Lecture 8: Alteration in the hematologic system
anemia:
reduction in the total number of erythrocytes in the circulating blood or in the quality or quantity of hemoglobin
(causes)
impaired erythrocyte production
acute or chronic blood loss
increased erythrocyte destruction
combination of above
classifications
anemias are classified in two ways
etiology- based on their etiology
morphology- morphology classification is based on two characteristics
size
cellular size is identified by terms that end in -cytic such as macrocytic, microcytic, normocytic
macrocytic typically results bc of a defect in dna synthesis (usually bc of b12/folate deficiencies). they are typically larger but theres less of them and they are usually immature. they also often have structural and functional abnormalities such as immaturity, fragility, and decreased numbers
hemoglobin content
hemoglobin content is identified by terms that end in -chromic such as normochromic and hypochromic
physiologic manifestation
major physiologic manifestation is hypoxia (reduced oxygen carrying capacity)
symptoms
symptoms vary based on severity and the ability for the body to compensate for hypozia
body compensation for anemia by respiratory (increased rate and depth of breathing), cv (increased heart beat (rate? bp? both?), and hematologic systems
classic anemia symptoms
fatigue, weakness, dyspnea, pallor
anisocytosis- rbcs are present in various sizes
macrocytic-normochromic anemias:
macrocytic (also termed megaloblastic) anemia is:
characterized by defective dna synthesis that results ineffective erythropoesis (large megaloblasts [large precursor (immature) cells to rbc’s, shouldn’t be in circulation] and large macrocytes [large rbc])
defective dna synthesis is caused by deficiencies in vitamin b12 or folate (both are needed as coenzymes for nuclear maturation and the dna synthesis pathway)
rna processes occur at a normal rate
results in the unequal growth of the nucleus and cytoplasm
dna synthesis being impaired causes the cell cycle/division to slow or stop but rna synthesis is continuing which directs production of proteins and other cellular components. since rna synthesis is at a normal rate while cell devision is slowed/stopped, there will be more proteins/cell components than there should be
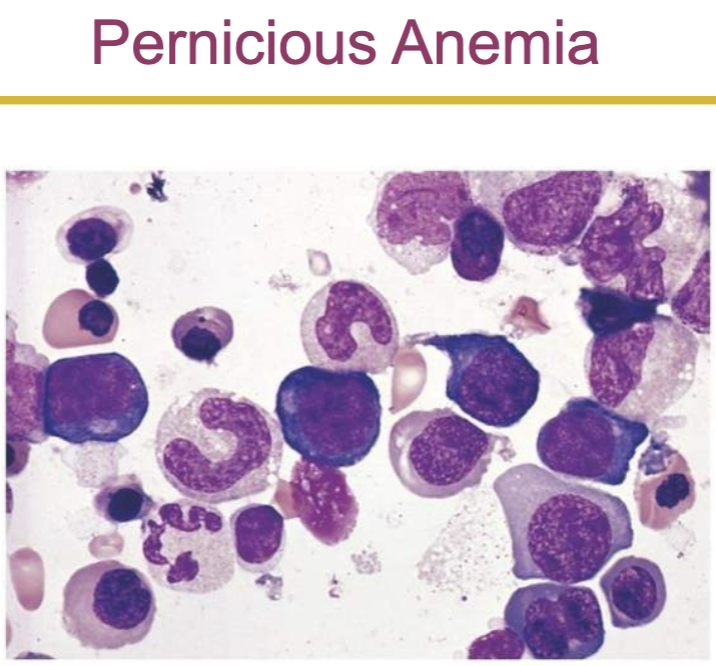
pernicious anemia
the most common type of macrocytic normochromic anemia
caused by vitamin b12 deficiency
vitamin b12 deficiency results from defective secretion of intrinsic factor from the gastric parietal cells (gastric mucosal cells)
intrinsic factors is an enzyme that is essential for vitamin b12 absorption
vitamin b12 is required for nuclear maturation of dna synthesis in erythrocytes
symptoms- develop slowly (20-30 yrs), typical anemia symptoms
neurologic manifestations results from nerve demyelination
others
