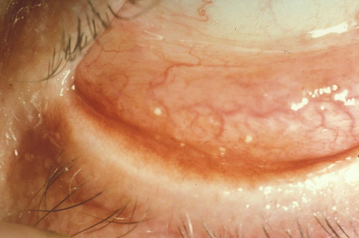
Conjunctivochalasis
Definition: A normal aging change to conjunctiva characterized by folds of redundant conjunctiva.
Common Presentation: Between the globe and lower eyelid, protruding over the lid margin.
Symptoms: Often asymptomatic but can exacerbate dry eye symptoms and commonly contributes to epiphora.
Management:
Topical lubricants for symptomatic relief.
Treatment for any accompanying blepharitis.
Short course of topical steroids may be helpful if symptomatic.
Severe cases may require surgical resolution (conjunctival resection).
 Knowt
Knowt