L5 Complicated Intra-Abdominal Infections (cIAIs)
Objectives
Causes and mechanisms of underlying Primary, Secondary, and Tertiary Peritonitis
with Diverticulitis, Cholecystitis/Cholangitis, and Pancreatitis
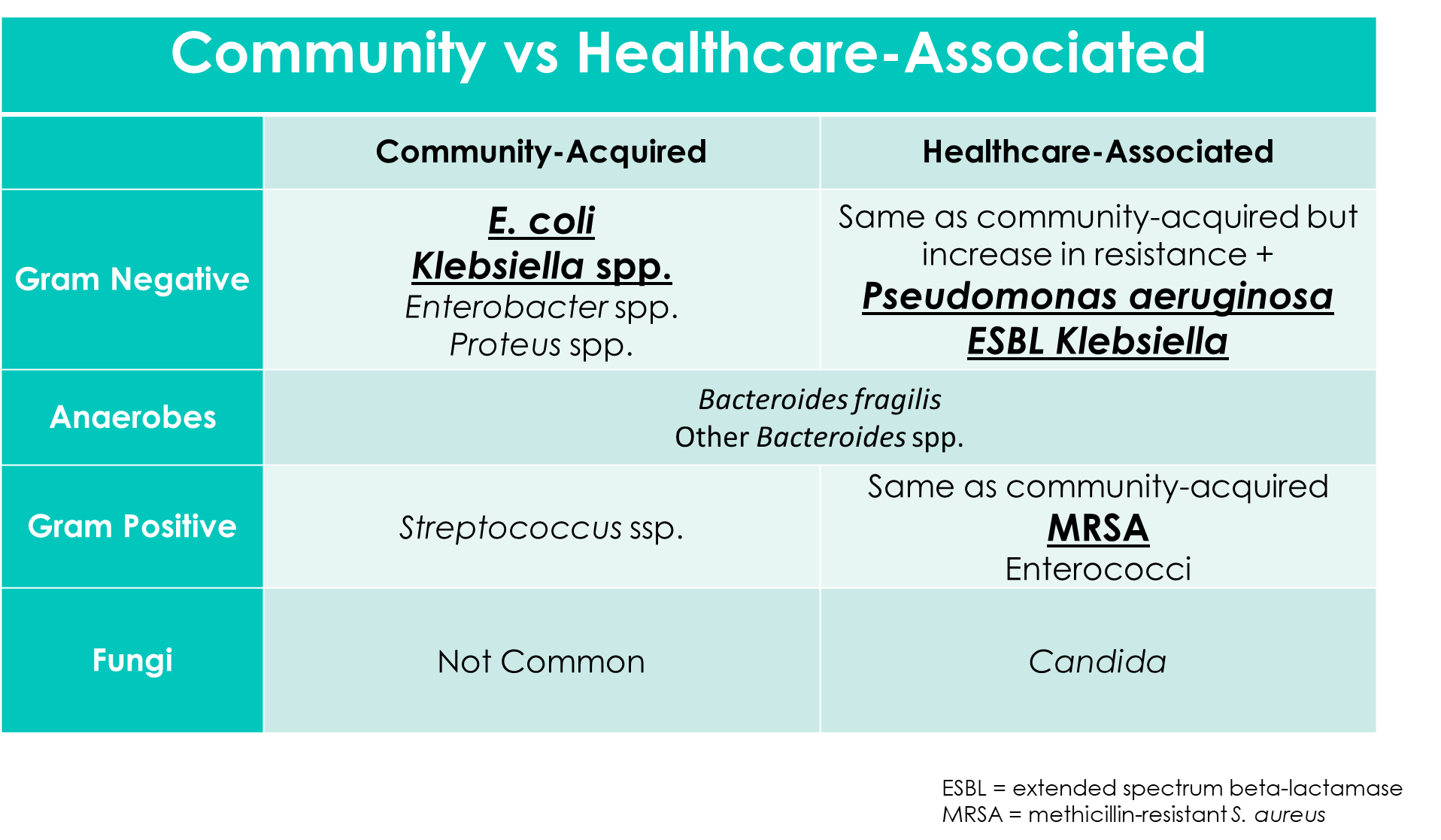
Differentiate common pathogens associated with Community-/Healthcare-Associated complicated infections
Understand clinical presentation
key signs, symptoms, PE findings, lab results, and imaging abnormalities
Recognize factors for high risk patients for treatment failure in cIAI management
Notes
T/F: cIAIs have low mortality and morbidity rates
False
What type of cIAI has a 30% occurrence in patients with Alcoholic Cirrhosis (serious liver disease that occurs when scar tissue replaces healthy liver tissue).
