Book Notes | The Heart
19.1 Overview
The cardiovascular system consists of the heart and blood vessels
Arteries carries blood away from the heart-efferent vessels
Veins carry it toward the heart-afferent vessels
Capillaries are microscopic vessels that connect the smallest arteries to the smallest veins
The Pulmonary and Systemic Circuits
Pulmonary circuit carries blood to lungs for gas exchange and returns it to the heart
The right half of the heart supplies the pulmonary circuit
Pumps oxygen poor (deoxygenated) blood into a large artery, the pulmonary trunk, which immediately divides into right and left pulmonary arteries
These transport blood to air sacs (alveoli) of the lungs, where CO2 is unloaded and O2 is picked up
The oxygenated blood flows by way of pulmonary veins to the left side of the heart
Systemic circuit supplies blood to every organ of the body, including parts of the lungs and the wall of the heart
The left side of the heart supplies the systemic circuit, blood leaves by the Aorta.
The aorta turns like an inverted U, the aortic arch, and passes downward posterior to the heart
The aorta travels through the thoracic and abdominal cavities and issues smaller arteries to the other organs before branching into the lower limbs
After circulating through the body & unloading O2, deoxygenated systemic blood returns to the right side of the heart mainly by two large veins: The superior vena cava (draining the upper body) and inferior vena cava (draining everything below the diaphragm)
Normally the pressure in the pulmonary circuit is less than the systemic circuit
A shunt us an abnormal, non capillary connection btw the two circuits
Position, Size, & Shape of Heart
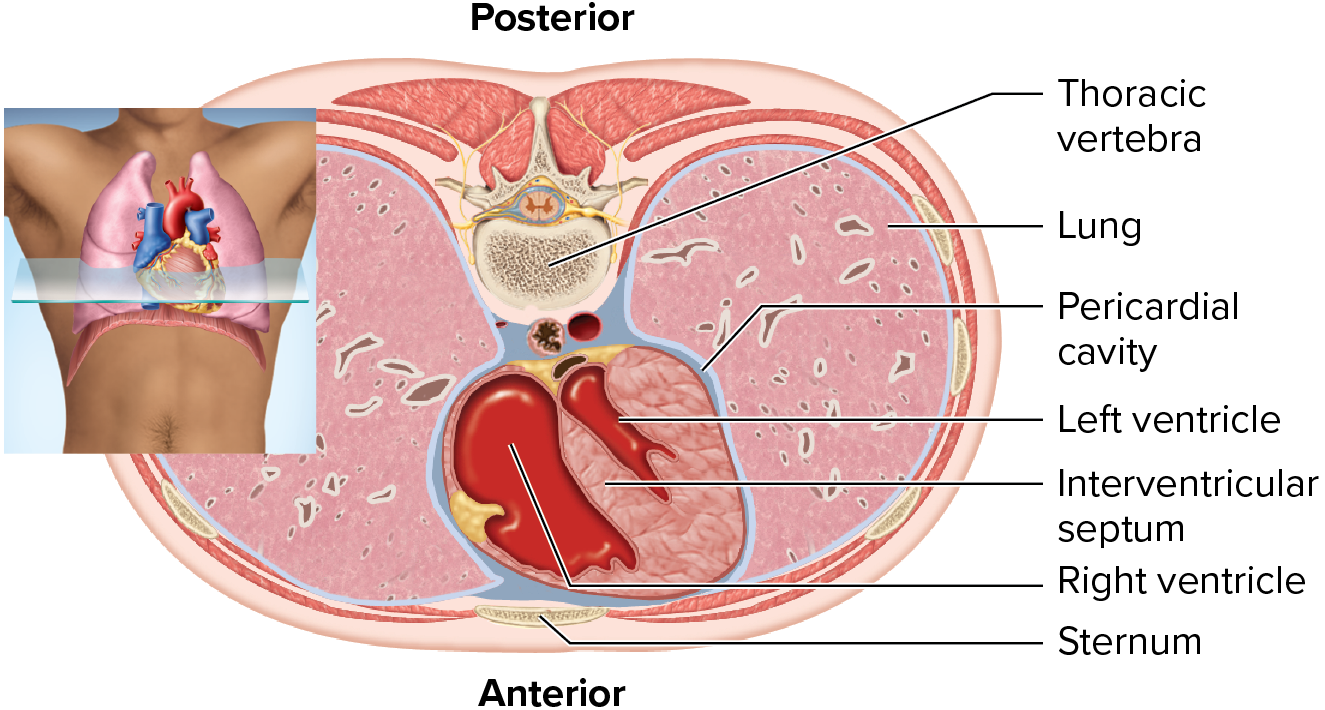
The heart lies btw the two thoracic cavities in an area called the mediastinum
Buffalo’s do not have a mediastinum, therefore easy to kill
It is triangular shaped, with the broad base lying superiorly
The apex is pointed inferiorly and somewhat to the left
It is roughly the size of a fist
it weight about 300 g in an adult

The Pericardium
The heart lies in a sac called the pericardium
It is a two layered structure, an outer fibrous layer and an inner serous layer
The fibrous layer is attached to the diaphragm
The serous side is a single squamous layer of cells, that secrete and absorb pericardial fluid. It also covers the surface of the heart called the epicardium
