Obstructions
Learning Outcomes
Describe Mechanical Obstructive Diseases: Understand and classify mechanical obstructive diseases affecting dogs and cats, including the pathophysiological mechanisms involved in these conditions.
Explain Pathogenesis: Detail the development and progression of conditions like constipation, neoplasia, and foreign body obstruction, highlighting the cellular and systemic impacts of these diseases.
Clinical Signs and Diagnosis: Recognize signs and diagnostic approaches for these diseases, detailing the clinical history, examination techniques, and advanced diagnostic modalities used in practice.
Mechanical Obstructive Disorder
Definition: A mechanical obstructive disorder is characterized by a physical blockage or narrowing of a passageway within the body, which obstructs the normal flow of essential substances such as air, blood, and digestive content. In the veterinary context, these disorders are particularly significant in the gastrointestinal (GI) tract, where timely diagnosis and management can have critical outcomes.
Focus Area: This overview primarily addresses mechanical obstructive disorders of the intestines, particularly their implications in dogs and cats.
Classifications of Mechanical Obstructions
Importance of Classification: Understanding the classification system is crucial in determining the severity of the obstruction, establishing prognosis, and selecting appropriate treatment strategies. It plays a pivotal role in guiding clinical decision-making regarding surgical versus medical management.
Types of Classification:
Anatomical Region: Differentiation between Small Bowel and Large Bowel obstructions, each having distinct implications for treatment and outcomes.
Cause-Based: Classifications include Intraluminal (caused by contents within the lumen), Intramural (arising from the intestinal wall), and Extramural (external pressure or growth).
Obstruction Degree: Classifying obstructions as Partial or Complete is essential for determining urgency in treatment.
Vascular Status: Differentiating between Strangulating (compromised blood supply) and Non-Strangulating obstructions can help assess the risk of ischemia and tissue death.
Onset Duration: Acute obstructions present suddenly and require immediate intervention, while Chronic obstructions may develop gradually, allowing for more conservative management options.
Etiology: Differentiating between Congenital (malformations present at birth) and Acquired (developing over time due to factors such as diet or environment).
Pathogenesis Overview
Initial Obstruction & Luminal Distention: Occurs when a physical blockage prevents the passage of contents, leading to distended loops of the intestine.
Increased Intra-luminal Pressure & Reduced Motility: Pressure buildup can impair normal peristalsis, resulting in further digestion and absorption issues.
Mucosal Injury & Bacterial Overgrowth: Prolonged obstruction can lead to damage of the intestinal lining and excessive bacterial growth, complicating the condition and potentially leading to infection.
Venous Congestion & Ischemia: Compromise in blood flow due to pressure and obstruction can lead to tissue ischemia, increasing the risk of necrosis.
Systemic Effects: The systemic impact of an obstruction can manifest as electrolyte imbalances, metabolic derangements, and multiorgan dysfunction.
Endotoxemia & Septic Shock: Severe cases can lead to the absorption of toxic substances from dead bacteria, resulting in systemic inflammatory response syndrome and possibly septic shock.
Clinical Signs of Mechanical Obstructions
Gastrointestinal Signs:
Vomiting: May occur frequently, often bilious, manifesting different shapes (e.g., projectile) and volumes.
Abdominal Distension and Pain: Palpation may yield tense abdomen, indicating significant distention and pain.
Anorexia and Dehydration: Reduced or absent appetite can lead to clinical signs of dehydration, necessitating supportive care.
Tenesmus: Difficulty or pain during defecation, which can vary from absence of feces to diarrhea, depending on the location and nature of the obstruction.
Systemic Signs (if severe):
Weakness and Lethargy: Indicating systemic illness and potential shock.
Fever: May indicate secondary peritonitis if the obstruction leads to intestinal perforation.
Shock: Can develop in cases of perforation, necrosis, or severe dehydration, necessitating immediate medical attention.
Diagnostic Tests
Combination of Tests: An ideal diagnostic approach will combine clinical signs, thorough physical examination, and appropriate diagnostic testing to confirm the type and extent of obstruction.
Common Diagnostic Tests:
Abdominal Radiographs: Often the initial imaging study, providing insight into fluid levels, distended loops, and potential foreign bodies, used with or without contrast.
Abdominal Ultrasound: Offers real-time visualization of the abdominal structures, identifying masses or fluid accumulation.
GI Endoscopy: Useful for direct visualization of the GI tract and potential removal of foreign bodies.
Exploratory Surgery: May be required when non-invasive diagnostics are inconclusive or if there is a high suspicion of severe disease.
Treatment Overview
Non-Surgical (Conservative):
Fluid Therapy: Essential for rehydration and correcting electrolyte imbalances.