Primary Peritonitis
What portions of the abdomen does infection occur?
Peritoneal Cavity and Retroperitoneal Space

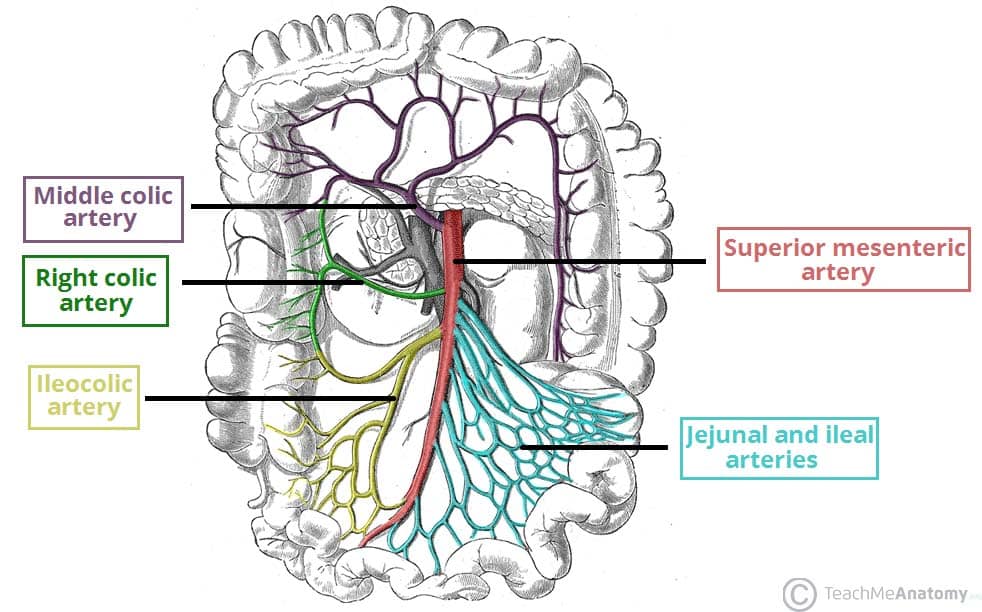
What organs make up the Retroperitoneal cavity?
Pancreas
Kidneys
Adrenal Glands
Great Vessels
Mesenteric Vascular Structures
What is Peritonitis
acute inflammatory response of the peritoneal lining
What causes Peritonitis
microorganism, chemical, or foreign-body injury
What is Abscess
purulent collection of fluid separated from surrounding tissue by a wall of inflammatory cells or adjacent organs
What causes Abscess
Necrotic Debris, Bacteria, Inflammatory Cells
What indicates an UNCOMPLICATED intra-abdominal infection
CONFINED in visceral structure (liver, gallbladder, spleen, kidney) and Peritoneum
What indicates a COMPLICATED intra-abdominal infection
Anatomical Disruption
Extends to more than one organ
Peritonitis and/or Abscess
What is PRIMARY Peritonitis also known as
Spontaneous Bacterial Peritonitis
What is Primary Peritonitis
peritoneal cavity infection WITHOUT evident source in abdomen
What are examples of possible causes of Primary Peritonitis?
Cirrhosis with Ascites
Nephrotic Syndrome
Peritoneal Dialysis
What is Secondary Peritonitis
peritoneal cavity infection WITH clear source in abdomen
What are examples of possible causes of Secondary Peritonitis?
