MB preparation - week 3
Hillegass, Chapter 6
COPD = chronic pulmonary obstructive disease
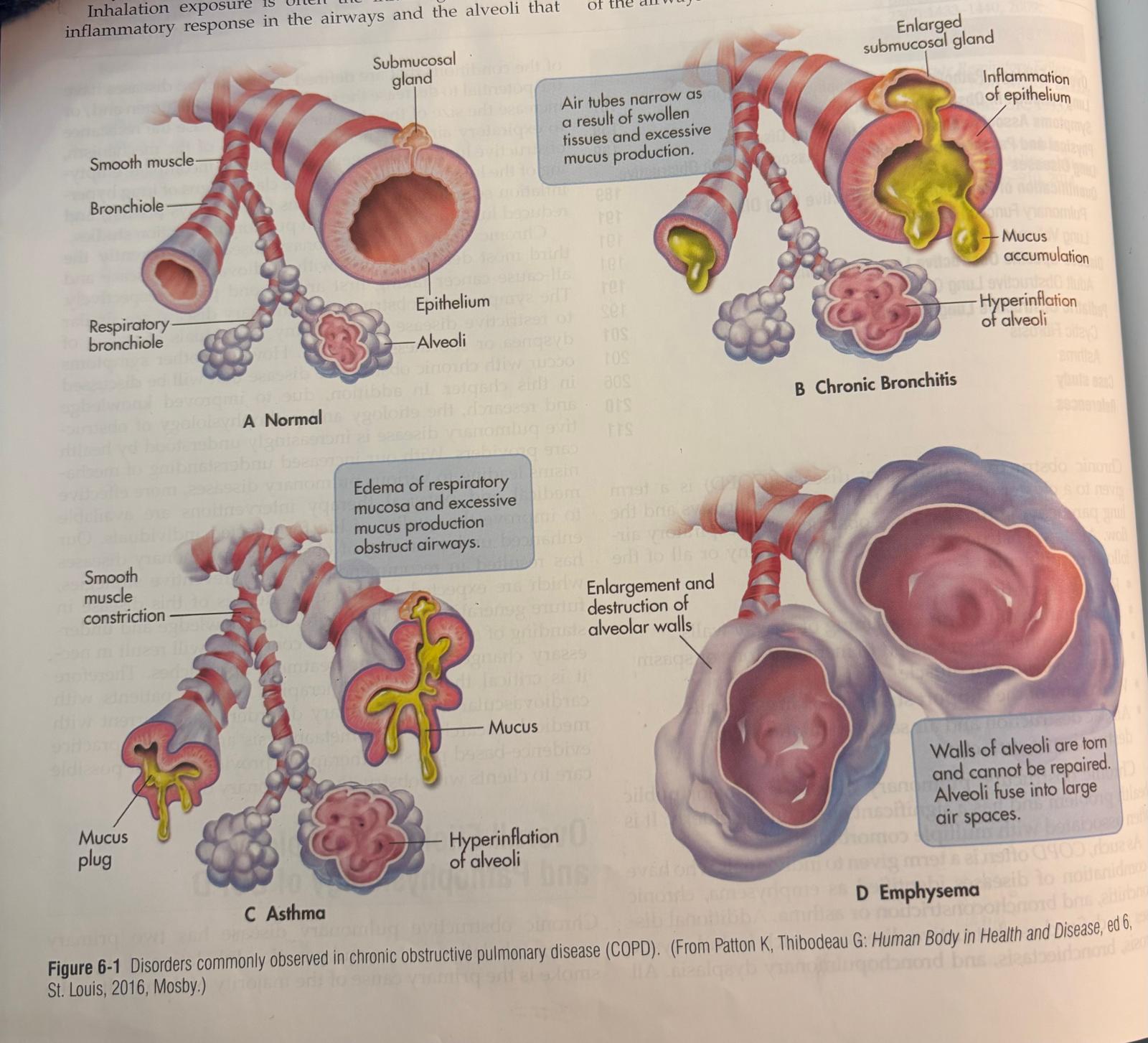
it’s a term given to a cluster of problems that affect the airways and the lung parenchyma that produce obstruction to the expiratory airflow
Airflow obstruction can be related to:
Retained secretions
Inflammation of mucosal lining of airway walls
Bronchial constriction related to increased tone or spasm of bronchial smooth muscle
Weakening of the support structure of airway walls
Air sac destruction and air sac overinflation with destruction of surfactant
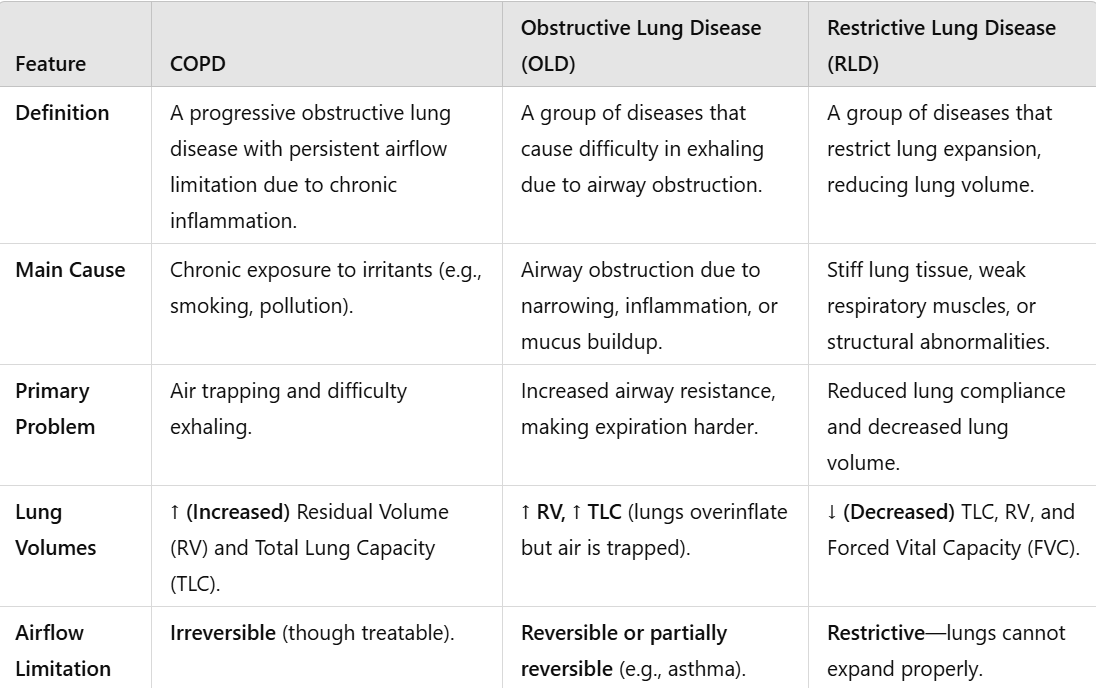
Differences between COPD and OLD
COPD = chronic pulmonary obstructive diseases
combination of diseases “emphysema“
chronic bronchitis
bronchoconstriction
asthma
OLD = obstructive lung disease
cystic fibrosis
bronchiectasis
bronchopulmonary dysplasia
