Anatomy/Physiology Exam 2
Ch 11: Nervous system
General steps:
Sensory input (Sensory nerve fibers/afferent division)
Integration (CNS)
Motor output (motor nerve fibers/efferent division)
Basic architecture:
Central Nervous System = brain and spinal cord (integrative/control)
Peripheral Nervous System = cranial and spinal nerves (communication btwn CNS and body)
Sensory division = somatic and visceral sensory fibers (impulses from receptors to CNS)
Motor division = conducts impulses from CNS to effectors (muscles/glands)
Somatic nervous system = voluntary; from CNS to muscles
Autonomic nervous system = visceral/involuntary; from CNS to cardiac, smooth, glands
Sympathetic division = mobilizes body during activity
Parasympathetic division = conserves energy; promotes housekeeping during rest
Neuroglia: supportive cells in nervous system
astrocytes - support, organize, clean (neurotransmitters), feed; form blood/brain barrier; most abundant
microglial cells - immune roles (ordinary WBC cannot cross blood/brain barriers)
ependymal cells - line CSF spaces; produce CSF (choroid plexus of ventricles)
oligodendrocytes - form myelin sheath around CNS axons (interacts with multiple)
satellite cells - surround PNS cell bodies (similar to astrocytes)
Schwann cells - form myelin sheath around PNS axons (single portion of axon)
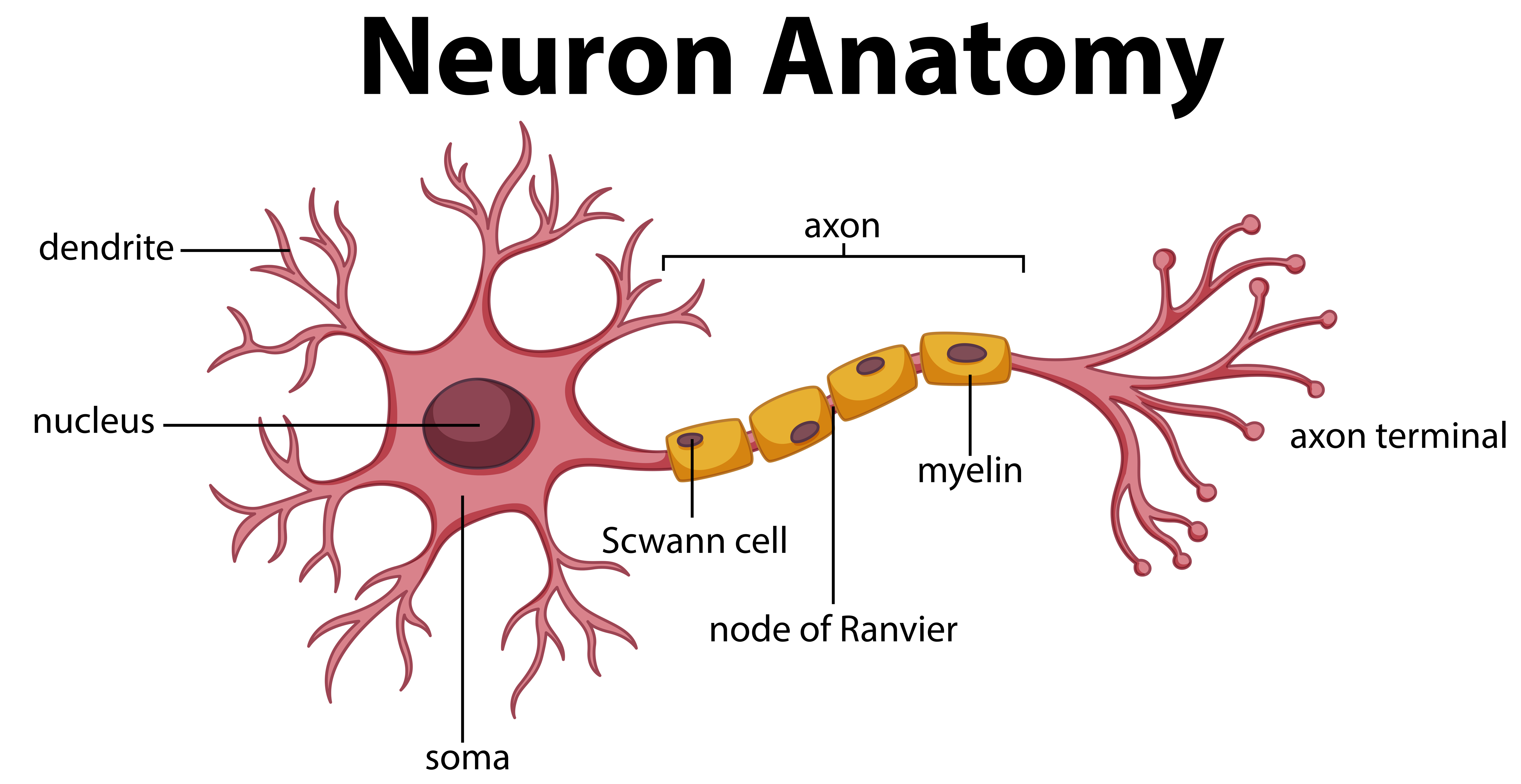
Neurons:
Highly elongated (axon/dendrite structure); high metabolic rate (aerobic); highly differentiated structure (cannot divide); long lived (lifetimes)
Dendrites - receptive/input regions, convey messages toward body
cell body - metabolic center, clusters in CNS=nuclei, clusters in PNS=ganglia
axon hillock - initiates AP in response to EPSP depolarization to threshold. “trigger zone”
Schwann cells/myelin sheath - insulates axon; lipid (plasma membrane); accelerates AP
node of Ranvier - gaps in myelin to allow for saltatory conduction
axon - propagates AP to terminus
axon terminal - secretory region, releases neurotransmitters to communicate
AP terminated; triggers Ca+2 influx, exocytosis of NT by synaptotagmin and SNAP/SNARE complex
afferent (sensory) neuron - transmit sensory info towards CNS (unipolar - one branched process [T], sensory of PNS)
efferent (motor) neuron - carry impulses away from CNS (multipolar - many dendrites and one axon, common in CNS; body in CNS)
interneurons - btwn motor/sensory neurons; through CNS; 99% of neurons; multipolar
bipolar - one dendrite, one axon; rare, typically in special senses
Membrane potentials
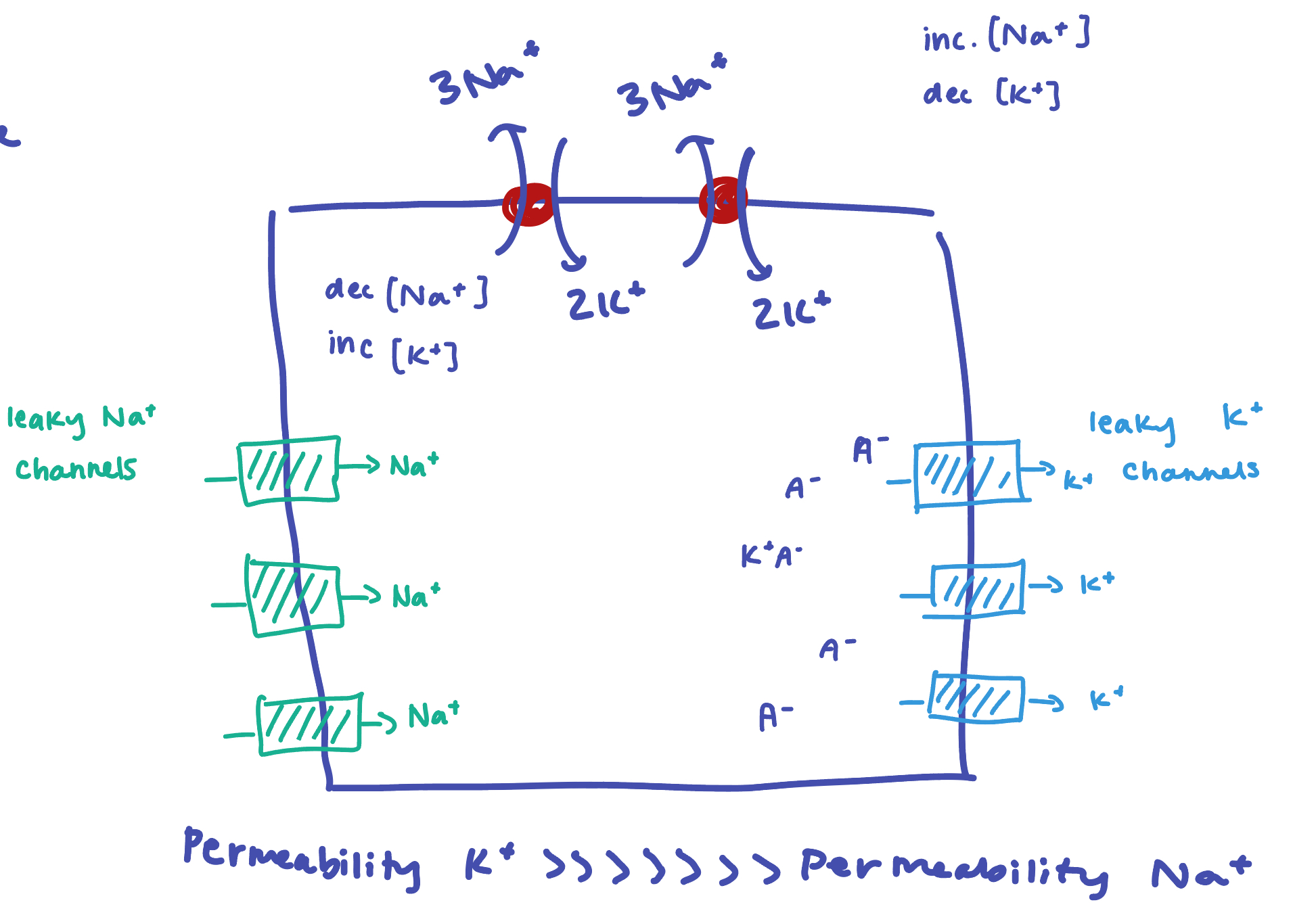
Resting potential - established by Na+/K+ ATPase (3 Na out, 2 K in; active ion pump); -70mV;