GI perforation (ulceration, ischemia, obstruction)
Postoperative Peritonitis
Abdominal Solid Organ Transplant
Posttraumatic Peritonitis (blunt or penetrating trauma)
Diverticulitis
gastrointestinal disease that occurs when pouches in the large intestine become inflamed or infected
Appendicitis
Inflammatory Bowel Diseases
Biliary Tract Infection
Necrotizing Pancreatitis
Mechanical GI Problems
GI Anastomosis (procedure that connects two parts of the GI tract) leakage
What is Tertiary Peritonitis
peritoneal cavity infection that persists in critically ill patients or
recurring infection AT LEAST 48 hours after attempted management of 1° or 2° peritonitis
What are examples of possible causes of Tertiary Peritonitis
Severe/Recurrent Peritonitis
Abscess formation
Necrosis
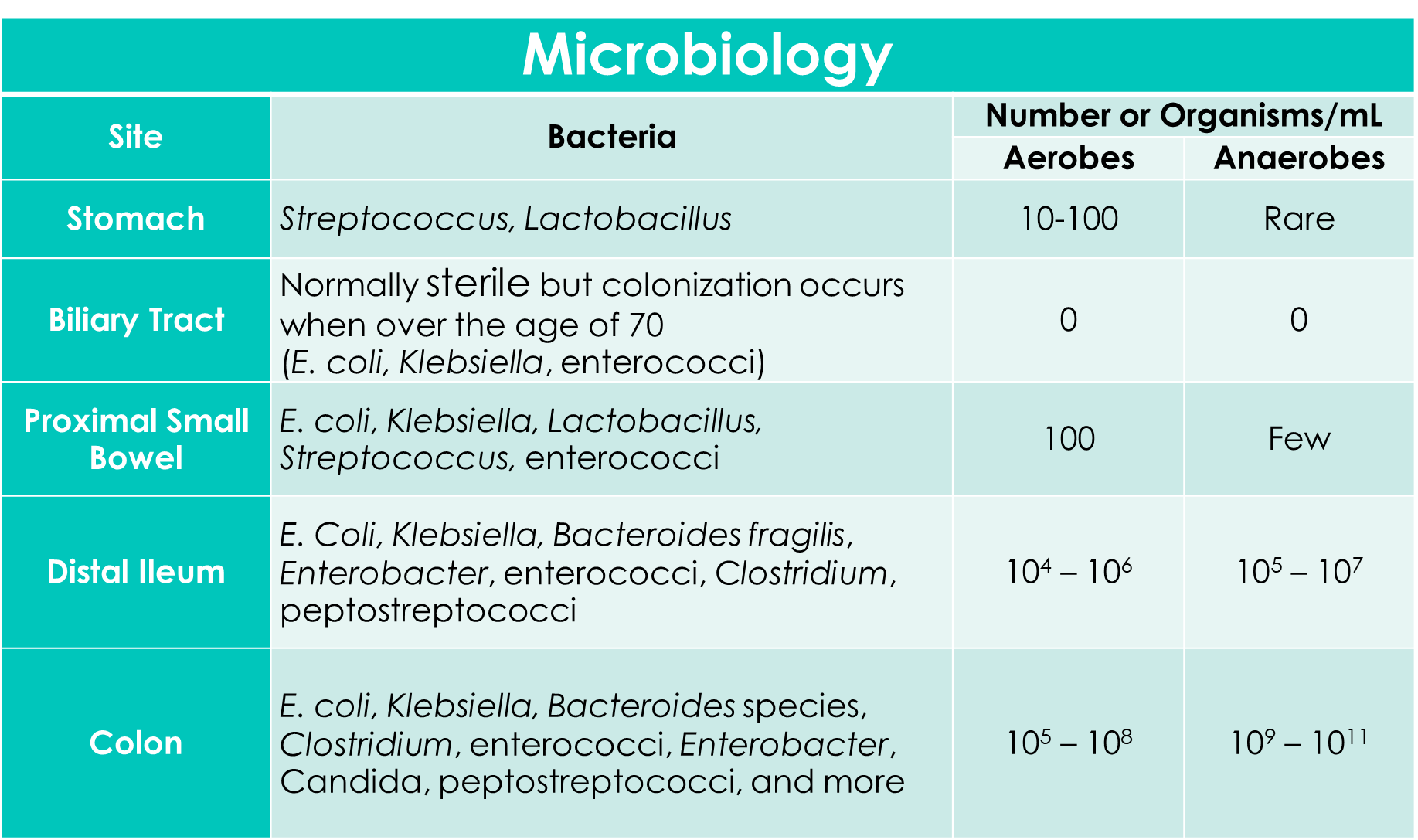
