WK8: CNS AND ANS
TERMINOLOGIES
ACTION POTENTIAL – this is a rapid change in the membrane potential that explains how impulses are conducted along the nerves
ANXIETY – feeling of fear, tension or apprehension from known or unknown reasons
DEPRESSION – affective disorders characterized by extreme sadness, hopelessness and disorganization
MANIA – characterized by period of extreme over activity and excitement
NEUROTRANSMITTERS – chemicals in the nervous system that help in the transmission of impulses
PALLIATIVE TREATEMENT – control of signs and symptoms of the disease
PARKINSON’S DISEASE – degenerative disease of the nervous system characterized by lack of neurotransmitter called Dopamine
SCHIZOPHRENIA – most common type of psychotic disorder that may cause impairment o function of an individual I the society
SEIZURE – abnormal and excessive impulse transmission in the brain
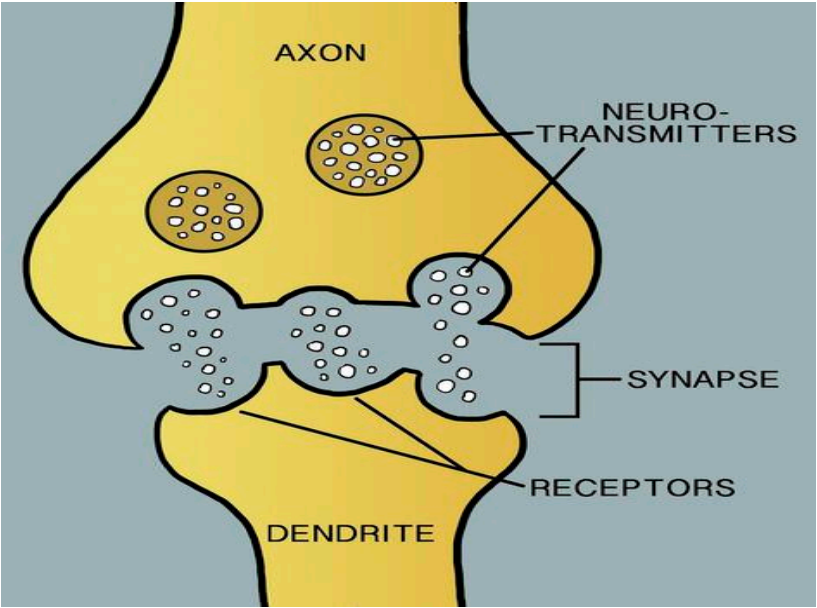
SYNAPTIC TRANSMISSION – conduction of impulses across the junction between neurons
INTRODUCTION
Drugs affecting the nervous system alter its functions. A thorough review of the anatomy and physiology of the Central Nervous System and Autonomic System would help students understand the mechanisms of actions of drugs. The functional unit, neurons basic function is impulse transmission which happen by electrical and chemical process. Electrical transmission of impulses happen by action potential and chemical process make use of neurotransmitters to achieve its functions.
CENTRAL NERVOUS SYSTEM
Brain & Spinal Cord – very important structure of the CNS is its protective mechanisms that not all chemicals can pass through it, this affects the pharmacodynamics of drugs because some of them cannot penetrate the CNS. One vital protective structure is the Blood Brain Barrier (BBB). This represents therapeutic challenge to drug treatment of brain related disorders because a large percentage of drugs are carried bound to plasma proteins and are unable to cross the brain.
PERIPHERAL NERVOUS SYSTEM
Autonomic Nervous System & Somatic Nervous System – Synapses made by the peripheral nervous system conduct impulses that is chemical in nature. These neurotransmitters have specific receptors in the neural membrane to facilitate conduction of nerve impulses. Drugs may act in the nervous system to either stimulate or block the receptors to correct alterations in the nervous functions.
Neurons conduct impulses by Action Potential, the rapid change in the membrane potential, this happens by movement of sodium into the cells causing depolarization and potassium out of the cells to cause repolarization. This movement of ions facilitated by channels in the cell membranes will be acted upon by drugs to correct changes in the nervous system causing disease process.
Classifications of Drugs Affecting the CNS
Anxiolytic and Hypnotic Drugs
Anxiety is a feeling of tension, nervousness, apprehension or fear that usually involves unpleasant reactions to a stimulus, whether actual or unknown. Anxiety is classified as mild, moderate, severe and panic. Mild anxiety is normal as it helps the person to have wider perspective and focus on certain activities but increasing anxiety may cause restlessness and increase sympathetic stress reaction which may cause physical symptoms of the sympathetic stress reactions. When anxiety becomes moderate, there is a need for drug treatment.
Sedation is the loss of awareness and reaction to environmental stimuli. Hypnosis is severe sedation. These conditions occur due to increase excitatory neurotransmitters causing rapid brain impulse conduction causing restlessness, irritability, loss of concentration, loss of mental focus and sympathetic responses like palpitations, tremors, diaphoresis, increase breathing and increase blood pressure.
Drugs for anxiety are called Anxiolytic Drugs or Sedative Hypnotic Agents
Mechanism of action – to enhance the effect of GABA (Gamma Amino Butyric Acid), an inhibitory neurotransmitter to decrease impulses in the synapses of the brain, therefore decreasing conduction of rapid impulses causing symptoms of anxiety.
Drug Classifications:
Barbiturates
drug action is to enhance GABA effect. This is used to be the drug of choice to manage anxiety but its depressant effect may cause severe respiratory depression that this is not primarily used for anxiety today.
Pharmacokinetics: Barbiturates are absorbed well, reaching the peak levels in 20 to 60 minutes. It is metabolized in the liver and excreted in the urine
Contraindications and Cautions: Barbiturates are more addicting than other anxiolytic drugs. May cause severe CNS depression and respiratory dysfunction. Contraindicated in pregnant women and clients with heaptic and renal dysfunction
Adverse Effects: CNS depression, paradoxical excitement, anxiety and hallucinations. Gastrointestinal signs and symptoms like nausea, vomiting, constipation, diarrhea and epigastric pain. Cardiovascular effects include bradycardia, hypotension and syncope
Examples: Phenobarbital, Secobarbital, Amobarbital
Benzodiazepines
drug action is to enhance GABA effect to cause inhibition of impulse transmission.