OLD decrease the size of the bronchial lumen , increase size of alveolar sac and increase resistance of the expiratory flow
Characteristics
incomplete emptying of the lung → lung hyperinflation
reduced lung function
RLD different than OLD
In common they have:
shortness of breath
dyspnea
Etiology, Pathology and Pathophysiology of COPD and OLD
COPD
Causes:
1) Inhalation factors:
Cigarette smoke (active and passive)
Exposure to chemicals and air pollution
Occupational dust and fumes
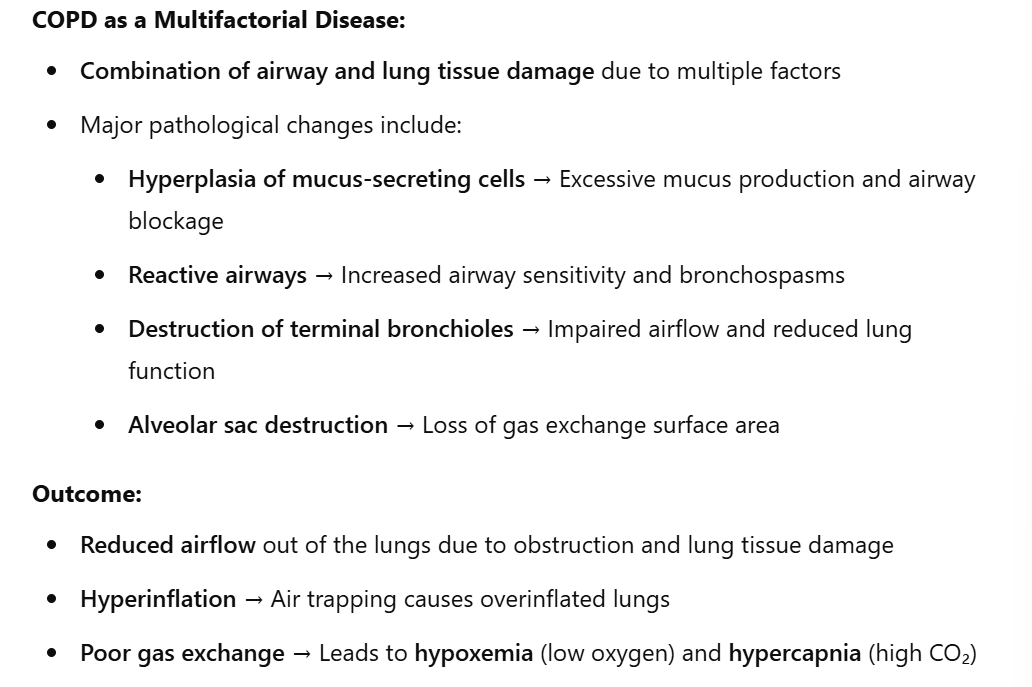
Pathophysiology (how it happens)
Inflammatory response activation:
Triggered by inhalation of harmful substances
Leads to an increase in protease and decrease in antiprotease
Protease breaks down elastin and connective tissue, causing structural damage
Long-term consequences:
Irreversible lung damage due to chronic inflammation