The space btw the parietal and visceral layers of the serous pericardium
is called the pericardial cavity
The layer is called the visceral layer of the pericardium, the layer under the fibrous pericardium is the parietal layer
The space btw the two layers is the pericardial sac, containing 5 to 30 ml of pericardial fluid
too much fluid is cardiac tamponade
19.2 Gross Anatomy of the Heart
The Heart Wall
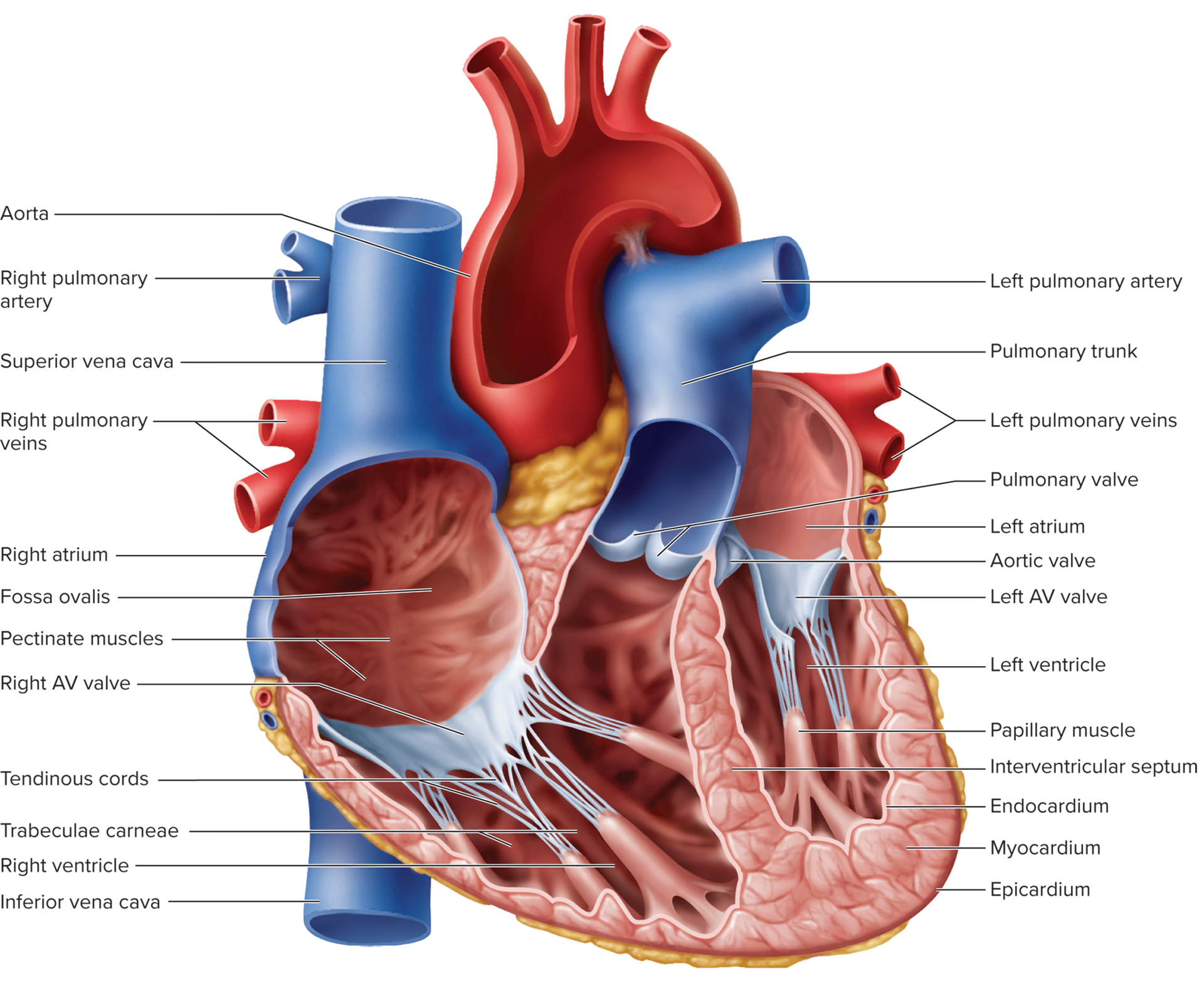
Consists of three layers: epicardium, myocardium, and endocardium
Epicardium
outermost layer, visceral layer of serous pericardium
some places, it includes a thick layer of adipose tissue that encloses the major coronary blood vessels and protects them from compression
Endocardium
lines the interior of the heart chambers
simple squamous epithelium overlying a thin areolar tissue layer
covers the valve surfaces and is continuous with the endothelium of the blood vessles
Myocardium
composed of cardiac muscle
thickest layer and performs the work of the heart
forms the vortex of the heart
when the ventricles contract, they exhibit a twisting or wringing motion that enhances the ejection of blood
Has a framework of collagenous elastic fibers that make up the fibrous skeleton
developed in fibrous rings around valves and in the sheets that connect the rings


The Chambers
4 chambers of the heart, 2 atria superiorly, and 2 ventricles below them inferiorly
Each atrium has a small flap called an auricle
The walls of the atria are thin due to their low-pressure workload
Each atrium is separated from the other by an interatrial septum
The right and left ventricles are thicker than the atrial walls, the left ventricular walls are thicker than the right
The LV is the circular in cross section whereas the right ventricle has a crescent shape
The two inferior chambers, right & left, are the pumps that eject blood into the arteries and keep it flowing around the body
Ventricles separated by a thick muscular wall, the interventricular septum
Both ventricles exhibit ridges called trabeculae carneae
Three sulci of the heart
The coronary sulcus encircles the heart near the base and separates the atria above from the ventricles below
The other two extend obliquely down the heart from the coronary sulcus toward the apex - one on the front called the anterior interventricular sulcus and one on the back called the posterior interventricular sulcus