Pharmacokinetics: this is well absorbed in the GIT with peak levels achieved in 30 minutes. This is lipid soluble and well distributed in the body crossing the BBB, placenta and breast milk. Metabolized in the liver and excreted in the urine
Contraindications and Cautions: Contraindicated in Clients with allergy to benzodiazepines, psychosis, clients with acute narrow angle glaucoma, shock, acute alcohol intoxication which may exacerbate the depressant effects of the drugs. Contraindicated in pregnancy as this is known to possible cause cleft lip or palate, inguinal hernia, cardiac defects, microcephaly or pyloric stenosis if taken during the first trimester. Caution should be used in the elderly or debilitated patients an those with hepatic and renal functions
Adverse Effects: Sedation, drowsiness, depression, lethargy, anticholinergic effects like drying of mount, constipation, orthostatic hypotension, urinary retention, dysrhythmias, blood dyscrasias and phlebitis. Withdrawal syndrome may occur with abrupt cessation characterized by nausea, headache, vertigo, malaise and headache.
Examples: Diazepam, Lorazepam, Clonazepam
Non – Benzodiazepines
Other drugs used for anxiety that do not fall under Benzodiazepine
Paraldehyde
Old drug used for Delirium Tremens, seizures, absorbed and metabolize in the liver. It has a distinctive odor and cannot be stored in plastic containers
Meprobamate
An old drug used to manage anxiety for 4 months, works in the limbic system, metabolized in the liver and excreted in the urine
Chloral hydrate
Frequently used to produce nocturnal sedation or preoperative sedation. Unknown mechanism of action, absorbed in the GIT, metabolized in the liver and excreted in the urine
Zolpidem
Used to treat insomnia, Metabolized in the liver and excreted in the urine
Anti histamines – Diphenhydramine (Benadryl) Promethazine (Phenergan)
Used or its drowsiness effect in anxiety. With anticholinergic effect. Used during preoperatively or postoperatively to decrease use of narcotics
Buspirone
No sedative, anticonvulsant, or muscle relaxant properties, unknown mechanism of action, reduces anxiety without many CNS effects. Absorbed in the GIT, metabolized in the liver an excreted in the urine
Beta Blockers – Propranolol, Metoprolol
Decreasing sympathetic effect to lessen signs and symptoms of anxiety
Nursing Considerations
Do not administer intraarterially because of possible serious areriospasm and gangrene may develop
Do not mix IV drugs with other drugs
Give parenteral forms if oral forms are not feasible and switch to oral which is safer
Give IV drugs slowly to avoid hypotension effects
Promote safety measures
Monitor hepatic and kidney function
Taper dose of drugs gradually
Provide comfort measures to help patient tolerate the effects of drugs
Provide thorough health teaching about drug effects and adverse reactions
Offer support and encouragement
For overdose of Benzodiazepine, Flumazenil must be ready as its antidote.
Antidepressant Drugs
Feelings of sadness is normal and expected after a tragic event in life. This is an expected response to a stressor. Since this is a normal process, many people experiencing severe sadness may develop a depressive disorder unrecognized. People fail to distinguish normal process of grieving with a major depressive disorder. Depression being an affective disorder is recognized by its clinical manifestations such as sleep disturbances, they have little energy, inability to perform daily activity. They may describe overwhelming feelings of sadness, despair, hopelessness and disorganization.
Pharmacology explains depression by Biogenic Amine Theory. This theory explains that depression occurs due to decreasing ne feesurotransmitters, norepinephrine, serotonin and dopamine.
When impulses travel across the synapses, neurotransmitters are released into the synapse, they bind in the receptors in the post synaptic neural membrane and help impulse to be conducted. After which, neurotransmitters are removed by enzymes or they may go back to the presynaptic neuron: Refer to picture below
In the limbic system which is the area responsible for over all emotion and behavior, there are three neurotransmitters being released, Norepinephrine, Serotonin and Dopamine. After impulse is transmitted across the synapse, and enzyme called Mono Amine Oxidase will remove them. Some however may go back to the pre synaptic neuron the process called reuptake of Neurotransmitters. If they are not available in the synapse, there will be no more impulse transmission.
Let us go back to Biogenic Amine Theory which explains that depression results from decreasing neurotransmitter in the limbic system which may happen due possibly to:
Overused of neurotransmitters ( Norepinephrine, Dopamine and Serotonin)
Increase effect of Mono Amine Oxidase ( MAO ) enzyme
Increase reuptake of neurotransmitter back to presynaptic neuron
If we know the problem in the limbic system that is decreasing neurotransmitters, then we need to increase them and make them stay in the synaptic cleft. Drugs for hypertension may achieve its therapeutic effect within 2 – 4 weeks from its oral intake.
Drugs for Depression are called Anti Depressant Drugs
Mechanisms of action
Inhibit the enzyme Mono Amine Oxidase (MAO)
Inhibit Reuptake of Neurotransmitters
Drug Classifications
Tricyclic Antidepressants (TCA)
inhibit presynaptic reuptake of neurotransmitter, norepinephrine and serotonin, which leads to accumulation of these neurotransmitters in the synaptic cleft and increased stimulation of post synaptic receptors
Pharmacokinetics: it is absorbed in the gastrointestinal tract, reaching the peak in 2 to 4 hours. Widely distributed in the tissue including the brain. Metabolized in the liver and excreted in the urine. They cross the placenta and the breast milk.
Contraindications and Caution: Contraindicated to those with known allergy to TCA. Clients with recent myocardial infarction because of its cardiovascular effects. Caution should be used in clients with Gastrointestinal and Genitourinary tract disorders. The presence of hepatic and renal impairment increases toxicity of the drugs.
Adverse Effects: CNS effects like sedation, hallucinations, fatigue, cardiovascular effects, unstable blood pressure, abnormal rhythms, myocardial infarction, anticholinergic effects like drying of the mouth, constipation, urinary retention Remember Mnemonics
C – Cardiovascular effects
A – Anticholinergic effects
S – Sedation
H – Hypotension or Hypertension
Clinically important drug – drug interactions: The effects of TCA may increase if combined with Ranitidine, Fluoxetine and Cimetidine especially the anticholinergic effects. Oral anticoagulant level may increase if combined with TCA and risk for bleeding increases. Increase effect with sympathomimetic drugs especially its cardiovascular effects
Examples: Imipramine, Amitryptilline, Clomipramine
Mono Amine Oxidase Inhibitors
these drugs inactivate the enzyme MAO to increase the neurotransmitters in the synapses.