List the Pathophysiology steps
Bacterial Entry
via blood stream of collection within intra-abdominal organs
Host Response
Humoral and Cellular defenses
Bacterial Dissemination
failure to contain bacteria → peritoneal cavity entry → infection (Peritonitis)
Inflammatory Response
Leukocytes, Fibrin, and other proteins combined in Peritoneal Fluid
Third Spacing
Fluid and Proteins → abdomen → DECREASED blood circulation and Hypovolemic shock
What are Diverticula
small, bulging pouches that form in the walls of hollow organs
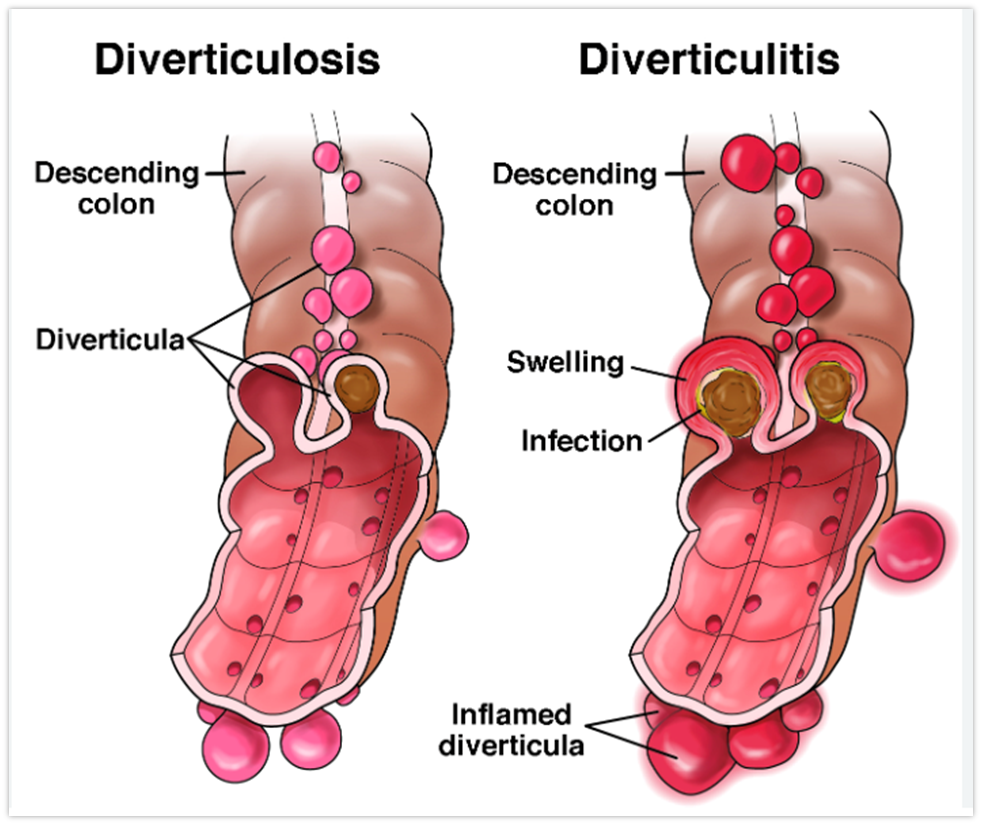
What triggers Diverticulitis
Micro-perforations or Obstruction
What can result in Obstructed Diverticulitis
INCREASED intraluminal pressure
DECREASED blood supply
Localized inflammation
due to stasis of intestinal contents
When is Diverticulitis considered severe?