The Valves
Each valve consists of fibrous flaps of tissues called cusps or leaflets, covered with endocardium
The Tricuspid valve (will be used more often) or right AV regulate openings btw the atria and ventricles
The mitral valve or left AV is considered inaccurate and obsolete
Tendinous cords prevent the the AV valves from flipping inside out or bulging into the atria when the ventricles contract
The semilunar valves regulate the flow of blood from the ventricles into the great arteries
The pulmonary valve controls the opening from the Tricuspid valve into the pulmonary trunk
The aortic valve controls the opening from the left ventricle into the aorta

Blood Flow Through the Chambers

Coronary Circulation
Blood vessels of the heart wall constitute the coronary circulation
the coronary
19.4 Electrical and Contractile Activity of the Heat
Contraction is called systole
Relaxation is a diastole
The Cardiac Rhythm
Triggered by the SA node
Sinus Rhythm - normal heartbeat
Spontaneous firing of the SA node is called ectopic focus
slower heart beat of 40 to 50 bp, is called a nodal (junctional) rhythm
Pacemaker Physiology
pacemaker potential - showing a gradual depolarization
Impulse Conduction to the Myocardium
firing of the SA node excitres atrial cardiomyocytes
AV slows the signal down to about 0.05 m/s bc cardiomyocytes here are thinner
Delays AV node for about 100 ms - allowing the ventricles time to fill with blood before they begin to contract
Ventricular systole begins at the apex of the heart
The EKG
P wave - atrial depolarization - produced when a signal from the SA node spreads
QRS complex - Ventricular depolarization - when the signal from the AV node spreads through the ventricular myocardium ad depolarized the muscle
T wave - Ventricular repolarization -
QT interval - duration of ventricular depolarization; shorter during exercise
QRS interval - atrial repolarization and diastole; repolarization concealed by QRS wave
PQ segment - signal conduction from SA node to AV node; atrial systole begins
ST segment ventricular systole and ejection of blood; corresponds to plateau of cardiomyocyte action potential
Any deviation from the regular is called an arrhythmia
V-fib is the major sign of a heart attack
Heart block, lack of QRS behind the P wave.