Dietary Management: Adjusting dietary inputs can help alleviate minor obstructions.
Medications: Laxatives, antiemetics, and analgesics to manage symptoms and discomfort.
Surgical (Aggressive):
Exploratory Laparotomy, Gastrotomy, Enterotomy, Resection & Anastomosis: Surgical interventions are indicated for severe and life-threatening obstructions.
Combination Treatments:
Conservative and surgical options may be applied concurrently to optimize outcomes.
Treatment Indications
For Conservative Treatment:
Indicated for Partial obstructions in stable patients or for Non-life-threatening conditions like mild constipation.
For Surgical Treatment:
Necessary for Complete obstructions, unstable patients, and situations presenting severe risk to patient health (e.g., peritonitis, necrosis).
Complications of Untreated Obstructions
Untreated obstructions can lead to several serious complications:
Perforation & Peritonitis: Opening of the intestinal wall leads to inflammation and infection of the abdominal cavity.
Severe Dehydration & Electrolyte Imbalance: Resulting from ongoing fluid losses associated with vomiting and lack of intake.
Sepsis & Systemic Infections: Potentially fatal systemic infections resulting from the contents entering the abdominal cavity or bloodstream.
Strangulation & Tissue Death (Necrosis): Impaired blood flow leading to irreversible damage to intestinal tissues, requiring aggressive surgical intervention.
Death: The ultimate outcome if treatment is not pursued promptly.
Common Mechanical Obstructive Disorders Focused In This Lesson
Constipation: Defined as infrequent, incomplete, or difficult evacuation of feces; can lead to obstipation and megacolon if untreated.
Foreign Body Obstruction: When an ingested foreign object blocks the normal flow through the GI tract, often requiring intervention.
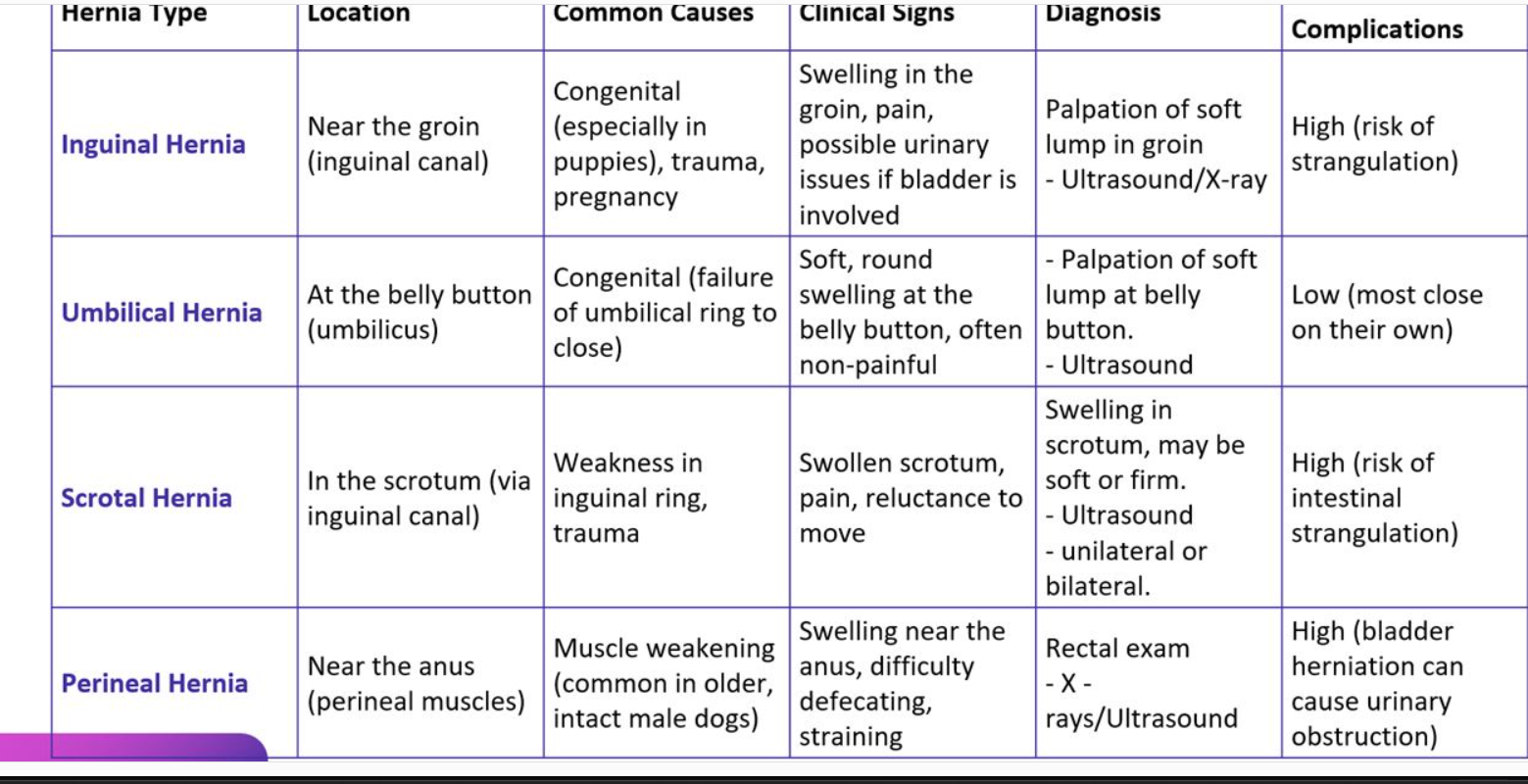
Herniation: Abnormal displacement of an organ or tissue through an opening in the body.