Increased risk of infections
Cilia dysfunction, impairing mucus clearance
Destruction of macrophages, reducing immune defense in lung tissue
Airway obstruction mechanisms:
Excessive mucus production and mucus plugging
Edema of the mucosal lining
Increased airway reactivity, leading to bronchospasms
Fibrosis and destruction of terminal airways
Lung function impairment:
Loss of elastic recoil, leading to airway collapse
Hyperinflation of lungs due to trapped air
Ventilation/perfusion (V/Q) mismatch, causing hypoxemia (low oxygen levels) → saturation?
Potential development of hypercapnia (high CO₂ levels)
2) Genetic Factors:
α1-Antitrypsin (AAT) deficiency
Affects surfactant production, reducing lung protection
Leads to early-onset emphysema, even without smoking
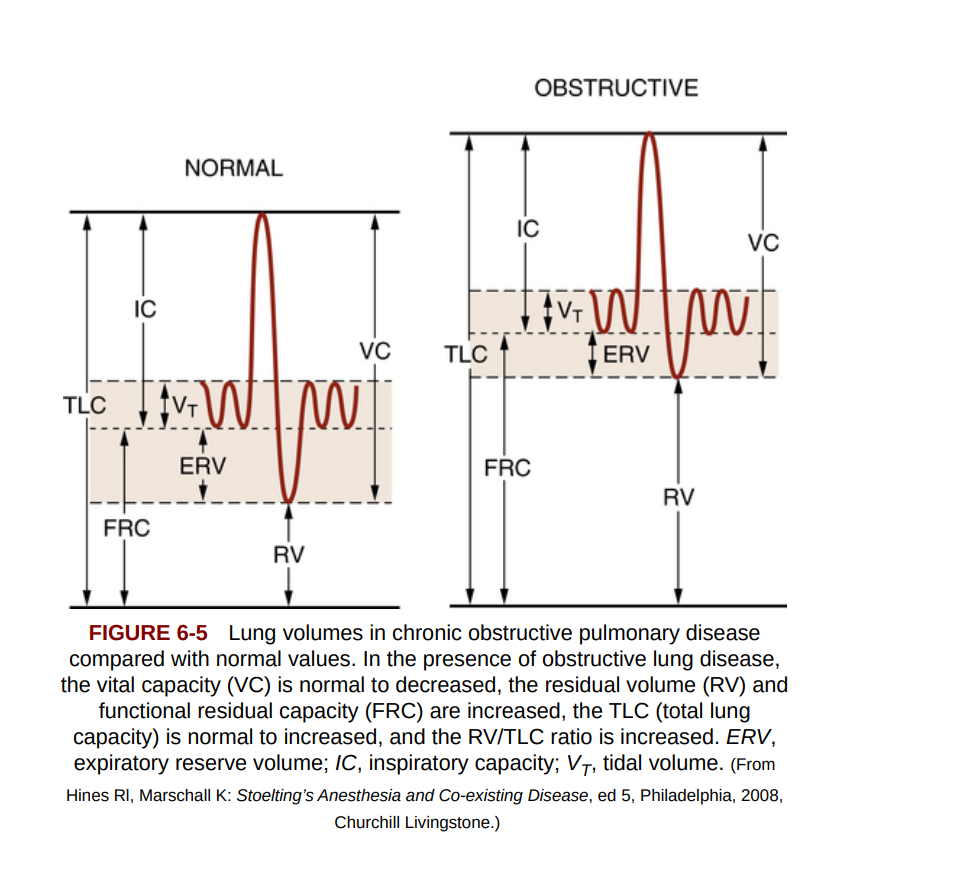
Lung Function in Obstructive Lung Disease (OLD)
