ENDO 11 SUMMARY?
Hello to anyone that may be reading this, this does NOT include all info. Just stuff I thought was important + did not know already. I’d suggest to read the slides afterwards cus I skipped most of the diagrams HAHAHA
SELF MONITORING BLOOD GLUCOSE = FOR DUM DUMS. (It’s not really required to do as much as people think they need to)
Diagnosing Diabetes 🩸
How we diagnose diabetes:
FPG ≥7.0, A1C ≥6.5%, 2hPG (OGTT) ≥11.1, or RPG ≥11.1
If symptomatic → Only one test needed!
If no symptoms → Confirm with a second test!
If NO symptoms:
Repeat the test on a different day to confirm.
If using different tests (e.g., one A1C and one FPG), and both are above the cutoff → diagnosis confirmed.
🔹 If symptoms ARE present (thirst, urination, weight loss, etc.):
Diagnosis is confirmed immediately—no second test needed!
🚨 For suspected Type 1 diabetes (especially in young, thin, or very symptomatic patients), treatment should start immediately—DO NOT delay for confirmatory tests!
A1C – The Gold Standard for Diabetes Control 🎯
🔹 What is A1C?
Measures the % of hemoglobin (HbA1c) bound to glucose in red blood cells.
Reflects average blood sugar over the past 3 months.
📌 A1C is a ‘surrogate marker’ for complications: Lower A1C → Lower risk of diabetes complications!
A1C = Long-term diabetes control marker
Pros: No fasting, every 3-6 months
Cons: Doesn’t show daily swings, affected by some conditions
🔹 A1C in a person WITHOUT diabetes? 4.5-5.9%
🔹 Targets for people WITH diabetes:
A1C Target | Who is it for? |
|---|---|
≤6.5% | T2DM patients at low risk of hypoglycemia (to reduce CKD & retinopathy risk) |
≤7.0% | Most adults with Type 1 or Type 2 diabetes |
7.1-8.0% | Functionally dependent patients (older adults, frail, mild dementia, etc.) |
7.1-8.5% | High-risk patients (severe hypoglycemia, limited life expectancy, advanced dementia, etc.) |
Preprandial and Postprandial Glucose Targets for A1C ≤7.0%
—> Post meal change of ~2-3 is ok lol
A1C (%) | Preprandial PG (mmol/L) | 2-hour Postprandial PG (mmol/L) |
|---|---|---|
≤7.0 | 4.0-7.0 | 5.0-10.0 |
If A1C ≤7.0% not achieved despite above targets | 4.0-5.5 | 5.0-8.0 |
Hypoglycemia (Low Blood Sugar) – What to Know
DEFINITION:
Blood sugar < 4.0 mmol/L
u can literally die after being in a coma —> hypoglycemia is not epic
SYMPTOMS:
Shaky, sweaty, dizzy, hungry, fast heartbeat, confusion
Nocturnal = nightmare, restless sleep, sweating, morning headache
** Beta blockers might mask symptoms of hypoglycemia EXCEPT SWEATING
—> Beta blockers are beta males who are stinky sweaters!!!!!!!
Adrenergic symptoms = A FOR ANXIETY
These occur first, followed by neuroglycopenic symptoms
MAY NOT OCCUR in ppl with impaired awareness of hypoglycemia
Trembling, palpitation, swearing, anxiety, hunger, nausea, tingling
Neuroglycopenic = THINK OF A DRUNK PERSON
Difficulty concentrating, confusion, weakness, drowziness, slurred speech, headache, dizziness
TREATMENT: "Rule of 15" → 15g sugar (e.g., juice, glucose tabs), wait 15 min, recheck
If after 3 attempts you’re still hypoglycemic, GO TO HOSPITAL !!! YOU FAILED YOURSELF DUMMY.