loss of appetite, abdominal pain, beefy red tongue (atrophic glossitis), icterus (jaundice), splenic enlargement
evaluation
blood test, bone marrow aspiration, schilling test, gastric biopsy, clinical symptoms
schilling test: the administration os radioactive cobalamin and the measurement of its excretion in the urine to test for vitamin b12 deficiency
treatment
parenteral (cyanocobalamin by intramuscular injection) or high oral doses of vitamin b12
parenteral == med administration by a way other than digestive tract
untreated pernicious anemia is fatal due to heart failure
effectiveness of vitamin b12 therapy is measured by reticulocyte count
folate deficiency anemia
absorption of folate occurs in the upper small intestine
not dependent on any enzyme or other facilitating factor
folic acid is stored in the liver
its essential for rna and dna synthesis within erythrocytes
similar symptoms to pernicious anemia except neurological manifestations are generally not seen
treatment requires daily oral administration of folate
microcytic hypochromic anemia:
characterized by abnormally small and pale erythrocytes (due to abnormally reduced amounts of hemoglobin)
results due to
disorders of iron metabolism
disorders of porphyrin and heme synthesis
disorders of globin synthesis
iron deficiency anemia
most common type of anemia worldwide
caused by
nutritional iron deficiency (the most common cause of iron deficiency anemia is chronic blood loss; if theres chronic blood loss, its depleting the iron faster than the nutritional intake is)
metabolic or functional deficiency
progression of iron deficiency causes
brittle, thin, coarsely ridged, and concave (spoon shaped) nails
a red, sore (ex. at the corner of mouth), and painful tongue
other symptoms include weakness, and dyspnea
evaluation: decreased hemoglobin, bone marrow biopsy (to measure iron storage), serum ferrin and treansferrin
treatment
identify and eliminate the cause, such as blood loss
iron replacement therapy
normocytic-normochromic anemias:
characterized by rbcs that are relatively normal in size and hemoglobin content but insufficient in number
these anemias have no common etiology, pathology, or morphological character
classified into
aplastic
posthemorrhagic
hemolytic
sickle cell
anemia of chronic inflammation
aplastic anemia
pathophysiology: autoimmune disease against hematopoiesis by activated cytotoxic t cells
in aplastic anemia, pancytopenia (reduction or absence of all three blood cell types) develops due to suppression of the bone marrow to produce adequate amounts of erythrocytes, leukocytes, and thrombocytes
manifestations: related to the speed of bone marrow destruction
treatment: removal of cause, bone marrow and peripheral blood stem cell transplantation, immunosuppressive therapy
posthemorrhagic anemia
acute blood loss from the vascular space
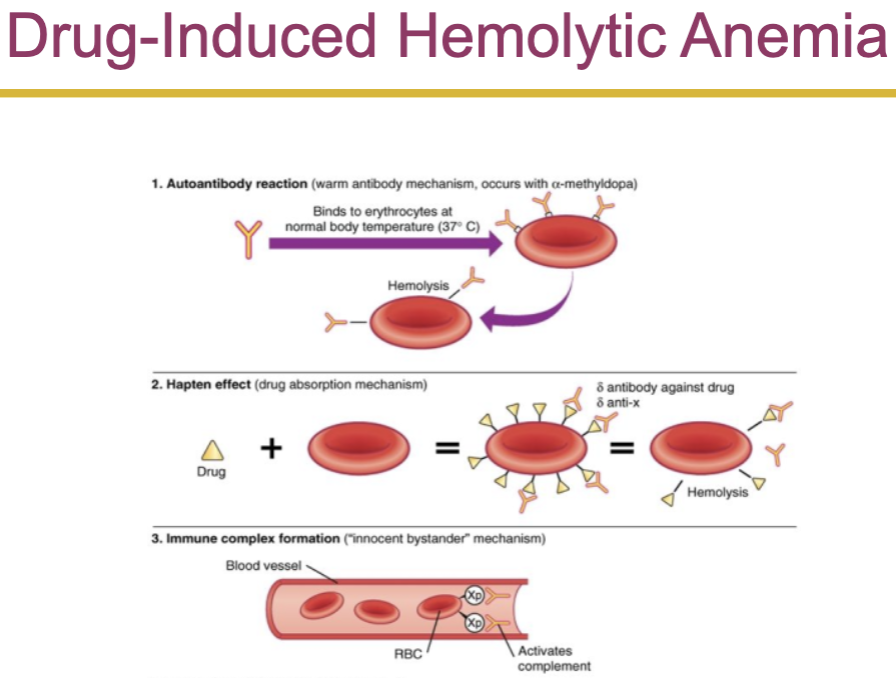
