7. KNSS 220 Introduction to Athletic Therapy: The Ankle & Lower Leg
KNSS 220 Introduction to Athletic Therapy
The Ankle & Lower Leg
Anatomy
Bones
Tibia
Fibula
Talus
Calcaneus
The Ankle Joint of the Right Foot
Anterior (front) view
Lateral (outside) view
Anatomy: Ligaments
Anterior and Posterior Inferior Tibiofibular Ligaments
Lateral Ligaments:
Anterior Talofibular Ligament
Posterior Talofibular Ligament
Calcaneofibular Ligament
Medial Ligament:
Deltoid Ligament
Anatomy: Articulations
Tibiofibular Joint
Talocrural Joint:
Components:
Trochlea of Talus
Articular facet on distal portion of the tibia
Medial Malleolus
Lateral Malleolus
Ankle Mortis
Lower Leg Injuries
Compartment Syndrome
Definition: The pressure within a compartment increases, restricting blood flow to the area and potentially damaging the muscles and nearby nerves.
CROSS-SECTION OF NORMAL CALF SHOWING MUSCLE COMPARTMENTS:
Deep Posterior Compartment
Anterior Compartment
Lateral Compartment
Superficial Posterior Compartment
Etiology: Muscle swelling causing compression.
Signs and Symptoms:
Pain and tenderness on the outside of the ankle
Swelling in the lateral aspect of the leg
Decreased range of motion and strength in the ankle
Difficulty weight-bearing or walking without support.
Management:
Apply R.I.C.E. (Rest, Ice, Compression, Elevation) principles to manage swelling and pain.
Consider a progression of range of motion exercises to restore mobility.
Implement strength training focused on the ankle and lower leg muscles to improve stability.
Use assistive devices (crutches or braces) to support weight-bearing as tolerated.
Medial Tibial Stress Syndrome (Shin Splints)
Etiology: Medial Tibial Stress Syndrome typically arises from repetitive stress on the tibia due to activities like running or jumping; it may also be exacerbated by improper footwear or biomechanical discrepancies such as flat feet.
Signs and Symptoms: Common signs and symptoms of Medial Tibial Stress Syndrome include pain along the inner part of the lower leg, tenderness or soreness during physical activity, swelling in the affected area, and pain that typically decreases with rest but reoccurs with activity.
Management:
Management of Medial Tibial Stress Syndrome includes several strategies:
Rest: Reduce or modify activities that exacerbate the symptoms, allowing the tibia to heal.
Ice therapy: Apply ice packs to the affected area for 15-20 minutes several times a day to reduce swelling and alleviate pain.
Stretching and strengthening exercises: Perform specific stretches for the calf muscles and strengthening exercises for the lower legs to address underlying muscle imbalances.
Footwear evaluation: Ensure adequate support and cushioning in shoes, and consider orthotic devices if structural issues are present.
Gradual return to activity: Reintroduce physical activity slowly, monitoring for pain or discomfort.
Peroneal Tendinopathies
Etiology: Sudden plantarflexion and dorsiflexion; acute ankle sprain.
Signs and Symptoms:
Pain along the lateral aspect of the ankle, especially during activities involving ankle movement.
Swelling and tenderness over the peroneal tendons.
Difficulty with activities requiring calf strength or balance, such as running or jumping.
Management:
Rest and ice application to reduce swelling and alleviate pain.
Compression bandaging to support the injured area.
Gradual rehabilitation exercises focusing on strengthening the calf muscles and improving balance.
Functional mobility training to restore full range of motion and prepare for a return to activity.
Ankle Injuries
High Ankle Sprain

Etiology:
Eversion
Dorsiflexion
Direct trauma
Signs and Symptoms: Common signs and symptoms of injuries to the ankle and lower leg include swelling, bruising, pain during movement, limited range of motion, tenderness to touch, and instability in the joint.
Management: Effective management strategies for ankle and lower leg injuries may include rest, ice application to reduce swelling, compression to limit edema, and elevation to minimize pain and promote healing.
Involved Structures:
Interosseous membrane
Syndesmosis tear
Anteroinferior Tibiofibular Ligament (AITFL)
Inversion Ankle Sprain
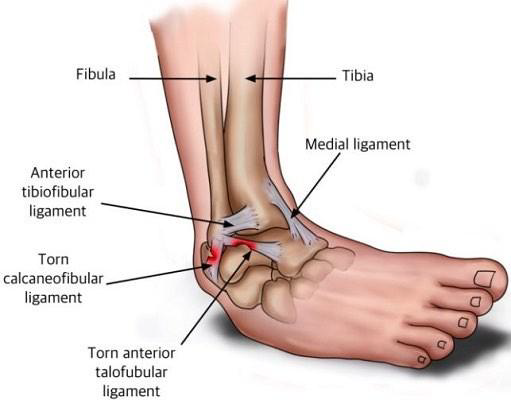
Etiology:
Caused by excessive inversion of the ankle, often during sports activities or sudden changes in direction.
Inversion
Plantarflexion
Signs and Symptoms:
Swelling around the ankle
Pain along the outer edge of the foot or ankle
Bruising that may spread to the foot
Difficulty bearing weight on the affected foot
Limited range of motion in the ankle joint
Management:
R.I.C.E. protocol (Rest, Ice, Compression, Elevation) to reduce swelling and pain
Gradual return to activity with controlled weight-bearing exercises
Strengthening exercises focusing on ankle stability and flexibility
Consultation with a physiotherapist for tailored rehabilitation program.