Prevention: Eat regular meals, adjust meds if needed
HYPOGLYCEMIA LEVELS:
1) LEVEL 1 HYPOGLYCEMIA
Glucose level below normal (3-3.9)
Autonomic symptoms present , no neuroglycopenic symptoms
2) LEVEL 2 HYPOGLYCEMIA
Glucose level below normal (<3)
Neuroglycopenic symptoms without significant impact on mental status (they ain’t going psycho)
Autonomic symptoms may or may not be present
3) LEVEL 3 HYPOGLYCEMIA
Glucose levels VERYYY BELOW normal
Neuroglycopenic symptoms that are BAD (altered physical / mental status)
Requires assistance to treat
COUNSELLING TIPS:
Important esp for bozos on sulfonylureas, meglitinides, insulin
Review possible causes w them (delayed meal, increased activity, drugs, alcohol)
REDUCING HYPOGLYCEMIA RISK DURING EXERCISE
Reduce bolus dose of insulin at time of exercise
Reduce or suspend basal insulin for exercise duration (if activity < 45 minutes)
Lower basal rate overnight after exercise by ~20%
Increase carbohydrate consumption prior to, during, and after exercise as necessary
**BASIC TIPS —> Just reduce both types of insulin and eat like a fatty mc fatty bc I guess you ain’t gonna be at a net calorie deficit when u exercise LOSERRRR
HYPOGLYCEMIA AND DRIVING
You gotta be 5 to drive —> (Levels <5 = DO NOT DRIVE)
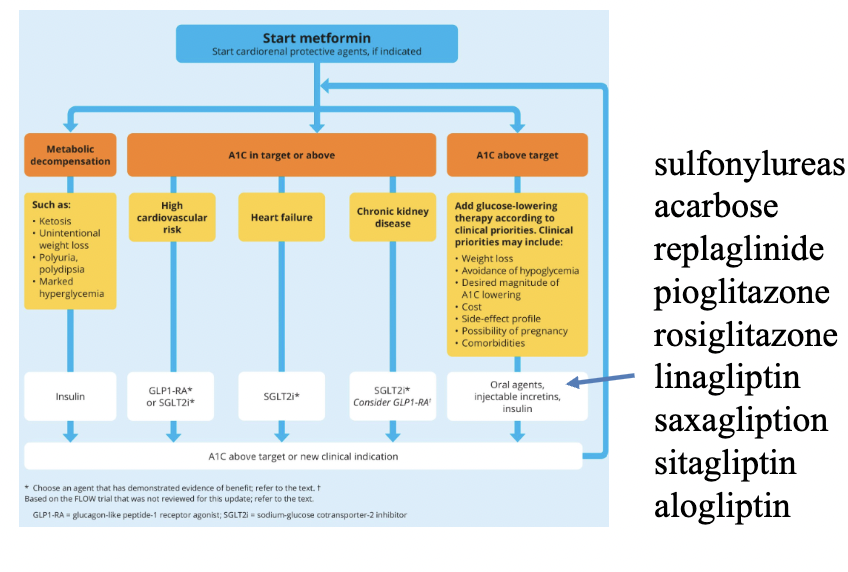
Choosing the Right Medications for Type 2 Diabetes
Medications are chosen based on the patient’s specific needs:
Medication Class | Benefits | Risks | Who it's best for |
|---|---|---|---|
Metformin | Weight neutral, cheap, good for the heart | GI upset, B12 deficiency | First-line for almost everyone |