Pharmacokinetics: absorbed in the GIT, reaching peak levels in 2 – 3 hours, metabolized in the liver and excreted in the urine. They pass the placenta and breast milk and not used in pregnancy.
Contraindications and Cautions: Contraindicated in clients with cardiovascular disease, hepatic and renal disease. Caution should be used in psychiatric patients
Adverse Effects: More adverse effects than other antidepressant drugs. Dizziness, excitement, nervousness, mania, hyperfexia, tremors, confusion, insomnia, agitation and blurred vision. Liver toxicity, Cardiovascular toxicity. Anticholinergic effects
Drug – Drug interaction: Drug interaction with other antidepressant drugs include hypertensive crisis, coma and severe convulsion. A period of 6 weeks should elapse after stopping SSRI and beginning MAOI.
Drug – Food Interactions: Tyramine – rich food which normally broken down by MAO enzymes in the GIT maybe absorbed in high concentration in the presence of MAOI and may cause hypertensive crisis.
Examples: Isocarboxazid, Phenelzine, Tranylcypromine
Selective Serotonin Reuptake Inhibitors (SSRI)
these drug specifically block the reuptake of serotonin with little or no effect on Norepinephrine. SSRIs do not have the many adverse effects of TCAs and MAOIs
Indications: Depression, Obsessive Compulsive Disorders (OCD) Panic attacks, Bulemia, Post Traumatic Stress Disorder (PTSD)
Pharmacokinetics: well absorbed in the GIT, metabolized in the liver and excreted in the urine or feces. SSRIs are associated with congenital abnormalities. They passed the placenta and the breastmilk
Contraindication and Caution: Those with allergy to SSRIs, pregnancy and lactation
Adverse Effects: CNS effects like headache, drowsiness, dizziness, insomnia, anxiety, tremor, agitation and seizures. Anti cholinergic effects on the gastrointestinal tract and genitourinary tract.
Examples: Fluoxetine, Sertraline, Paroxetine
Nursing Considerations
Limit drug access to potentially suicidal patients to decrease the risk of overdose
Monitor the patient for 2 – 4 weeks to ascertain onset and full effects
Monitor blood pressure and orthostatic blood pressure carefully
Monitor liver function
Withhold medication dose in client with severe headache that may due to severe hypertension and cerbrovascular effects
Have phentolamine or another adrenergic blocker for hypertensive crisis
Provide comfort measures to help the client tolerate drug effects
Provide list of food that is low or no tyramine to clients on MAOI therapy
Offer support and encouragement to help patients cope with the disease and drug regimen
Psychotherapeutic Drugs
Mental disorders have several classifications. For this course, discussion include only drugs used for Schizophrenia and Mania, two of the most common psychiatric disorders.
Schizophrenia is the most common type of osychotic disorders. This prevents an individual in functioning in the society. Some clinical manifestations include, hallucinations, delusions, paranoia, speech abnormalities and affective problems.
Mania is associated with Bipolar illness. Mania is characterized by periods of extreme overactivity and excitement
Drugs for mental disorders are called Psychotherapeutic drugs. Drugs for Schizophrenia are called Anti Psychotic Drugs and for drugs for Mania are called Anti Manic Drugs
Antipsychotic drugs
Mechanisms of Action
Typical Antipsychotic drugs – block Dopamine receptors in the limbic system, in the reticular activating system and the brain. This group of antipsychotic may block all dopamine receptors including those not associated with psychoses
Atypical Antipsychotic drugs – block Dopamine and Serotonin receptors. This group will lock only the receptors of Dopamine and Serotinin which are responsible for occurrence of psychosis making them more specific drugs for Psychotic disorders
Drug Classifications
Typical Antipsychotic drugs: Older drugs, they are less potent and associated with more adverse effects
Examples: Chlorpro1mazine, Fluphenazine, Thioridazine, Haloperidol
Pharmacokinetics: Antipsychotic drugs are erratically absorbed in the GIT, metabolized in the liver and excreted in the bile and urine. Widely distributed in the tissues, being released up to 6 months after they are discontinued. Drugs cross the placenta and breast milk so they are not given to pregnant and lactating mothers
Contraindications and Cautions: Contraindicated in patients with Parkinson’s disease, cardiovascular disease, severe hypotension and bone marrow suppression
Adverse Effects include Anti chlinergic effects like drying of the mouthe, constipation and urinary retention, Sedation effect, Orthostatic hypotension and extra pyramidal symptoms. Remember the mnemonics ASHE. These are the most common adverse effects of antipsychotic drugs which are manifesting more in typical antipsychotic than atypical antipsychotic drugs
A – Anti cholinergic effect
S – Sedation
H – Hypotension
E – Extra pyramidal Symptoms
Parkinson’s like syndrome, Dystonia, Akathisia, Tardive dyskinesia these adverse reactions happen because of dopmaine blocking effect in the basal ganglia altering its function of coordination and fine motor function.
Other adverse effects may include respiratoy distress like laryngospasms, bronchospasms and dyspnea. Bone marrow suppresion and blood dyscrasia are seen in some patients
Nursing Considerations
Do not allow patients to crush or chew the tablet as it decreases absorption of the drugs
Monitor for orthostatic hypotennsion
Consider warning the patient or the patient’s guardian on the risk of tardive dyskinesia
Monitor CBC to check signs of bone marrow suppression
Provide positioning of legs to decrease discomfort of dyskinesia
Provide sugarless candies for drying of the mouth
Encourage the patient to void before taking the dose if urinary retention is a problem
Provide safety measures such as side rails and assistance in ambulation if there are CNS effects
Provide vison examination to determine ocular changes
Conduct thorough health teaching on the effects and adverse effects of the drugs
Offer support and encouragement to help patients cope with their drug regimen
Anti Manic Drug - LITHIUM
Mechanism of Action – Lithium alters sodium transport in the nerve and muscle, inhibit the release of norepinephrine and dopamine slightly and decreases intraneuronal content of second messengers. The last action may modulate impulses to control hyperactive state in mania
Pharmacokinetics: Lithium is absorbed in the GIT. It slowly crosses the BBB. Dehydration and sodium depletion may cause the kidneys to reabsorb more Lithim thus increasing serum levels and toxicity. Lithium crosses the palcenta and breastmilk.
