Chapter 35: Rest and Sleep
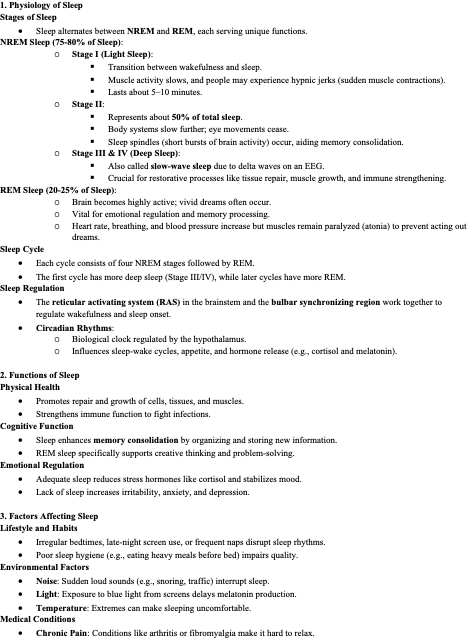
1. Physiology of Sleep
Stages of Sleep
Sleep alternates between NREM and REM, each serving unique functions.
NREM Sleep (75-80% of Sleep):
Stage I (Light Sleep):
Transition between wakefulness and sleep.
Muscle activity slows, and people may experience hypnic jerks (sudden muscle contractions).
Lasts about 5–10 minutes.
Stage II:
Represents about 50% of total sleep.
Body systems slow further; eye movements cease.
Sleep spindles (short bursts of brain activity) occur, aiding memory consolidation.
Stage III & IV (Deep Sleep):
Also called slow-wave sleep due to delta waves on an EEG.
Crucial for restorative processes like tissue repair, muscle growth, and immune strengthening.
REM Sleep (20-25% of Sleep):
Brain becomes highly active; vivid dreams often occur.
Vital for emotional regulation and memory processing.
Heart rate, breathing, and blood pressure increase but muscles remain paralyzed (atonia) to prevent acting out dreams.
Sleep Cycle
Each cycle consists of four NREM stages followed by REM.
The first cycle has more deep sleep (Stage III/IV), while later cycles have more REM.
Sleep Regulation
The reticular activating system (RAS) in the brainstem and the bulbar synchronizing region work together to regulate wakefulness and sleep onset.
Circadian Rhythms:
Biological clock regulated by the hypothalamus.
Influences sleep-wake cycles, appetite, and hormone release (e.g., cortisol and melatonin).
2. Functions of Sleep
Physical Health
Promotes repair and growth of cells, tissues, and muscles.
Strengthens immune function to fight infections.
Cognitive Function
Sleep enhances memory consolidation by organizing and storing new information.
REM sleep specifically supports creative thinking and problem-solving.
Emotional Regulation
Adequate sleep reduces stress hormones like cortisol and stabilizes mood.
Lack of sleep increases irritability, anxiety, and depression.
3. Factors Affecting Sleep
Lifestyle and Habits
Irregular bedtimes, late-night screen use, or frequent naps disrupt sleep rhythms.
Poor sleep hygiene (e.g., eating heavy meals before bed) impairs quality.
Environmental Factors
Noise: Sudden loud sounds (e.g., snoring, traffic) interrupt sleep.
Light: Exposure to blue light from screens delays melatonin production.
Temperature: Extremes can make sleeping uncomfortable.
Medical Conditions
Chronic Pain: Conditions like arthritis or fibromyalgia make it hard to relax.
Respiratory Issues: Sleep apnea or asthma disrupts breathing during sleep.
GERD: Lying down may worsen acid reflux, causing discomfort.
Medications
Stimulants (e.g., amphetamines, caffeine): Interfere with sleep onset.
Diuretics: Can cause frequent urination, disrupting sleep.
Sedatives: Help with sleep but may reduce restorative REM sleep if misused.
Age Variations
Infants: Sleep is polyphasic, with frequent naps during the day.
Adults: Often require 7–8 hours; reduced deep sleep occurs with aging.
Older Adults: Experience frequent nighttime awakenings and lighter sleep.
4. Common Sleep Disorders
Insomnia
Persistent difficulty falling or staying asleep.
Can be caused by stress, anxiety, or poor sleep hygiene.
Chronic insomnia leads to fatigue, cognitive impairment, and mood disturbances.
Sleep Apnea
Temporary cessation of breathing during sleep, leading to fragmented sleep.
Obstructive Sleep Apnea (OSA): Caused by upper airway collapse.
Symptoms include loud snoring, daytime drowsiness, and morning headaches.
Narcolepsy
A neurological disorder causing sudden, uncontrollable sleep episodes.
May include cataplexy, a loss of muscle control triggered by strong emotions.
Restless Legs Syndrome (RLS)
Tingling or crawling sensations in the legs, usually at night.
Movement provides relief but disrupts sleep continuity.
Parasomnias
Sleepwalking: Occurs during deep sleep; person may perform complex behaviors while unconscious.
Night Terrors: Sudden arousal from sleep with intense fear, more common in children.
5. Assessment of Sleep
Sleep History
Ask about:
Bedtime and wake-up routine.
Sleep quality (how refreshed the patient feels).
Use of medications or substances that affect sleep.
Symptoms like snoring, nightmares, or leg movements.
Sleep Diary
Record sleep habits over 1–2 weeks:
Bedtime, wake time, interruptions, and naps.
Physical Exam
Look for signs of sleep deprivation:
Dark circles, irritability, reduced alertness.
Diagnostic Tests
Polysomnography: Measures brain activity, oxygen levels, and body movements during sleep.
Actigraphy: A wearable device that tracks rest and activity cycles.
6. Nursing Interventions
Sleep Hygiene
Establish a fixed bedtime and wake time.
Limit stimulants (e.g., caffeine) and alcohol in the evening.
Create a calming pre-sleep routine (e.g., reading or warm baths).
Environment Optimization
Keep the bedroom dark, quiet, and cool.
Use white noise machines if needed.
Ensure the bed and pillows are comfortable.
Lifestyle Adjustments
Encourage regular physical activity, but not close to bedtime.
Promote relaxation techniques, such as deep breathing or meditation.
Pharmacologic Interventions
Use hypnotics sparingly for short-term relief.
Recommend melatonin for circadian rhythm disorders if appropriate.
7. Patient Education
Stress the importance of consistent routines.
Teach relaxation strategies to reduce bedtime anxiety.
Educate on the effects of alcohol, nicotine, and caffeine on sleep quality.
Highlight the importance of seeing a specialist for persistent sleep issues.
8. Evaluation
Review the patient’s sleep diary to monitor progress.
Ask about changes in energy levels, mood, and cognitive performance.
Adjust interventions if the patient reports persistent difficulties