Perforation → Peritonitis or Abscess
What makes up the Biliary Tract?
network of organs and ducts that produce, store, and transport bile, a fluid essential for fat digestion
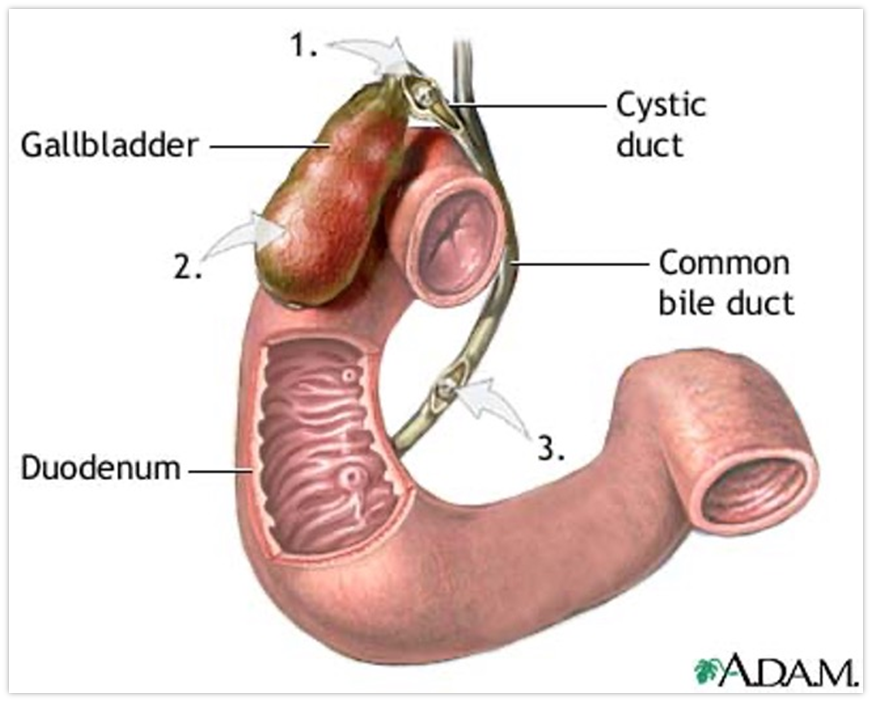
What types of infections can occur in the Biliary Tract?
Cholecystitis and Cholangitis
What is Cholecystitis
Gallbladder inflammation often caused by obstruction (Gallstone in Cystic Duct)
can lead to gallbladder wall ischemia, inflammation, and potential necrosis//perforation
What is Cholangitis
Bile Duct infection
T/F: Pancreatitis are only caused by infection
False, noninfectious as well
What are examples of infectious causes of Pancreatitis
Viruses
Fungi
Atypical Organisms
Parasites
Gram NEGATIVE Bacteria
What are examples of Non-infectious causes of Pancreatitis
Gallstones
Alcoholism
Hypertriglyceridemia
Hypercalcemia
CA
Anatomic Abnormalities
Drugs
What is Community Acquired Infection (CAI)
Caused by the patient’s own microflora and is present WITHIN 48 hours of hospital admission
What is Healthcare Associated Infection (HAI)
Community-onset with healthcare exposure risk factor and occurs AFTER 48 hours of hospitalization
Presence of Invasive Device
known MRSA infection/colonization
Healthcare facility residence
Dialysis
Prior Surgery within 12 months
What are Symptoms of cIAIs
N/V/D
Abdominal pain
Altered mental state
What are Signs of cIAIs
Fever
Hypotension
Tachy -cardia/-pnea
Hypoactive Bowel Signs (BS)
What are lab work observed for cIAIs
CBC — WBC
Blood and Source Cultures
Basic Metabolic Panel (BMP) — SCr and BUN
C-reactive Protein
is a sign of inflammation but is not specific enough??
What imaging tests are observed for cIAIs
Ultrasound
Computed Tomography (CT)
MRI
What are ultrasounds preferably used for in IAIs?
Biliary Tract Infections
What are CTs preferably used for in IAIs?
Abscess confirmation
T/F: MRIs are better than CTs for IAIs
False
What are the factors for high risk patients for treatment failure in cIAI management
Delayed initial intervention ≥ 24 hours
High illness severity (APACHE II score ≥ 15)
> 70
Pre-existing chronic conditions
Malignancy
Poor nutrition
Diffuse Peritonitis
Inadequate SOURCE control of infection
 Knowt
Knowt