hemolytic anemia
accelerated destruction of red blood cells
sickle cell anemia
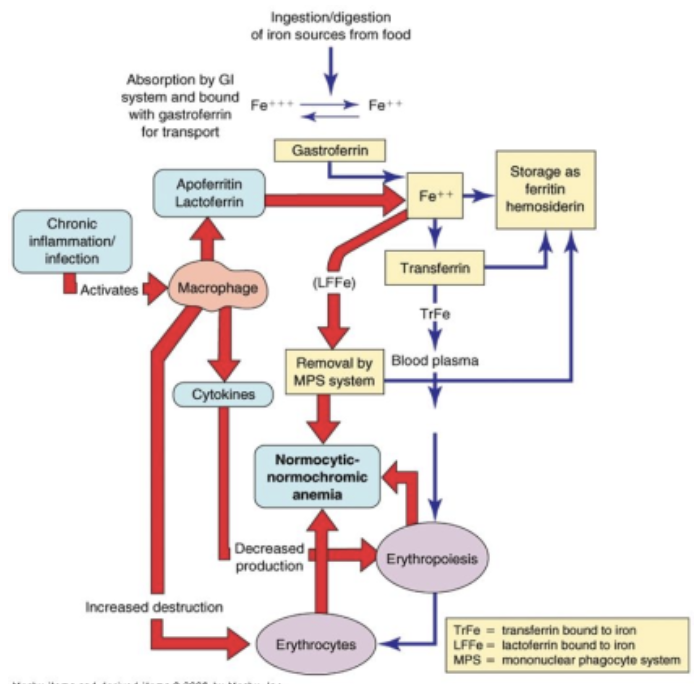
anemia of chronic inflammation
mild to moderate anemia seen in
aids, rheumatoid arthritis, lupus erythematosus, hepatitis, renal failure, and malignancies
caused due to
decreased erythrocyte life span
ineffective bone marrow response to erythropoietin
altered iron metabolism
alterations of leukocyte function:
quantitative disorders
increases or decreases in cell numbers
bone marrow disorders or premature destruction of cells
response to infectious microorganism invasion
qualitative disorders
disruption of cellular function
quantitative alterations of leukocytes:
leukocytosis
leukocytosis is a normal protective physiologic response to physiologic stressors
leukopenia
leukopenia is not normal and not beneficial
a low white count predisposes a patient to infections
ex. neutropenia- reduction in circulating neutrophils due to
prolonged severe infection
decreased production
reduced survival
eosinophilia:
hypersensitivity reactions trigger the release of eosinophilic chemotactic factor of anaphylaxis from mast cells
increased in allergic disorders
basophils:
basophils account for only 0-1% of the circulating wbcs
basophilia
response to inflammation and hypersensitivity reactions
basopenia
occurs in acute infections, hyperthyroidism, and long term steroid therapy
infectious mononucleosis:
acute, self limiting infection of b lymphocytes transmitted by saliva through personal contact
commonly caused by the epstein barr virus (ebv) - 85%
b cells have an ebv receptor site
diagnostic test
monospot qualitative test for heterophilic antibodies
monospot test detect IgM
symptoms
lymph node enlargement (is a classical clinical manifestation), fever, sore throat, increased lymphocyte count, and atypical (activated) lymphocyte
leukemias:
malignant disorder of the blood and blood forming organs
excessive accumulation of leukemic cells
acute leukemia
presence of undifferentiated or immature cells, usually blast cells
chronic leukemia
predominant cell is mature but does not function normally
early signs and symptoms of leukemias: bruising, fatigue, bone pain, anorexia
myeloma:
proliferation of plasma cells
the tumor may be solitary or multifocal (multiple myeloma)
the malignant plasma produce abnormally large amounts of one class of immunoglobulin or incomplete immunoglobulin
the unattached light chains of the immunoglobulins (bence jones proteins) can pass through the glomerulus and damage the renal tubular cells
multiple myeloma causes increased osteoclastic bone destruction
clinical manifestations
cortical (compact bone) and medullary (spongy bone) bone loss
skeletal pain
recurring infections due to loss of the humoral immune response (humoral as in humor as in body fluid so its the fluid [blood/lymph] immune response)