Contraindications and Cautions: Contraindicated to those with allergy to the drug, dehydration, hyponatremia and leukemia
Adverse Effects: Toxicity associated with serum level of Lithium. ( Therapeutic level 0.6 – 1.2 mmol/L)
Serum level less than 1.5 mmol/L CNS problems including lethargy, slurred speech, muscle weakness, fine tremor; poluria, beginning gastric toxicity
Serum level 1.5 – 2 mmol/L Intensification of the above plus ECG changes
Serum levels of 2.0 – 2.5 mmol/LProgression of CNS symptoms to ataxia, hyperreflexia and seizure, hypotension
Serum levels more than 2.5 mmol/L complex multi organ toxicity and death
Other drugs used for Mania
Aripiprazole – atypical antipsychotic drug
Lamotrigine – anti convulsive drug
Olanzapine – atypical antipsychotic drug
Quetiapine – atypical anti psychotic drug
Nursing Considerations on administration of Lithium
Daily monitoring of lithium serum levels
Give the drug with food to alleviate GI irritation
Ensure that the patient have adequate intake of salt nd fluid
Monitor closely especially during the initial stage of therapy
Arrange for small and frequent meals with sugarless lozenges for drying of mouth
Provide safety measure like siderails and assistance with ambulation if CNS effects occur to prevent potential injury
Offer support and encouragement ot help patient cope with drug regimen
Anti – Seizure Drugs
Seizure is a collection of different syndromes characterized by abnormal and excessive impulse transmission in the brain. Seizures may be primary or secondary. Primary seizure disorder has no known cause this is often called Epilepsy. Secondary Seizure may be caused by Cerebrovascular accident, Infections, Brain Tumor, Traumatic Brain Injury, Fever and a lot more conditions that may alter impulse transmission in the brain. Seizure and Convulsion are not synonymous. Convulsion is seizure manifesting motor symptoms like tonic clonic seizure. All convulsions are seizure but not all seizures are convulsions.
Seizure is further classified into Generealized and Partial Seizure. Generalized seizure beigns in one area of the brain and rapidly spread to both hemispheres of the brain.
Examples of generalized seizure include Tonic – Clonic Seizure formerly known as Grand Mal Seizure. Partial seizures or focal seizures involve one area of the brain and do not spread throughout the entire organ. The presenting symptoms depend on exactly where the excessive electrical discharge is occurring in the brain. Samples include Partial Seizure and Complex Seizure.
The problems of seizure is excessive impulse transmission in the brain, so the action of the drug is to decrease impulse transmission, anti seizure drugs cause CNS depression.
Mechanisms of Action
Suppressing sodium influx or deporalarization in the neuron
Suppressing calcium influx, preventing electric current generated by calcium ions
Increasing the action of the Gamma Amino Butyric Acid ( GABA ) an inhibitory neurotransmitter in the brain
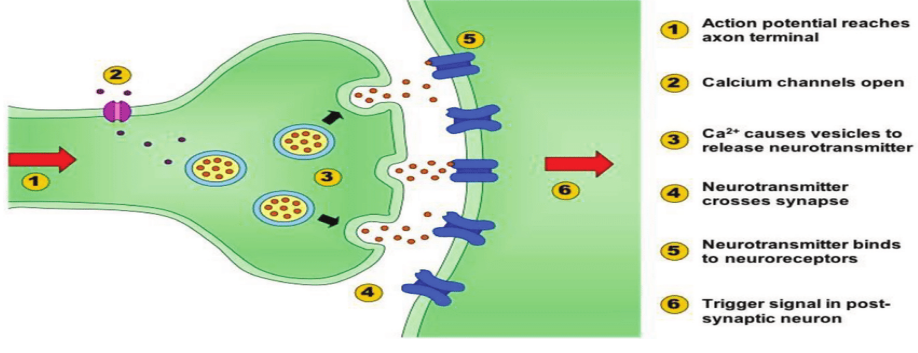
The figure shows how impulses are transmitted across the synapse. Action potential happen by sodium influx and potassium efflux, calcium channels open causing release of calcium that generate electrical activity and nurotransmitters both excitatory and inhibitory regulate impulse transmission. Excitatory neurotransmitters allow impulses to travel while inhibitory neurotransmitters stop impulses.
The mechanisms of action of anti seizure drugs occur in the neuronal synapse. Drugs for Seizures are called Anti – seizure drugs or Anti – convulsive drugs (Anticonvulsant drugs) or Anti – Epileptic Drugs.
Drug Classifications
Hydantoins
inhibit sodium influx or depolarization along the nerve fiber.
Pharmacokinetics: Hydantoinsa are absorbed in the GIT. . It is higly protein bound up to 95%. A decrease in serum albumin or proteins increases free phenytois serum levels. Average half life is 24 hour. Hydantoins are metabolized to inactive metabolites and excreted in the liver. Hydantoins are less sedating than Barbiturates and Benzodiazepines.
Adverse Effects: Neurologic and psychiatric effect which include slurred speech, confusion, depression. Low platelet count and WBC may happen and gingival hyperplasia (overgrowth of gum tissue or reddened gums that easily bleeds). Hyperglycemia and less severe adverse effcts such as nausea, vomiting, constipation, drowsiness, headache and alopecia
Drug – Drug interactions: Hydantoins must not be taken with other anti seizure drugs because it may increase its CNS depressant effects. Increase effects of Hydantoins happen in combination with Aspirin, anticoagulants, Barbiturates, Rifampicin and chronic ingestion of ethanol. Decreased Hydantoins absorption occur when combined with Antacids, calcium preparations, sucralfate and some anti cancer drugs.
Examples: Phenytoin,Fosphenytoin, Ethotoin
Barbiturates
enhanced GABA effect. These drugs are highly sedating and they may cause severe CNS depression. ( Refer to Anxiolytic Drugs for detailed discussion )
Indications: Anxiety, General Anesthesia and most commonly used for Generalized Tonic – Clonic Seizure
Benzodiazepines
enhanced GABA effect. (Refer to Anxiolytic Drugs for detailed discussion and examples)
Indications: For status epilepticus and benign febrile seizure. Diazepam is not used for long term treatment of seizure. Clonazepam is good for treatment of Petit Mal Seizure and Myoclonic Seizure
Succinimides
enhanced effect of GABA, an inhibitory neurotransmitter.