SGLT2 inhibitors (-flozins) | Weight loss, good for kidneys & heart | Increased urination, risk of infections | Good for heart failure & kidney disease |
GLP-1 RAs (-tides) | Weight loss, heart benefits | Injectable, GI side effects | Good for weight loss & heart benefits |
Sulfonylureas (gliclazide, glimepiride) | Cheap, effective | Can cause low sugar (hypoglycemia), weight gain | Use if cost is an issue
|
Insulin | Lowers sugar effectively | Weight gain, hypoglycemia | Used later when other meds aren't enough |
What about DPP-4 Inhibitors
They’re an option but mainly used if patients cant tolerate SGLT2i or GLP1 RA
Weaker and not the best option b/c no heart or kidney benefits
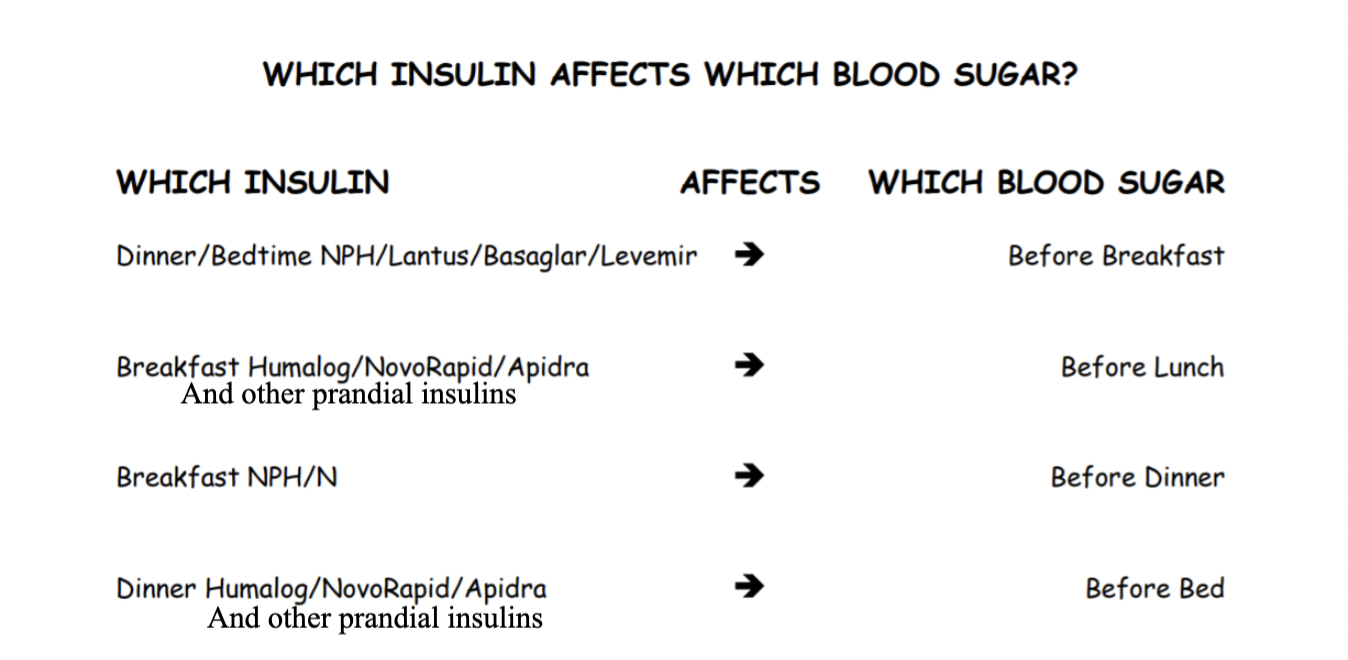
When to Start Insulin & How to Adjust
We start insulin when other meds aren’t enough (A1C is above target AND patient is on 2-4 maximal doses of non insulin medications)
Starting dose: Basal insulin (e.g., glargine) at 10 units/day or 0.1-0.2 units/kg (5-10 units at bedtime)
Most people will eventually require 25-50 units of basal insulin
Adjusting: Increase by 1 unit each morning if blood glucose above 7, check A1C in 3 months
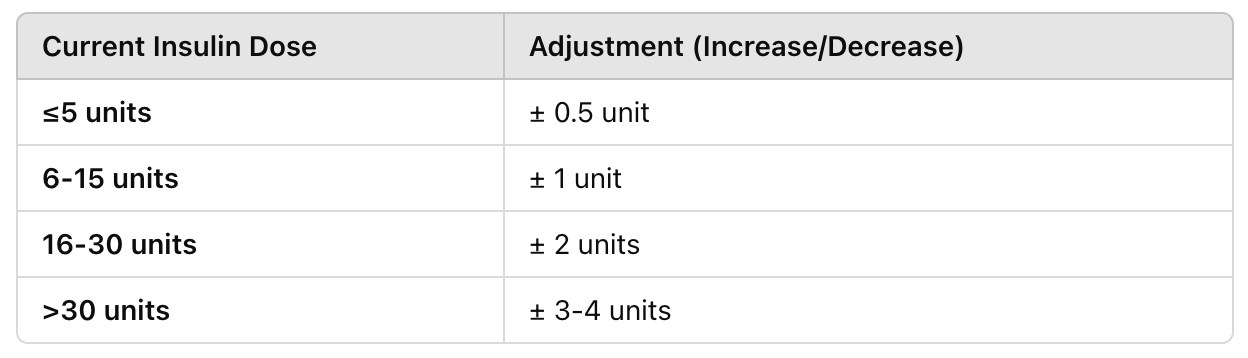
You always only want to change the dose of ONE type of insulin at a time
Look for patterns outside the goal range (one abnormal reading can be ignored)
IF ALL blood sugars are high —> adjusting morning blood sugars takes priority
Always assess effect of dose change (wait 2-3 days before making another insulin adjustment)
DISCONTINUING MEDICATIONS WHEN STARTING INSULIN ?