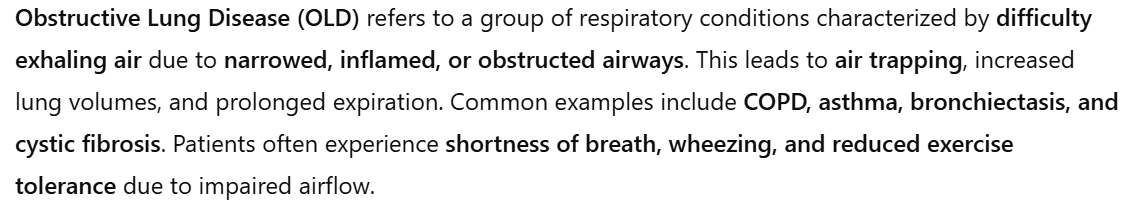
Lung Hyperinflation and Its Effects
Lung hyperinflation impacts:
The mechanical function of respiratory muscles.
Gas exchange efficiency.
Signs of OLD
Horizontal ribs
Barrel-shaped thorax (increased anteroposterior diameter)
Low, flattened diaphragms
To confirm the diagnosis, medical assessments: (do we need to ask them as physio?)
Chest X-ray
Spirometry
CT scan
Examination of arterial blood gases (e.g., oxygen saturation levels)
Symptoms
Dyspnea on exertion (DOE) – difficulty breathing during ADLs, stair climbing, or walking long distances/fast.
Increased secretion production
Chronic coughing
Anxiety (understandable, you almost dying bruh).
COPD
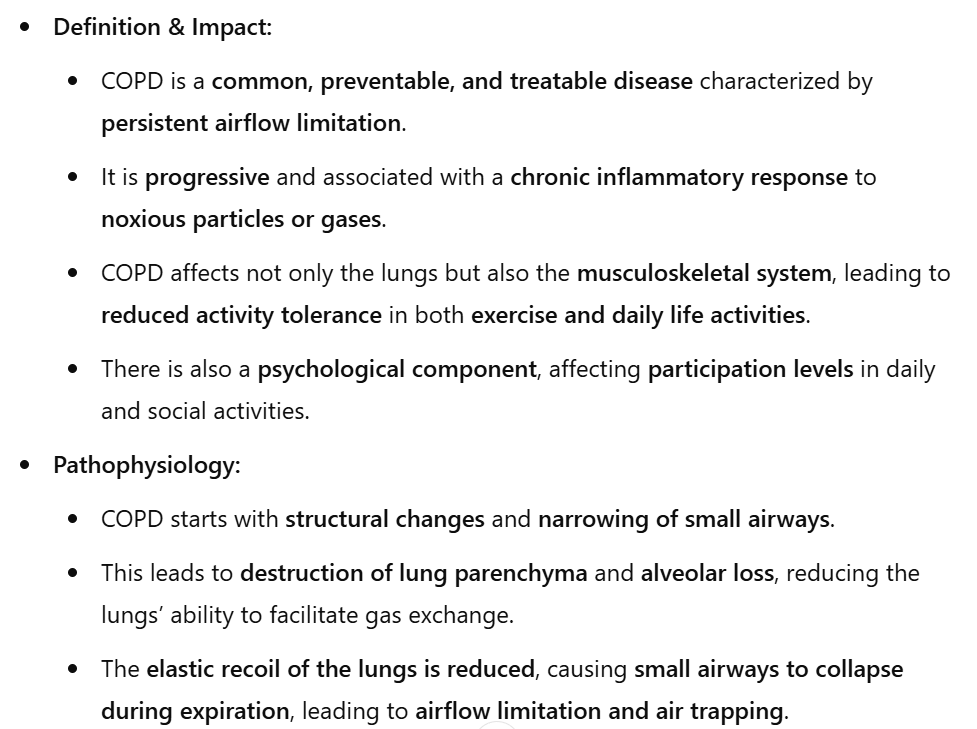
Structural Changes and Their Consequences
Loss of elastic recoil → Lung hyperinflation → Changes in the thorax, leading to a "barrel-shaped" chest.