Examples: Ethosuximide the drug of choice for Petit – Mal or Absence Seizure with relative few adverse effects than other anti seizure drugs. Methosuximide
Valproate or Valproic Acid
reduces electrical acivity by suppressing calclim influx and enhancing GABA effects the drug of choice for treating myoclonic seizure
Other anti- seizure drugs
include Carbamazepine, Gabapentin, Lamotrigine, Levetiracetam. Topiramate. Some of these drugs used for partial seizure may also be used for treatment of neuropathic pain like Carbamazepine is used for treatment of Trigeminal Neuralgia.
Nursing Considerations
Administer the drug with food to alleviate GI irritations
Monitor CBC to detect possible bone marriw suppresion
Evaluate therapeutic blood level to prevent toxicity
Provide safety measures
Provide thorough health teaching, including drug name, prescribed dosage and avoidance of adverse effects
Suggest that clients wear Medic Alert Bracelet to alert health care workers about the use of anti epiletpic drugs
Offer support and encouragement to help the partient cope with the drug regimen.
Anti – Parkinson’s Drugs
Parkinson’s Disease is a degenrative disorder of the central nervous system. There is no known cause. This is common among elderly 60 years old and above. The disease is characterized by degeneration of the substantia nigra in the midbrain. A dopamine secreting neurons in the brain. Therefore there is tremendous decrease of dopamine in the brain especially affecting the basal ganglia. The basal ganglia is responsible for coordinating fine motor movement of the body. Alterations in the basal ganglia function results to lack of coordination, tremors, rigidity and bradykinesia. The neurons of the basal ganglia function normally when there is a balance between excitatory and inibitory neurotransmitters. Dopamine in the basal ganglia acts as the inhibitory neurotransmitter and Acetylcholine produced by higher neuron in the cerebral cortex act as excitatory neurotransmitter.
In Parkinson’s disease an imbalance of neurotransmitters, decreased dopamine and increased acetylcholine results to clinical manifestions causing incoordination for unconscious muscle movements including those that control position, posture and movement
Anti – Parkinson’s drugs should balance the effects of the neurotransmitters. To increase Dopamine effect and to decrease Acetylcholine effect should control symptoms of Parkinson’s Disease. These Drugs do not cure the disease but control the symptoms, hence the use is for palliative treatment.
Mechanisms of Action
1. To increase dopamine effect
2. To supress acetylcholine effect
Drug Classifications
Dopaminergic drugs
increase the effect of Dopamine at the receptor sites by increasing the levels of dopamine in the substantia nigra or directly stimulating the receptors
Pharmacokinetics: These drugs are absorbed in the GIT, metabolized in the liver and excreted in the urine. They cross the placenta and the breast milk
Contraidication and Caution: Contraindicated to clients with allergy to the drugs and glaucoma as the drug can exacerbate glaucoma. Caution should be used with any condition that could be exacerbated by dopamine receptor stimulation such as cardiovascular disease, bronchial asthma, peptic ulcer disease, urinary tract obstrution and psychiatric disorders.
Adverse Effects: CNS effects include anxiety, nervousness, headache, malaise, fatigue, confusion, mental changes, blurred vision, muscle twitching and ataxia. Peripheral effects include anorexia, nausea, vomiting, diarrhea, constipation, cardiac arrythmias, urinary retention and bone marrow suppresion
Drug – Drug interaction. Dopaminergic drugs combined with MAOI may increase hypertensive crisis. The combination of levodopa with Vitamin B6 and phenytoin and dopamine antagonists may lead to decrease effect of dopaminergic drugs.
Examples:
Levodopa – a precursor of Dopamine. Once levodopa enters the BBB, it becomes dopamine and will replace the loss od dopamine. Dopamine itself cannot pass the BBB so a precursor called Levodopa is used. When this drug was develop, there was a dramatic reduction in the signs and symptoms of Parkinson’s disease, however it was found out later that levodopa can be destroyed by and enzyme called dopa decarboxylase before they cross the BBB resulting to decreasing the level of levodopa that may cross the BBB. This is the reason why another drug is combined with levodopa. This is Carbidopa. This drug cannot increase the level of dopamine in the brain but it inhibits the enzyme, dopa decarboxylase, therefore allowing more levodopa to pass the BBB. A combination of levodopa and carbidopa (Sinemet) is still the best drug for Parkinson’s disease.
Amantadine is adrug that can increase the release of dopamine. This drug can be effective as long as there is a possibility of more dopamine release.
Bromocriptine acts a direct dopamine agonists on dopamine receptor sites in the substantia nigra.
Anticholinergic drugs
oppose the effects of acetylcholine at receptor sites in the substantia nigra. These anticholinergic drugs have greater affinity with the receptors of acetylcholine in the CNS than those in the periphery. However, they still block some receptors at the autonomic nervous sytem. Blocking the acetylcholine effect help to normalize the dopamine – acetylcholine imbalance in the basal ganglia.
Pharmacokinetics: drugs absorbed in the GIT, metabolized in the liver and excreted by cellular pathways. They pass the placenta and the breast milk
Contraindications and Cautions: Contraindicated in clients with Gastro intestinal or Genito urinary obstruction. Caution should be used in clients with cadiovascular conditions because of its blocking effect of parasympathetic nervous system
Adverse Effects: Blocking CNS actylcholine may cause disorientation, confusion and memory loss. Peripheral anticholinergic effect include drying of the mouth, constipation, urinary retention and orthostatic hypotension.
Drug – Drug interaction: These drugs should not be combined with other drugs with anti – cholinergic effects like anti – psychotic, anti – depressant drugs.
Examples: Diphenhydramine ( Benadryl ), Benztropine ( Cogentin ), Biperiden ( Akineton ) Trihexyphenidyl ( Artane ) These drugs are famous by their brand names. Most often used for treatment of Parkinson’s like syndrome, an adverse effect of anti – psychotic drugs.