K+ has higher permeability (leaks out of cell and leaves behind anions; leak channels); Na+ leaks into cell MUCH slower, maintains conc. gradient)
Resting potential depends on the permeabilities of ions (closest to equilibrium of K+)
Graded potential - incoming (local) signals with varying strength (not all or nothing); must add up before it initiates an AP; current decreases with distance and varies with strength of stimulus
depolarization - decrease in membrane potential (EPSP; closer to AP threshold; -55mV; Na+ channels [voltage gated ion channels])
inactivation gate of channel prevents continuous activation; one way propagation
hyperpolarization - increase in membrane potential (IPSP; Cl- or VG K+ channels)
receptor potential - graded potential at sensory neuron due to physical or chemical change
postsynaptic potential - graded potential produced by ligand-gated ion channels (LGICR) in postsynaptic cell (NT, NM, hormone)
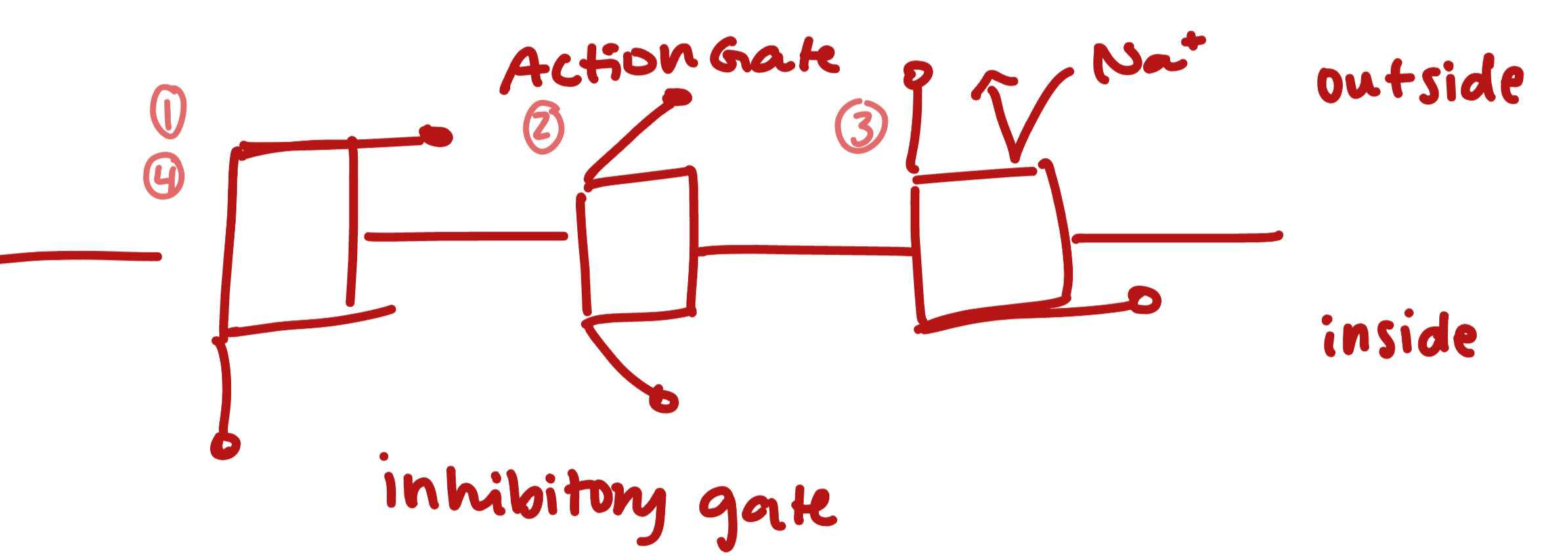
Action potential - long distance signal of axon (always same strength)
initiation/threshold - depolarization at hillock opens VG-Na+ channels (-55mV)
depolarization - Na+ influx changes polarization to +30mV
repolarization - K+ channels open as a result of potential change, influx into cell and decreases potential to baseline
absolute refractory period - when channels are open/resetting (inhibitory gate) another AP cannot occur; also why it propagates unidirectionally
AP don’t last forever due to diffusion, leak channels, Na/K pump
hyperpolarization - continued flow of K+ decreases to -90mV
recovery - ions slowly restore back to resting potential through leaky channels and ATPase
relative refractory period - AP requires greater stimulation to reach threshold, but it can still occur

Conduction velocity - size and degree of myelination
Size - larger diameter = less resistance = faster conduction
Myelination - much faster when myelinated
Strength of signal - based on frequency and number of nerve cells engaged
Saltatory conduction - AP '“jumps” from nodes of Ranvier (insulated wave propagation, ion flow to maintain AP only at nodes)
Neuron Interfaces
Synapses
axodendritic - btwn axon ending of presynaptic cell and postsynaptic dendrite (typically chemical)
axosomatic - direct interface btwn presynaptic axon and postsynaptic soma (body); stronger effect due to proximity to axon hillock
axoaxonic - (rare) connection btwn axon terminus and axon (important in neuromodulation [alteration of strength of synapse by external forces])