malignant lymphomas:
malignant transformation of a lymphocyte and proliferation of lymphocytes, histiocytes, their precursors, and derivatives in lymphoid tissues
two major categories
hodgkin lymphoma
non hodgkin lymphoma
hodgkin lymphoma:
characterized by the presence of reed sternberg cells in the lymph nodes
reed sternberg cells are necessary for diagnosis, but they are not specific to hodgkin lymphoma
classical hodgkin lymphoma
nodular lymphocyte predominant hodgkin lymphoma
physical findings
adenopathy (swelling/enlargement of lymph nodes), mediastinal mass, splenomegaly, and abdominal mass
symptoms
fever, weight loss, night sweats, pruritus (itching)
laboratory findings
thrombocytosis (high number of platelets), leukocytosis, eosinophilia, elevated esr, and elevated alkaline phosphatase
elevated esr: erythrocyte sedimentation rate, aka how quickly rbcs settle at the bottom of a test tube, helps detect inflammation (more inflammation means more of certain proteins which causes rbcs to clump together which causes them to sink)
paraneoplastic syndromes
common sites of hodgkin lymphoma masses (either enlarged lymph nodes or tumors)
left and right axillary nodes
left and right cervical supraclavicular nodes
retroperitoneal nodes (located behind the peritoneum)
left and right inguinal nodes
uncommon sites of hodgkin lymphoma masses (either enlarged lymph nodes or tumors)
epitrochlear and brachial nodes
mesenteric nodes
popliteal nodes
disorders of platelets:
immune thrombocytopenic purpura (itp)
IgG antibody that targets platelet glycoproteins
antibody coated platelets are sequestered and removed from the circulation
the acute form of itp that often develops after a viral infection is one of the most common childhood bleeding disorders
manifestations
petechiae (tiny, pinpoint, red/purple spots on skin caused by bleeding under skin from capillaries, don’t blanch when pressed) and purpura (larger, flat, red/purple spots caused by bleeding under the skin, often from larger vessels than those causing petichiae), progressing to major hemorrhage
alterations of platelet function:
qualitative alterations in platelet function demonstrate an increased bleeding time in the presence of a normal platelet count
platelet function disorders result from platelet membrane glycoprotein and von willebrand factor deficiencies
manifestations
petichiae, pupura, mucosal bleeding (bleeding from any mucous membrane, ex. nose, mouth, gums, gi tract), gingival bleeding, and spontaneous bruising
disorders can be congenital or acquired
alterations of coagulation:
vitamin k deficiency
vitamin k is necessary for synthesis and regulation of prothrombin, the prothrombin factors (ii, vii, xi, x), and proteins c and s (anticoagulants)
liver disease
liver disease causes a broad range of hemostasis disorders
defects in coagulation, fibrinolysis, and platelet number/function