Nursing Considerations
Provide sugarless lozenges to relieve drying of the mouth
Give the drugs with caution in hot weather or with exposure to hot environemtn because of increase risk for heat prostration
Give drugs with meals as they may cause GI irritation
Monitor bowel functions
Establish safety precautions
Ensure that the patient voids before taking the drugs if urinary retention is a problem
Provide thorough patient teaching about topics such as the drug name and prescribed dosage, measures help to avoid averse effects, warning signs that may indicate problems and need for pwriodic monitoring and evaluation to enhance patient knowledge about drug therapy and to promote compliance
Offer support and encouragement to help the patient cope up with the disease and drug regimen
AUTONOMIC NERVOUS SYSTEM
The division of the peripheral nervous system that supply involuntary muscles, glands and other effectors not innervated by the somatic nervous system. Autonomic nervous system is responsible for all involuntary actions of the body that the person is not aware of. This is divided into two divisions:
PARASYMPATHETIC NERVOUS SYSTEM
Parasympathetic nervous system (PNS) comes from the cranio – sacral outflow of the peripheral nervous system. Cranial nerve X, IX, VII, III participate in the cranial flow. Majority of the PNS comes from cranial nerve X ( Vagus nerve ). This is the only cranial nerves that extend up to the thorax and abdomen to supply majority of parasympathetic innervation, so a vagal stimulation is synanymous with parsympathetic innervation. Sacral nerves also participate in the PNS to supply mostly the effectors in the pelvic area like urinary bladder.
The ganglia of the PNS are located near the organ of innervation. The neurons therefore of the PNS are pre – ganglionic neuron, the neuron from the Cranio – sacral outflow to the ganglia and the post – ganglionic neuron, the neuron from the ganglia to the organ of innervations. PNS is responsible for “REST AND DIGEST” involuntary responses of the body
Impulses transmitted across the synapses of the ganglia are mediated also by the neurotransmitters.
In the PNS, the neurotransmitter is Acetylcholine. Receptors for acetylcholine are located in the post synaptic neuronal membrane. These receptors are called cholinergic receptors. There are 2 types of cholinergic receptors
Nicotinic Receptors
Muscarinic receptors
SYMPATHETIC NERVOUS SYSTEM
The division of the autonomic nervous system, Sympathetic nervous system (SNS) from the thoraco- lumbar outflow, spinal nerves from this region send nerve fibers to the sympathetic ganglia located near the CNS, then post ganglionic neurons send innervation to the involuntary muscles and glands and other effectors mostly assoicated with involuntary process in the body.
The preganglionic neuron of the SNS is shorter than PNS and the post ganglionic neuron is longer than PNS. SNS is responsile for “FIGHT OR FLIGHT” involuntary responses of the body. Impulses transmitted across the synapses also are mediated by the neurotransmitters. There are two neurotransmitters in the SNS. Actylcholine and Epinephrine and Norepinpehrine ( Catecholamines )
Actylcholine is released by the preganglionic neurons, while epinephrine and norepinephrine are the neurotransmitters released by the post ganglionic neurons, except for those post ganglionc neurons innervating adrenal medulla, pilo arector muscles, sweat glands and some smooth muscles of the blood vessels, they have sympathetic innervations but the neurotransmitter in at the postganglionic neurons is Acetylcholine
Epinephrine and Norepinephrine may also be called Adrenalin and Noradrenaline respectively or they are being refered to as catecholamines. Their receptors are called Adrenergic Receptors.
There are 2 types of adrenergic receptors
1. Alpha receptors
2. Beta receptors
Drugs affecting the Autonomic Nervous System are called Autonomic Drugs
Classifications of Autonomic Drugs
Drugs affecting the PNS are called Cholinergic
Drugs Drugs affecting the SNS are called Adrenergic Drugs
In the study of pharmacodynamics, one action of the drugs is its binding with the receptors that may stimulate the receptors (drugs are called agonist) and drugs that may block the receptors (drugs are called antagonists). If a student is aware of the responses of the PNS and SNS, it would be easier to remember drug actions, they would either stimulate the receptors and produce the same effect or block the receptors or inhibit the effects.
Most of the effectors are innervated by both sympathetic and parasympathetic and in such case the response of the body is opposite. See examples below:
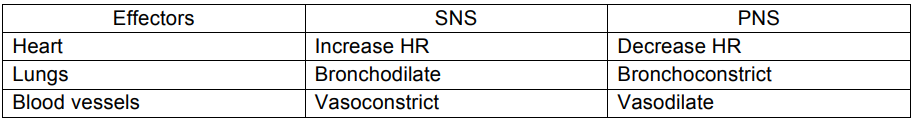
Therefore, if a drug stimulates the receptors for PNS, it is called cholinergic agonist, enhancing PNS effect so such drug is also referred to as parasympathomimetic drug. A drug that blocks the cholinergic receptors is called cholinergic antagonist, also called anticholinergic drugs, inhibiting PNS response and such drug may also be referred to as parasympatholytic drug
If a drug stimulates receptors for SNS, it is called adrenergic agonist, increasing SNS effect so such drug is also referred to as sympathomimetic drugs. A drug that blocks the adrenergic receptors decreases SNS responses called adrenergic agonist or it is also called sympatholytic drugs.
Remember, knowing the responses of the PNS and SNS is very important to understand actions of autonomic drugs, because these drugs would only stimulate or block the receptors.
Cholinergic Agonist drugs
majority of these drugs affect the PNS
Direct acting cholinergic agonist
directly stimulates the cholinergic receptors to increase its effects
Pharmacokinetics: well absorbed with relatively short half – life. Metabolism and excretion may occur at the synaptic level but exact mechanism is unknown
Contraindications and Cautions: These drugs enhance parasympathetic effect so must not be given to patients with hypotension, bradycardia or heart block, intestinal obstruction and urinary retention.
Adverse effects: These are related to increase parasympathetic responses such as bradycardia, diarrhea, urinary incontinence. Increase sweating may happen because of the acetylcholine present in the sweat glands.
Drug – Drug interaction: Effects of these drugs maybe increase if combined with anticholinesterase drugs or the indirect acting cholinergic agonists.
Examples
Bethanecol – indicated for non – obstructive urinary retention like in neurogenic bladder
Carbachol – indicated for glaucoma, causing pupillary constriction
Pilocarpine – indicated for glaucoma, causing pupillary constriction
Indirect acting cholinergic agonist
this drug increases acetylcholine effect by inhibiting the action of acetylcholinesterase (an enzyme that removes acetylcholine in the synapse. If acetylcholinesterase is not removed in the synaptic cleft, more acetylcholine stays in the synapse stimulating more receptors, thus enhancing their effects. These drugs are used for treatment of Myasthenia gravis and Alzheimer’s disease
Myasthenia gravis is an autoimmune disease of the neuromuscular junction (NMJ). This is characterized by destruction of cholinergic receptors at the NMJ that will slow down impulses going to the skeletal muscles. This disease is characterized by the development of muscle weakness and paralysis. To increase junctional transmission, indirect acting cholinergic agonist inhibits acetylcholinesterase making more acetylcholine present in the junction to improve impulse transmission and muscle function. These drugs are also called anticholinesterase drugs.