electrical - gap junctions; physical portal btwn two cells for direct ion transfer/conduction of AP (rare - smooth/cardiac but NOT muscle)
chemical - rely on NT to bridge gap btwn cells and carry message
AP induces VG-channel to allow Ca+2 into the terminus; vesicular fusion triggered by Ca+2 binding to synaptotagmin, conformation change, SNARE complex proteins form vesicles for exocytosis
Termination: 1) diffusion of ligand out of synapse (often reabsorbed by astrocytes); 2) reuptake by presynaptic cell for recycling/storage; 3) breakdown by enzymes in synaptic cleft
synaptic delay - chemical (diffusion limited)/physical (membrane/protein rearrangement) limitations of NT (0.3-5.0 ms); slower than electrical wave; synapse = rate limiting step (gap junctions are the fastest!)
Signaling summation
Temporal - increased frequency (helps reach threshold); one pre and one postsynaptic
Spatial - helps reach threshold; many pre and one postsynaptic
EPSP - excitatory (depolarizing) stimulus (Na+); must be summed before AP produced
IPSP - inhibitory (K+ channels or Cl-); if present, EPSP must overcome to activate AP (integration)
Synaptic potentiation - repeated/continuous use enhances ability to excite (larger EPSP); accumulation of Ca+2 in terminus or more complicated
Presynaptic inhibition - hyperpolarize axons (axoaxonic), inhibit NT release, smaller EPSP
Long-term potentiation (LTP) - sensitizing synaptic firing patterns in hippocampus; neural pathway is easier to trigger by some stimulus
postsynaptic receptor upregulation (DISCUSSED LATER); Ca+2 ionotropic sensitization; increased NT synthesis
Neurotransmitters
NT - chemicals that carry signals btwn neurons (or effector tissue)
chemical ID is not sufficient to determine action; actions are based on receptors (same NT can have different effect based on different receptors); different signal transduction pathways
metabotropic - activates signal transduction pathway (G-protein, secondary messengers); can alter many cell functions (enzyme activity, gene expression, ion channels)
ionotropic - activates LGICR to directly alter membrane potential in postsynaptic neuron (EPSP or IPSP)
NM (neuromodulator) - chemical signal released that affects strength of transmission (not directly EPSP or IPSP); TUNE not GENERATE signal
acetylcholine
nicotinic cholinergic receptor (NAchR); ionotropic, EPSP; skeletal muscle stimulation (PNS); nicotine is agonist, increases sympathetic activation
muscarinic cholinergic receptor (MAchR); metabotropic, M2-Gi inhibitory, M1/M3 excitatory; PaANS, inhibits smooth muscle and pacemaker, stimulates digestion; muscarine is agonist, atropine is antagonist, used to control HR