Involved Ligaments:
Torn calcaneofibular ligament
Torn anterior talofibular ligament
Anterior tibiofibular ligament
Eversion Ankle Sprain
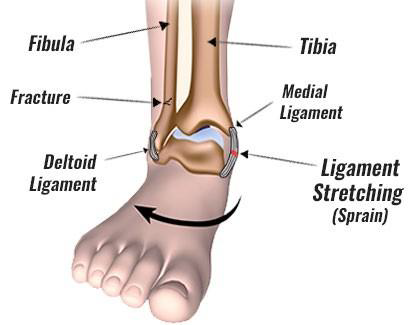
Etiology: The etiology of an ankle sprain often involves excessive inversion or eversion during physical activity, leading to strain on the ligaments that support the ankle joint.
Signs and Symptoms: Common signs and symptoms of an ankle sprain include swelling, tenderness to touch, bruising, limited range of motion, and difficulty walking or bearing weight on the affected ankle.
Management: Effective management of an ankle sprain includes the R.I.C.E. method: Rest, Ice, Compression, and Elevation. Additionally, rehabilitation exercises may be introduced to restore strength and flexibility.
Involved Structures:
Deltoid ligaments
Medial malleoli
Achilles Tendinopathy
Etiology:
The underlying causes of Achilles Tendinopathy include repetitive strain and overuse, often exacerbated by factors such as improper footwear, excessive training intensity, or biomechanical abnormalities.
Activities such as jumping, running, and sprinting
can lead to increased strain on the Achilles tendon, resulting in microtraumas and eventual degeneration if not properly managed.
Signs and Symptoms:
Pain, swelling, and stiffness of the Achilles tendon
Management:
Management strategies include rest, ice application, anti-inflammatory medications, physical therapy exercises to strengthen surrounding muscles, and gradual return to activity to prevent recurrence.
Types:
Mid-portion Achilles tendinopathy
Insertional Achilles tendinopathy
Achilles Rupture
Etiology: Overuse injuries, degeneration of the tendon due to repetitive stress, and anatomical factors such as abnormal foot mechanics and tight calf muscles.
Signs and Symptoms: Pain along the Achilles tendon, stiffness in the morning, swelling around the tendon, and difficulty with activities that involve pushing off the foot or raising the heel.
Characterized by a pop sound
Management:
Initial management includes the R.I.C.E protocol (Rest, Ice, Compression, Elevation) to reduce swelling and pain.
Once acute symptoms subside, rehabilitation involving range of motion, strengthening exercises, and proprioception training should be implemented.
Deep Vein Thrombosis
Etiology: Deep vein thrombosis (DVT) is primarily caused by prolonged inactivity, which can lead to blood pooling in the veins, increasing the risk of clot formation. Other contributing factors include trauma, certain medical conditions, surgery, and the use of medications that affect blood clotting.
Signs and Symptoms:
DVT may present with swelling, pain or tenderness in the affected leg, warmth, and discoloration. In some cases, patients may be asymptomatic despite having a clot.
Swollen leg
Management:
Elevation of the affected leg to reduce swelling
Compression therapy using bandages or stockings to improve venous circulation
Anticoagulant medications to prevent further clotting
Gradual mobilization and physical therapy to restore function, if appropriate
Monitoring for potential complications such as pulmonary embolism.
Ankle & Lower Leg Assessment
History
Who: Name, age, gender, job
Mechanism of injury:
What happened?
How did it happen?
When did it happen?
Pain:
Location
Onset: Gradual or acute
Type: Sharp, dull, ache, shooting
Severity: Scale of 1-10
What makes it feel worse and better?
Sounds/sensations: Did they feel or hear abnormal pop, snap, crack, etc.?
Signs and Symptoms
Previous health/injury history, medications/allergies
Observation
Always compare bilaterally
Look for:
Swelling, discoloration, deformity
Formations/abnormalities:
Pes planus/cavus
Hammer, claw, and mallet toe
Morton's toe
Inspection of medial, lateral, dorsal, and plantar views
Inspection of shoes and gait
Assessment
Temperature
Pulses:
Post tibialis
Dorsalis pedis
Soft tissue assessment:
Muscle: Gastrocnemius, Soleus, Anterior compartment, Lateral compartment
Tendons:
Plantar fascia
Ligaments:
ATFL
PTFL
CFL
Deltoid
Bones/bony prominences:
Calcaneus
Talus
Cuboid
Navicular
Cuneiforms 1-3
Metatarsals 1-5
Styloid process of 5th MT
Phalanges
Sesamoids
Tibia
Fibula
Lateral/medial malleoli
Range of Motion (ROM)
Ankle ROM:
Active Range of Motion (AROM)
Passive Range of Motion (PROM)
Resistive Range of Motion (RROM)
Movements:
Plantarflexion
Dorsiflexion
Eversion
Inversion
Toe ROM:
Movements:
Extension
Flexion
Special Tests
Anterior Drawer Test
Purpose: Assess the stability of the anterior talofibular ligament
Method: Stabilize the tibia and fibula with one hand, pull heel with the other.
Positive Test: Laxity and pain
Talar Tilt Test
Purpose: Assess stability of the lateral and medial ligaments of the ankle
Method: Same hand position as anterior drawer test, but put the ankle through eversion and inversion motions.
Positive Test: Pain and laxity over the deltoid ligaments during eversion and over the lateral ligaments during inversion
Kleigers Test
Purpose: Assess syndesmosis (high ankle sprain)
Method: Place the foot into dorsiflexion and eversion.
Positive Test: Pain between the distal tibia and fibula
Bump Test
Purpose: Assess for fractures in the lower leg
Method: Bump heel with the palm.
Positive Test: Pain present
Thompson Test
Purpose: Assess for an Achilles rupture
Method: Patient lies prone; squeeze the gastrocnemius/soleus complex.
Positive Test: No plantarflexion of the ankle