Altered rib movement – disrupts the normal "pump-handle" and "bucket-handle" motion of the ribs.
Diaphragm flattening due to structural adaptations (loss of sarcomeres), altering its tension and impairing ventilation mechanics.
Increased intra-abdominal pressure (IAP) → Elevated pelvic floor pressure → Possible urinary incontinence.
Respiratory Muscle Adaptations
Impaired inspiration → Increased reliance on accessory muscles.
Over time, these muscles undergo hypertrophy and shortening, contributing to postural deviations.
Patients may assume a forward-leaning posture to facilitate expiration.
Skeletal Muscle Changes
Shift from Type I (endurance) to Type II (fast-twitch) muscle fibers, reducing endurance capacity.
Decline in anaerobic metabolism, affecting energy efficiency (We like breathing CO2 cause oxygen, what is oxygen)
Muscle weakness and fatigue are common due to chronic oxygen deprivation.
Psychological Aspects of COPD/ OLD
Anxiety and depression – common due to the chronic struggle to breathe.
Cognitive impairment – chronic hypoxemia (low oxygen levels) can negatively affect brain function.
Because it’s not clear, here a table with the differences between COPD, OLD and RLD
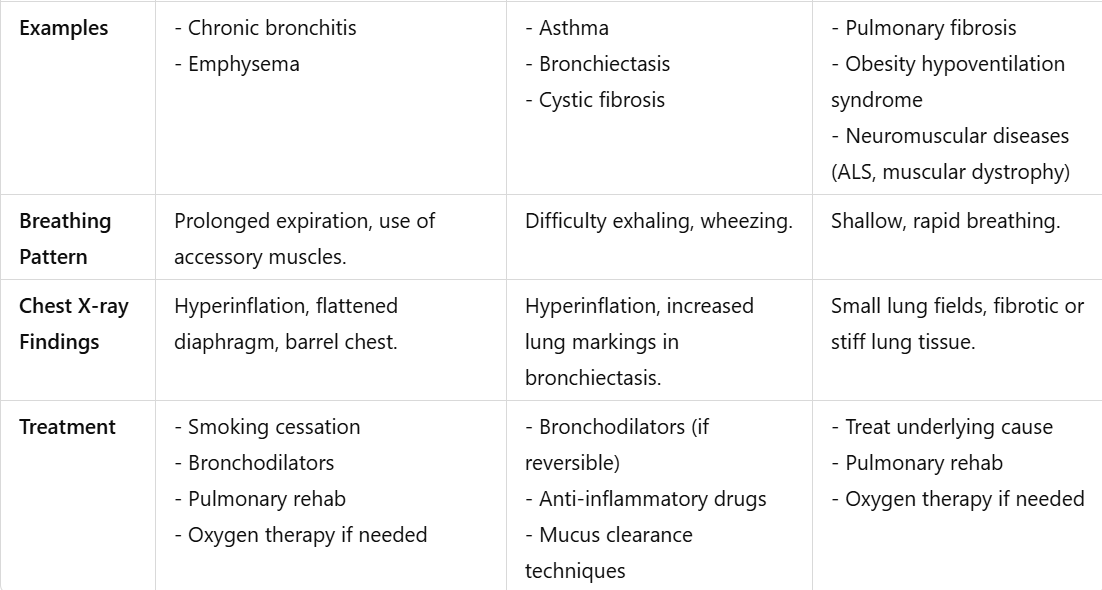
Using the values, we can express these changes between OLD and COPD
(note to self: you read from the book and the info come from there than God but you ask chat to semplify it cause wtf was that)
why?
question to ask: how deep do we need to know OLD (like we said before, it’s a group of diseases) do we have to know each one?