norepinephrine/epinephrine
alpha adrenergic receptors; metabotropic, a1 excitatory, a2 inhibitory; a1 stimulate smoother muscle constriction, a2 are autoreceptor negative feedback; a1 agonists for vasoconstrictors, a2 for vasodilation
beta adrenergic receptors; metabotropic, mostly excitatory (B1, B3), B2 inhibitory; B1, excitatory, increase HR and cardiac contractile force (blockers lower HR and BP); B2, smooth muscle relaxation (agonists used to reverse airway constriction); B3, lipolysis, thermogenesis
dopamine (dopaminergic receptor); metabotropic, neuromodulatory; limbic system (emotion), desire/reward, motivation, satisfaction, motor relays in midbrain (Parkinson’s); monoamine oxidase inhibitor (MAOI) inhibits degradation, increasing dopamine levels, treats depression
serotonin, 5-HT (serotonergic receptor); metabotropic, neuromodulatory; sleep, wakefulness, emotional state, perception, modulates CNS, stomach activity; serotonin reuptake inhibitors (SSRI) increase serotonin in synapses, reduce depression, LSD stimulates receptors
glutamate (glutamatergic receptors); ionotropic, EPSP; stimulatory of CNS; NMDA antagonists are anesthetics, dissociative euphoriants, alcohol is iGluR antagonist
GABA (gabaergic receptors); inonotropic, IPSP; inhibitory of CNS; benzodiazepine agonists reduce anxiety and/or muscle tone (xanax), alcohol is agonist and slows CNS
Ch 14: Autonomic Nervous System
Autonomic Nervous System - unconscious actions/changes in homeostatic set points (metabolism, reflexes, heart rate, blood pressure, respiration, digestion, etc.); Sympathetic and Parasympathetic; visceral
SyANS: moves body towards action
effector origin: thoracic and lumbar spinal cord
short preganglionic (ganglia along spinal cord); long post ganglionic
ACh (nicotinic), epinephrine/norepinephrine
extensive preganglionic branching
adrenal and sweat glands involved
elevated HR, pupil dilation, vaso-constriction/dilation, increased ventilation, inhibit glands and digestion, stimulates epinephrine production, increased metabolic rate
vascular system is under sympathetic tone at rest
Uniquely SyANS: thermoregulation (blood vessel dilation/sweat glands); release of renin from kidneys (blood pressure); metabolic effects
PaANS: moves body towards rest (maintain homeostasis)
effector origin: cranial nerves, sacral spinal cord
long preganglionic fibers (ganglia near/within organs)
ACh, (nicotinic and muscarinic)
limited preganglionic branching
slows HR, stimulates digestion, promotes peeing, restricts ventilation, sexual arousal
under tone: cardiac activity (pacemaker of heart is around 100bpm, PaANS is inhibitory), digestive and urinary activity, immunity