Anticholinesterase drugs for Myasthenia gravis include:
Edrophonium HCL (Tensilon) – short acting anticholinesterase drug used to diagnose the disease. The action lasts for 10 to 20 minutes.
Neostigmine, Physostigmine, Pyridostigmine – long acting anticholinesterase drugs used for therapeutic purposes. The onset of action starts 20 to 30 minutes and may last for 3 – 6 hours.
Alzheimer’s Disease is a degenerative disease of the CNS characterized by loss of neurons in the CNS which may slow down impulse transmission across the synapses of the CNS. One important cause of this is explained by loss of acetylcholine receptors in the post synaptic neurons, like myasthenia gravis, less receptors mean lesser impulse transmission. So anticholinesterase drugs that inhibit acetylcholinesterase enzyme will increase acetylcholine effect and promote impulse transmission in the CNS. Can drugs for myasthenia gravis be used to patients with Alzheimer’s disease? The answer is no simply because those drugs cannot pass the BBB. Therefore, Alzheimer’s disease will have its own anticholinesterase drugs.
Acetylcholinesterase drugs used for Alzheimer’s disease are called Anti Alzheimer’s drugs which include
Rivastigmine
Donepezil
Tacrine
Pharmacokinetics: These drugs are well absorbed and distributed in the body. Drugs for myasthenia do not pass the BBB. The drugs are metabolized in the liver and excreted in the urine
Contraindications and Cautions: The drugs are not given to those with known allergy to the drugs. The drugs may exacerbate bradycardia, diarrhea and urinary incontinence
Adverse effects: Exacerbation of parasympathetic effects may be seen in the patient such as bradycardia, hypotension and incontinence
Nursing Considerations
Properly administer eye medication
Slow IV administration to avoid severe cholinergic effects
Cholinergic agonist oral preparation must be taken with an empty stomach to decrease nausea and vomiting
Closely monitor vital signs and exacerbation of parasympathetic effects
Provide safety measures
Monitor patients with Alzeimer’s disease for progression of the disease. Drugs will not cure the disease
Monitor patients with Myasthenia gravis for underside or overdose of medication
Provide health teaching on the name of drugs, its action and adverse effects to promote client’s understanding and compliance
Provide emotional support and encouragement to help the patient cope with drug regimen
Cholinergic antagonist
also being referred to as anticholinergic drug or parasympatholytic. The drugs act to block the cholinergic receptors in the PNS. The drugs may also block some cholinergic receptors present in the SNS
Pharmacokinetics: The drugs are well absorbed and distributed. Drugs pass the BBB, placenta and breastmilk. The drugs are excreted in the urine.
Contraindications and Cautions: The drugs are not given to patients with known allergy to the drugs. Should not be used in clients with cardiovascular, gastrointestinal or genitourinary conditions because they may exacerbate anticholinergic effect add worsen the conditions. Contraindicated in client with glaucoma as the drug may cause pupillary dilation and further increase intraocular pressure. Caution is used to patients with hepatic or urinary impairment.
Adverse effects: These are associated with anticholinergic effects of drugs such as drying o the mouth, constipation, urinary retention, tachycardia, mydriasis. Drowsiness, confusion and insomnia are all related to the CNS effects of anticholinergic drugs
Examples:
Atropine – indicated to decrease secretions, treat bradycardia, pylorospams, ureteral colic, cause pupil dilation (mydriasis) indicated as preop drug for cataract extraction. Use as antidote for cholinergic crisis
Dicyclomine – use for hyperactive bowel in adults
Scopolamine – use in motion sickness, indicated to decrease secretion, pupil dilation
Adrenergic Agonist drugs
these drugs act to either stimulate or block the adrenergic receptors in the SNS
Adrenergic agonist – stimulate the receptors to increase sympathetic effect and is also referred to as sympathomimetic drugs
Adrenergic antagonist – block the receptors to decrease sympathetic effect and is also referred to as sympatholytic drugs
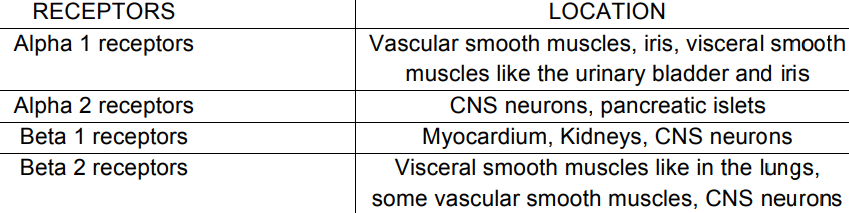
Adrenergic receptors have 2 types and subtypes. Classification is based on their actual locations in the body. Below are some adrenergic receptor sites and their specific locations in the body
Types of the Adrenergic Receptors
1. Alpha receptors
a. Alpha 1 receptors
b. Alpha 2 receptors
2. Beta receptor
a. Beta 1 receptors
b. Beta 2 receptors
Study the table below for some important locations of the receptors
For the sake of the discussion and the given examples of drugs, the effects of some of drugs in particular receptors will be discussed first.
Alpha 1 receptors when stimulated will cause vasoconstriction, pupillary dilation and closure of urinary bladder sphincter causing urinary retention. When the receptors are block? What would be the expected effects?
Alpha 2 receptors in the CNS neurons when stimulated will decrease norepinephrine flow from the CNS to the SNS therefore decreasing sympathetic response. Take note that this is the drug that stimulate adrenergic receptors but decreasing SNS effect because the receptors being stimulated are located in the CNS.
Beta 1 receptors in the heart when stimulated will increase heart rate. When we use a drug that blocks the receptor, what is the effect?
Beta 2 are located in the lungs, if we use a drug that stimulates receptors, the effect is bronchodilation, what is the effect if we block the receptor?