Neoplasia: Tumor formation can lead to obstructions in various anatomical sites.
Intussusception: A condition where a part of the intestine telescopes into an adjacent segment, often resulting in obstruction and compromised blood supply.
Volvulus/Torsion: Twisting of the intestine which can obstruct blood flow and lead to rapid progression of severe clinical signs.
Constipation
Definition: Characterized by infrequent, incomplete, or difficult fecal evacuation; if unresolved, it can progress to obstipation and megacolon, requiring more aggressive management.
Predisposing Factors:
Low-fiber diets, dehydration, lack of exercise, stress, foreign bodies, pelvic mechanical obstructions, or medications that affect motility such as opioids.
Pathogenesis Steps:
Inadequate colonic motility: Results in slow transit times leading to fecal build-up.
Fecal retention & dehydration: Moisture draws out of the feces, resulting in hard, dry stools.
Colonic distention and weak muscles: Continued pressure leads to distended convolutions of the colon.
Mucosal injury & inflammation: Potential development of colitis or mucosal tearing.
Clinical Signs of Constipation
Infrequent or absent defecation: Notably dry, hard feces that may cause straining.
Straining without producing feces: Indicative of significant obstruction.
Painful defecation: Often leads to behavioral changes, lethargy, or vomiting in severe cases where pain is improperly managed.
Diagnosis of Constipation
History & Physical Exam: Involves understanding dietary habits, hydration status, and behavioral responses regarding defecation; essential abdominal palpation should focus on identifying impacted feces.
Imaging: Radiographs help visualize fecal loading; ultrasound can identify masses; contrast studies used to assess for strictures or obstructions.
Laboratory Tests: To rule out underlying metabolic disorders or electrolyte imbalances that may contribute to constipation.
Special Species Considerations
Cats: More commonly prone to idiopathic megacolon, often necessitating long-term management strategies to prevent recurrence.
Dogs: Obstructions more frequently related to pelvic fractures, tumors, or dietary indiscretions, each needing tailored approaches to management.
Treatment of Constipation
Mild/Moderate Cases: May be managed with dietary modifications, introduction of laxatives, maintaining hydration, encouraging regular exercise, and using enemas if necessary to relieve fecal impaction.
Severe Cases: May require manual evacuation, administration of intravenous fluids, and consider surgical intervention such as subtotal colectomy for chronic, intractable cases with significant colonic dilation.
Foreign Body Obstruction (FBO)
Definition: An ingested object obstructing the normal flow of contents through the GI tract, potentially leading to severe complications if not promptly addressed.
Types of Foreign Bodies:
Non-Linear: Solid, more rigid objects such as balls or bones.
Linear: String or thread-like materials that can cause serious complications by anchoring into the GI tract.
Clinical Signs of FBO
Common Symptoms: Consistent vomiting, loss of appetite, noticeable abdominal pain upon palpation, diarrhea (sometimes mixed with blood), and varying levels of dehydration and lethargy.
Diagnosis of FBO
Bloodwork: Assists in evaluating dehydration and infection signs.
Imaging Techniques: Radiographs or ultrasound can help visualize the foreign body and any associated complications, including perforation.
Exploratory Surgery: May be warranted if non-invasive diagnostic techniques do not adequately address the blockage or if critical signs develop.
Treatment of FBO
Conservative: For minor or suspected partial obstructions, supportive care with fluids and close monitoring may suffice.
Aggressive: Surgical interventions are typically required where there is evidence of significant damage or when the obstruction leads to ischemia, such as gastrotomy or enterotomy to remove the foreign body directly.