Vagus nerve - primary visceral sensory and PaANS effector pathway for all organs in thorax and abdomen (90% of fibers); PaANS is focused on digestive, heart, lungs
Dual innervation: both SyANS and PaANS control; allows for fine tuning (rapid and precise changes); easier to “come down” from SyANS to enter PaANS state
Mostly antagonistic, “push-pull” control
Cooperative action: sexual excitation and urination
Visceral vs Somatic NS
involuntary (Somatic NS: voluntary)
sensory - general sensations/action for organs, run with autonomic fibers (SNS: general sensations from integument and superficial regions of body; run with motor neurons; muscles)
stimulates OR inhibits, modulatory (SNS: stimulation only)
dual-fiber pathways, require synapses at autonomic ganglia (SNS: single-fiber pathway, cell body in spinal cord and axon termini at target)
NT: ACh preganglionic, acetylcholine (muscarinic) or adrenergic post ganglionic, epinephrine (SNS: ACh, glutamate and GABA in CNS)
Brain regions:
spinal cord - lateral horns (effector bodies), medial dorsal horn (visceral reflexes)
brain stem - cranial nerves and where they originate (manage ANS, network spanning these regions); ventrolateral medulla (HR and blood vessel diameter), medullary region (gastrointestinal), midbrain (pupil diameter and focus)
hypothalamus - overall control; anterior (CRH, PaANS); posterior (ACTH, SyANS)
limbic system and cortex - emotional state; fear response w amygdala; remembered stress w hippocampus
Conscious thought does not control ANS, but emotion and memory (so relaxation) can affect ANS tone; good for managing chronic stress from SyANS
Chapter 15: Endocrine system
Exocrine - “secreted outside”; chemical signals that leave internal space of body (enter lumen or exit skin); released by ducts; non-hormonal
Endocrine - “secreted inside”; chemical signals for communication; released by glands into blood stream (reach most cells)
hormone - long distance (global) signaling between tissues through the blood (or lymph)
paracrine - “secreted along side”; short distance (released into ISF to near-by tissues; act locally); can be the same chemical as hormone
autocrine - “secreted by self”; short distance (target the same cell that released it); negative feedback
Hormones:
water soluble: fast-acting, short-lived; GPCR or RTK signaling
amines - nitrogenated compounds; acetylcholine (made from phospholipid, NOT a lipid), biogenic amines (amino acid derivatives: epi/norepi, dopamine, thyroid hormone, serotonin, melatonin
catecholamines - derivatives of tyrosine (dopamine, norepinephrine, epinephrine, thyroid hormones)