Alpha and Beta adrenergic drugs ( Sympathomimetic drugs )
these drugs stimulate all adrenergic receptors to enhance their effects
Pharmacokinetics: these drugs are rapidly absorbed, metabolized in the liver and excreted in the urine. These drugs may cross the placenta and breastmilk
Contraindications and Cautions: Should not be given in client with allergy to these drugs and to patients with pheochromocytoma as the drugs may exacerbate the signs and symptoms
Adverse effects: These are all related to increase SNS response like tachycardia, hypertension, constipation, urinary retention, pupillary dilation
Examples
Epinephrine – the drug of choice during CPR, indicated for treatment of shock
Dobutamine – used for treatment of congestive heart failure
Dopamine – usually given for congestive heart failure and cardiogenic shock
Norepinephrine – like epinephrine, may be indicated for cardiac arrest
Alpha specific adrenergic agonist
these drugs specifically stimulate only the alpha receptors and not the beta receptors
Pharmacokinetics: these drugs are well absorbed and distributed, reach peak levels in 20 to 45 minutes. These drugs are metabolized in the liver and excreted in the urine
Contraindications and Cautions: these drugs are not indicated to clients with allergy to the drugs, those with hypertension and close angle glaucoma. Caution is used in clients with cardiovascular disease.
Adverse effects: these are related to the overdose of drugs that may increase sympathetic effects like hypertension, gastrointestinal depression and genitourinary effects like urinary retention
Examples
Alpha 1 adrenergic agonist – Phenylephrine used for treatment of common colds and allergy. This drug causes vasoconstriction to lessen congestion in the nose therefore called decongestants.
Alpha 2 adrenergic agonist – Clonidine better known for its brand name as Catapres acting on the CNS neurons to decrease norepinephrine flow. This drug is indicated for treatment of hypertension.
Beta specific adrenergic agonist
these drugs specifically stimulate the beta receptors and not the alpha receptors.
Pharmacokinetics: well absorbed and distributed in the body, metabolized in the liver and excreted in the urine. The drugs pass the placenta and breastmilk, use in pregnancy and lactation only if benefits outweigh the risks
Contraindications and Cautions: The drugs are contraindicated in clients with allergy to the drugs. Caution is used in clients with cardiovascular disease like hypertension and tachycardia.
Adverse effects: These are related to the primary effects of drugs which will increase sympathetic effects like hypertension and tachycardia.
Examples
Isoproterenol – for treatment of cardiogenic shock and heartblock in transplanted heart.
Salbutamol – for treatment of obstructive respiratory disease like COPD and bronchial asthma
Nursing Considerations
Avoid sudden withdrawal of the drug because it may cause rebound hypertension, arrhythmias and flushing
Monitor vital signs especially blood pressure and heart rate
Avoid comfort measures including rest and environmental control to decrease CNS irritation
Provide adequate health teaching on the name of drug, prescribed dosage, effects and adverse effects to increase patient’s knowledge and subsequent compliance.
Adrenergic Antagonist Drugs (Sympatholytic drugs)
Alpha and Beta adrenergic antagonist
these drugs block all adrenergic receptors
Pharmacokinetics: these drugs are well absorbed and distributed in the body, metabolized in the liver and excreted in the urine and the feces.
Contraindications and Cautions: These drugs should not be given to clients with allergy to the drugs. To those with hypotension and bradycardia. Caution is used in clients with cardiovascular disease and obstructive lung disorder
Adverse effects: these mainly on the effects of the drugs in the lungs like bronchospasm, blood vessels causing vasodilation and hypotension.
Examples
Carvedilol
Labetalol
Both examples maybe indicated to clients with severe hypertension caused by pheochromocytoma
Alpha adrenergic antagonist
these drugs block only the alpha receptors, specific drugs act on the alpha 1 and alpha 2 receptors.
Pharmacokinetics: these drugs are well absorbed and distributed, metabolized in the liver and excreted in the urine.
Contraindications and Cautions: The drugs should not be given to clients with hypotension and urinary incontinence
Adverse effects: related to the primary action of the drug causing vasodilation and hypotension
Example
Phentolamine – more specific drug hypertension in pheochromocytoma, that will have less adverse effects
Alpha 1 selective adrenergic antagonist
these drugs block only the alpha receptors, specific drugs act on the alpha receptors on the blood vessels and urinary bladder to case vasodilation for treatment of hypertension and bladder emptying for treatment of urinary retention. Although some drugs may act in both blood vessels and urinary bladder at the same time
Pharmacokinetics: drugs are absorbed in the GIT, metabolized in the liver and excreted in the urine.
Contraindications and Cautions: Contraindicated in clients with allergy to the drugs. This may exacerbate hypotension and urinary incontinence. Caution is used to clients with cardiovascular disease, gastrointestinal and genitourinary conditions
Adverse effects: related to the sympatholytic effect of drugs causing hypotension and urinary incontinence.
Examples
Prazosin – indicated for treatment of hypertension
Terazosin – indicated for treatment of hypertension and BPH causing urinary retention
Doxazosin – indicated for treatment of hypertension and BPH causing urinary retention
Alfuzosin indicated for treatment of BPH
Tamsulosin – indicated for treatment of BPH
Beta adrenergic antagonists
these drugs block both beta 1 and beta 2 receptors, particularly affecting both the heart and the lungs, these drugs increase heart rate and bronchoconstriction of the lungs
Beta 1 specific adrenergic antagonist
these drugs block specifically beta 1 receptors in the heart. These drugs are most commonly known as beta blockers. These drugs are indicated to clients with hypertension, dysrhythmias, angina and use to support cardiac function in clients with congestive heart failure
Pharmacokinetics: these drugs are absorbed in the gastrointestinal tract and undergo hepatic metabolism. The presence of food may increase the bioavailability of some beta blockers. These drugs are known teratogenic in animals as it passes the placenta and breast milk
Contraindications and Cautions: Contraindicated in clients with allergy to the drugs. Caution should be used in clients with bradycardia and heart block as well on patients with obstructive lung diseases like COPD and bronchial asthma
Adverse effects: these are related to the bradycardia and bronchoconstriction effect of the drug. Gastrointestinal effects like nausea and vomiting, genitourinary symptoms may be disturbing to clients as well.
Examples
Beta adrenergic antagonists or Beta blockers
Propranolol
Pindolol
Beta 1 specific adrenergic antagonists or Beta 1 blockers
Metoprolol
Atenolo
Nursing considerations
Avoid sudden withdrawal of the drug because it may cause rebound hypertension, arrhythmias and flushing
Monitor vital signs especially blood pressure and heart rate
Monitor ECG
Avoid comfort measures including rest and environmental control to decrease CNS irritation.
Provide adequate health teaching on the name of drug, prescribed dosage, effects and adverse effects to increase patient’s knowledge and subsequent compliance.