Bundle branch block is a heart block resulting from damage to one or both branches of the AV bundle
PVC - premature ventricular contraction - ventricular ectopic focus firing and setting off an extra beat (extrasystole)
Sinus Rhythm - normal
V-fib - heart rhythm is going nuts - makes ‘v"‘
A fib - irregular, weak ripping contraction in the atria
Heart Block - lack of QRS following p waves
PVC - irregular “v” in the EKG
19.5 Blood Flow, Heart Sounds, and the Cardiac Cycle
Measurement Of Pressure
Blood pressure specifically has been traditionally measured with sphygmomanometer
A fluid flows only if it is subjected to more pressure at on appoint than another - the difference is a pressure gradient
Pressure gradient - fluids always flow down their pressure gradients, from high pressure point to low pressure point
Volume and pressure have an inverse relationship
AV valve is open, blood flows into the ventricle from the above atrium
The ventricle contracts, its internal pressure arises
When the ventricles are relaxed and their pressure is low, the AV valve cusps hang down limply and both valves are open
Lub-dub
Lub S1 and Dubb S2
S1 louder and longer
S2 a little softer and sharper
Third Heart Sound
rarely audible, triple rhythm or gallop
Phases of the Cardiac Cycle
Wiggers Diagram
major events that occur simultaneously at each moment throughout the cardiac cycle
Ejection Fraction: the percentage of blood ejected during ventricular systole, the percentage of the vend-diastolic volume in the ventricles
Stroke Volume: the actual volume of the ejection fraction
End Diastolic volume: total volume of blood in the ventricle at the end of the ventricular filing..the end of the diastole
Normal ejection fraction-around 55-60%
End systolic volume 60 ml
volume during atrial diastole + 30 ml
volume during atrial kick + 40 ml
Total end-diastolic volume 130 ml
stroke volume - 70 ml
End systolic volume 60 ml
Both ventricles have equal volumes
BP in the right ventricle is relatively low
Equal ooutput by the two ventricles is essential for homeostasis
If the right ventricle pumps more blood into the lungs then the left ventricle can can handle on return, blood accumulates in the lungs, causing pulmonary hypertension, edema, and risk of drowning in one’s own body fluid
CHF - congestive heart failure - insufficiency of ventricular pumping
19.6 Regulation of Cardiac Output
Autonomic Innervation of the heart
Sympathetic stimulation increases heart rate, contraction strength, and dilates coronary arteries
There is little to no parasympathetic innervation of the myocardium or ventricles
Cardiac Output
CO = HR x SV
Difference btw the maximum and resting cardiac output is called cardiac reserve
Magic 5 liters - max at rest
Heart Rate and Chronotropic Agents
Avg. adult female HR is 72-80bpm
Avg. adult male HR is 64-72bpm
tacycardia & bardycardia
Positive chronotropic - factors outside of the heart itself that raise the heart rate
Negative chronotropic agents lower the heart rate
Adrenergic stimulation increases heart rate by increases SA node firing through stimulation with catecholamines, epi and norepi
Cholergenic stimulation stimulation from the Vagus nerve slows the heartbeat, secrete acetylcholine at the SA and AV nodes, opens k+ channels, hyper-polarize these nodes and the heart slows down
Central Nervous System
propioceptors in the muscles and joints provide information changes in physical activity. Thus, the heart can increase its output even before the metabolic demands of the muscles rise.
Baroceptors
pressure sensors in the aorta and internal carotid arteries
HR increases, cardiac output increases and raises bp
signals to medulla to raise or lower BP
Chemoreceptors
occur in the aortic arch, carotid arteries, and the medulla oblongata
sensitive to pH, CO2, and O2 lvls
Hypercapnia - excess CO2
Acidosis - pH greater than 7.35
Hypoxemia - O2 deficiency
hormones, drugs, and other chronotropic chemicals
Increased HR
positive chronotropic agents
sympathetic nervous system
epi, norepi
TH
glucagon
Nicotiene, caffeine
Hypocalcemia
Increased stroke volume
Increased preload (myocardial stretch)
Positive inotropic agents
Sympathetic nervous system
glucagon digitalis
nicotine, caffeine
Hypercalcemia
Reduced Heart Rate
Negative chronotropic agetns
parasympathetic nervous system
acteycholine
hypercalcemia
HyperK
Beta blockers
Reduced stroke volume
reduced preload
reduced contracility
increased afterload
negative inotropic agents - changes force of contraction
Hypocalcemia
HyperK
More Definitions
preload: amount of stretch prior to contraction, increased preload, up to a point
frank-starling relationship - stroke volume is proportional to the end diastolic volume
contractility - how hard the myocardium contracts for any given level of preload
Positive inotropic agents increase contractility
negative inotropic agents decrease contractility
calcium is a positive inotropic agents
hyperK is a negative inotropic agent
digitalis increases intercellular calcium, making it a positive inotropic agents decrease contractility
afterload - the sum of the forces the ventricle must overcome to to eject blood
increased blood pressure is an increase in the afterload, anything that impedes the flow of blood increases the afterload