indolamines - derivatives of tryptophan (serotonin, melatonin)
peptides - small protein fragments; hypothalamic and pituitary hormones
fragments of polypeptide gene products; produced similarly to proteins, but are clipped (by proteases) rather than folded; one gene can produce many signaling peptides
proteins - posttranslationally modified before active; insulin, prolactin
eicosanoids - most paracrines, highly modified fatty acid; BP, pain, swelling
lipid soluble: long-acting, long-lived, enter cell and act deep within (change transcription)
steroids - cholesterol derivative; adrenal and gonadal
need to be transported by carrier proteins, diffuse directly through cell membranes, activate internal receptors
glucocorticoids - glucose metabolism, stress
mineralocorticoids - sodium reabsorption
gonadocorticoids - sex hormones
thyroid hormone - modified amine, acts like steroid
Stimulation
Humoral: direct change in blood ion/glucose concentration
Neural: response to neural stimulation (neuron or neurotransmitter); adrenaline in response to ACh
Hormonal: response to another hormone; aldosterone in response to ACTH
tropic = hormones that stimulate the production/release of other hormones
hypophysiotropins = released by hypothalamus into hypophyseal portal to stimulate anterior pituitary (different from neurological stimulation to posterior pituitary)
Response
cell response is based on receptor and the signal transduction at those receptors
upregulation - persistent low levels = more receptors to increase sensitization
downregulation - persistent high levels = decreased receptors to tolerate hormone
permissiveness - hormone cannot exert full effects without other hormone present
synergy - more than one hormone produces the same effect; amplification
antagonism - two hormones oppose actions of another
Hypothalamic hormones (stored in posterior lobe)
GHRH (growth hormone-releasing hormone) - stimulates GH
GHIR (growth hormone-inhibiting hormone) - inhibits GH, hunger/metabolism
TRH (thyrotropin-releasing hormone) - stimulates TSH in response to metabolic need
CRH (corticotropin-releasing hormone) - stimulates ACTH, increased by stress and low BP
GnRH (gonadotropin-releasing hormone) - stimulates FSH and LH
DA (PIH) - dopamine, inhibits prolactin
Pituitary hormones
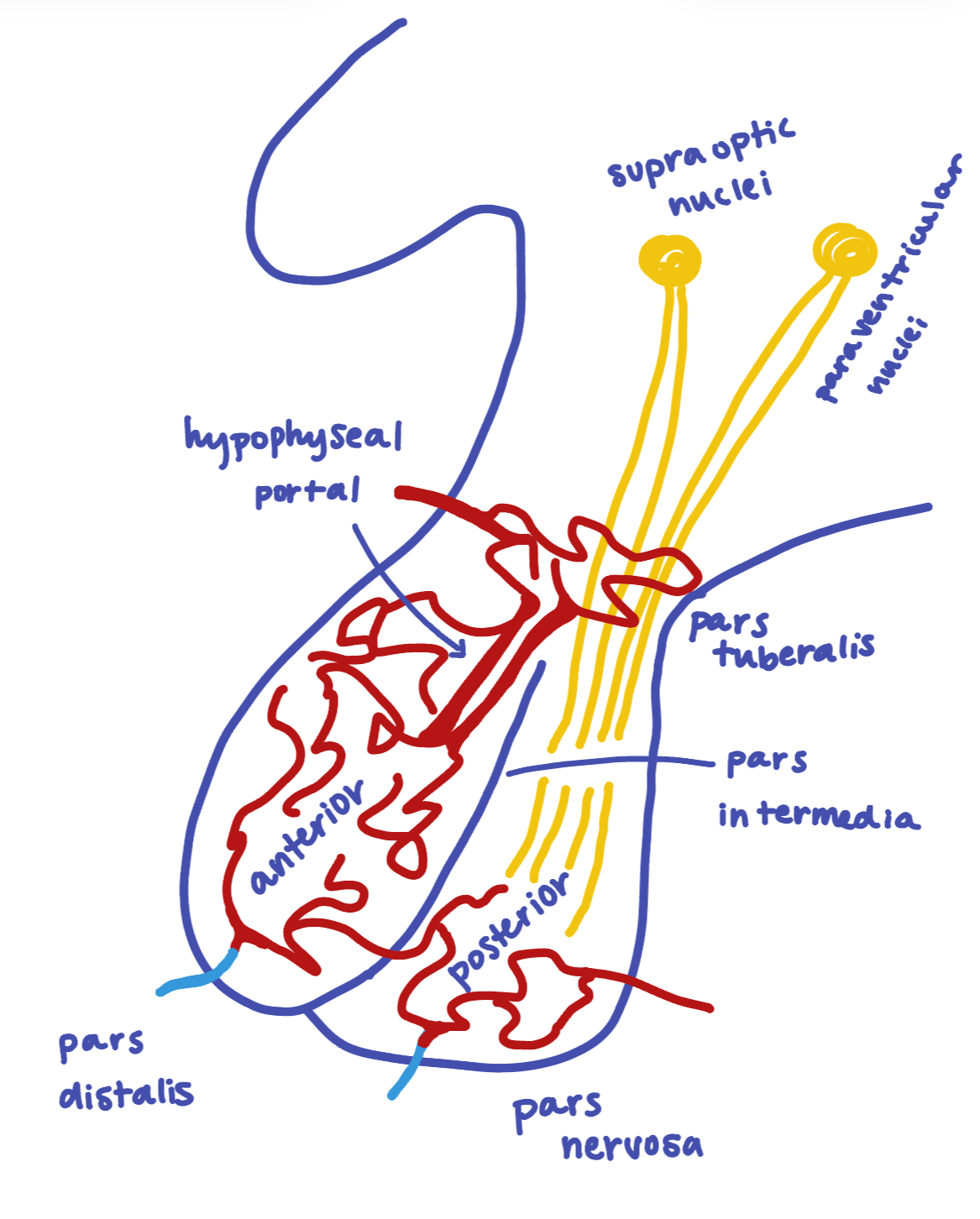
ACTH; pars distalis; stimulates adrenal cortex, trigger for cortisol; stimulated by CRH
Cushing’s disease - hypersecretion of cortisol; characteristic body mass changes, elevated blood glucose, decreased healing, possible sexual development changes, water and mineral balance; typically hypersecretion of ATCH