Don’t discontinue other diabetes medications UNLESS its
Rosiglitzone or Pioglitazone
in which case…. u should prob discontinue lol
BOLUS INSULIN (Nutritional Insulin)
Start with 2 units w/ largest meal (or meal that has highest postprandial reading)
Adjust weekly —> Eventually most ppl have 50% basal 50% bolus
DISCONTINUE OR REDUCE DOSE of sulfonylureas, repaglinide (to decrease risk of hypoglycemia)
How often should blood glucose levels be measured?
🔹 Depends on type of diabetes & medications:
GENERALLY:
Check once daily for once a day injections
Twice daily for twice a day injections etc
✅ Exception: If sick, fasting, or changing meds → check more frequently!
Sick Day Management for Diabetes
Key Principles
✅ Stay Hydrated – Drink plenty of fluids with minimal sugar, avoid caffeine.
✅ Prevent Low Blood Sugar – If you can't eat normally, have 15g carbs (e.g., juice, toast).
✅ Monitor Blood Sugar Frequently – If using insulin, check levels more often and adjust as needed.
✅ Medications to Hold if Sick & Eating Less for >24h:
🚫 Diabetes meds: Metformin, SGLT2 inhibitors
🚫 Blood pressure meds: Certain ones (ask doctor)
🚫 ALL water pills (diuretics)
🚫 NSAIDs (anti-inflammatory pain meds)
➡ Continue Basal Insulin even if not eating, but rapid-acting insulin may need adjustments.
When to Seek Medical Help 🚨
📌 Blood sugar >14 mmol/L before meals/bed (2x in a row) AND
Urine ketones moderate to large OR
Blood ketones >1.5 mmol/L
📌 Other RED FLAGS:
Severe vomiting or diarrhea (>24h)
Can't keep blood sugar >4 mmol/L
Signs of Diabetic Ketoacidosis (DKA)
Signs of Diabetic Ketoacidosis (DKA) ⚠
❗ Extreme Thirst & Urination
❗ Weakness, Nausea, Vomiting, Stomach Pain
❗ Trouble Breathing (Air Hunger)
❗ Confusion
Why Sliding Scale Insulin (SSI) Alone is Inefficient
🚫 Problem: Sliding scale insulin (SSI) only reacts to high blood sugar after it happens.
✅ Solution: A proactive approach with Basal + Bolus + Correction insulin leads to smoother glucose control.
How Insulin Therapy Works Best
🔹 Basal Insulin (Long-acting) – Provides steady background insulin all day.
🔹 Bolus Insulin (Mealtime/Prandial) – Covers blood sugar spikes from eating.
🔹 Correction Insulin – Adjusts for unexpected highs (like a safety net).
Key Hospital Considerations
🏥 Why SSI Alone is Not Enough:
It lets high blood sugar happen first instead of preventing it.
Leads to rollercoaster glucose levels (highs and lows).
🏥 When to Call the Doctor:
Blood sugar < 4 mmol/L – Risk of severe hypoglycemia.
Blood sugar > 19 mmol/L – Severe hyperglycemia may need urgent adjustments.
🏥 Why Insulin is the First Choice in Hospital:
Other diabetes meds may be temporarily stopped (e.g., kidney/liver issues).
Insulin is the most reliable way to control blood sugar in critically ill patients.
Bottom Line
❌ Sliding Scale Alone = Reactive, leads to variable blood sugar
✅ Basal + Bolus + Correction = Proactive, smoother blood sugar control