ADH; pars nervosa; vasoconstriction, renal water reabsorption; stimulated by low BP, high osmolarity
Diabetes insipidus - hypersecretion of ADH; high urinary volume, high thirst/water intake; damage or tumor to hypothalamus or pituitary gland
endorphins; pars intermedia; natural opioid, pain killer; stimulated by pain/stress
FSH; pars distalis; sexual development and reproduction, stimulates estrogens; stimulated by GnRH
GH; pars distalis; tissue growth, activates IGF’s to promote mitosis and tissue growth; stimulated/inhibited by GHRH/GHIH
gigantism - hypersecretion of GH during childhood
dwarfism - hyposecretion during childhood
LH; pars distalis; sexual development and reproduction, testosterone and progesterone; stimulated by GnRH
MSH; pars intermedia; melanocyte activity, melanin production; stimulated by UV exposure
oxytocin; pars nervosa; contractions, breastfeeding, social attachments and bonding; stimulated by childbirth, breastfeeding, social interaction
PRL (prolactin); pars distalis; mammary gland development and milk production; stimulated by sex hormones, maybe TRH
TSH; pars distalis; thyroid gland development and TH production; stimulated by TRH
Pineal gland: endocrine gland in cranium (melatonin)
Thyroid
Thyroid hormone - tyrosine derivatives; contain iodide and two linked tyrosine AA; secreted by follicular cells as precursors
T3 (triiodothyronine) - high activity form; formed from T4 at target tissues
T4 (thyroxine) - low activity form
TSH stimulates thyroid release and stimulation to “restock” follicle lumen; TRH stimulates release; T3 acts as negative feedback to both TSH and TRH, TRH inhibits TSH
hormonal ‘throttle’ of metabolic rate, body heat, hunger (inc. sugar uptake, release of fatty acids, mobilizes fuel); permissive to GH; sympathetic activation of B-adrenergic receptors (hyperthyroid can present as high sympathetic activation)
Goiter - enlarged or protruding thyroid; iodine deficiency = low T3 = inc TRH and TSH = thyroid growth
Grave’s disease - hyperthyroid; autoimmune, antibodies target thyroid and stimulate TH release; elevated metabolism, anxiety, insensitivity to cold
Congenital hypothyroidism - poor development of thyroid in babies (TH needed for neural and physical development)
parafollicular secretory cells - No known role in humans, calcitonin antagonizes PTH to decrease blood calcium
Parathyroid
small glands on posterior side of thyroid; produce PTH (parathyroid hormone)
PTH stimulated by low blood calcium; decreases renal secretion of Ca+2, increases Vitamin D activation, increases bone reabsorption (osteoclasts)
Adrenal gland (above renal [kidneys])
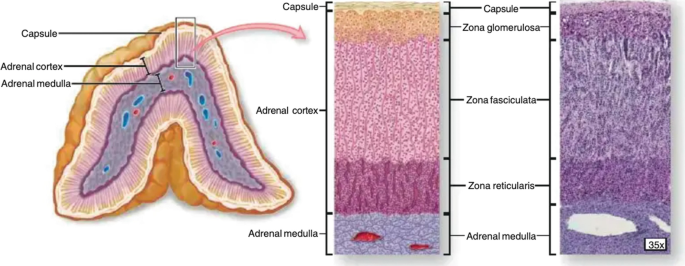
Zona glomerulosa - aldosterone (mineralocorticoid); increases Na retention and K excretion by kidney; increases blood volume/pressure; stimulated by RAAS, increase in plasma K, ACTH, inhibited by ANP
Zona fasciculata - cortisol (glucocorticoids) and some adrenal androgens (in response to ACTH); increases blood sugar/metabolic activity, gluconeogenisis, permissive to adrenaline signaling, chronic stress suppresses growth, immunity, digestion, inflammation; stimulated by ATCH and CRH
cortisol supports stress changes with increased fuel, decreased digestion, immune, reproductive and growth actions; stimulated by ATCH
Zona reticularis - androgens (gonadocorticoids) and some cortisol; stimulated by ATCH; precursors to testosterone and estrogen but also have behavioral roles (sex drive in women); some progesterone made, mostly in ovaries
Adrenal medulla - produces epinephrine and some norepinephrine
adrenaline drives primary stress response (HR, BP, metabolic rate, etc.); stimulated by SyANS
Addison’s disease - ‘underactive adrenal gland’ or adrenal hyposecretion; ATCH levels rise but insufficient corticosteroids produced; weight loss, low blood sugar, low energy, high K levels, dehydration
Pancreas (both endocrine and exocrine)
Blood sugar regulators
glucagon - stimulated by low blood sugar; alpha cells; stimulates gluconeogenisis (breakdown of fats/proteins to glucose) and glucose release from liver; targets liver and fat
insulin - stimulated by high blood sugar; beta cells; stimulated glucose uptake and storage in tissues, fat anabolism, metabolism; synergistic with growth hormone
digestive regulators
somatostatin (SST) - delta cells
pancreatic polypeptide (PP) - gamma cells
ghrelin - epsilon cells
Other
leptin, adiponectin, resistin: adipose tissue; “fat” hormones; leptin = increases metabolism, decreases appetite, high fat levels; adiponectin = increased insulin sensitivity, low fat; resistin = increased insulin resistance, high fat
ANP (atrial natriuretic peptide) - stretch in atrial wall (high BP/volume); inhibits aldosterone release, decreases blood Na and volume
EPO (erythropoietin), renin: kidneys; EPO = stimulates red blood cell formation, in response to O2 levels; renin = stimulates aldosterone production, SyANS and urinary flow
osteocalcin: bone; metabolic regulator, increases insulin production, restricts fat anabolism
Vitamin D: cholesterol in skin or ingested; absorption of Ca from diet
IGF1: liver, skeletal muscle, bone; resource/nutrient uptake; stimulated by GH