Unit IV - Animal Physiology and Anatomy
Ch 9.1 - Why We Need To Eat
Nutrient: a chemical that must be obtained by an organism from its environment to survive, provide the raw material for growth and repair, and may be a source of energy
Food for Energy
Animals eat to obtain chemical energy
- chemical energy produced by plants is transferred to herbivores and omnivores → cell use the chemical energy to fuel biological processes and physical activities, and even to maintain a constant body temperature
Factors affecting the energy requirements
Metabolism: the set of chemical reactions that occur in living organisms that are necessary to maintain life
\
Catabolism: the metabolic reactions that break down larger molecules into smaller subunits\
Anabolism: the metabolic reactions that use energy to produce larger molecules from smaller subunits\
Metabolic rate: the rate at which the body converts stored energy into working energy
→ size determines how much an animal needs to eat
→ endothermic animals need a greater deal of energy to keep their bodies warm
Metabolism - the chemical reactions that keep you alive
- Catabolism - chemical and physical breakdown of nutrients and materials in an organism
- Anabolism - the building of larger and more complex from smaller and similar molecules
Metabolic rate: the rate at which the body converts the stored energy into working energy
- body size - requires more energy the larger the body
- physical activities - require more energy as muscle burns more energy than fat
- sex - males typically have a great proportion of muscle mass than females of the same size, age, and fitness level
- age - metabolic rate decreases with age due to the decreased physical activity and loss of muscle mass
- hereditary factors - sine gave a naturally high metabolic rate or quicker converts chemical energy to metabolic rate
Measuring Energy
Basal metabolic rate: the minimum amount of energy requires to keep you alive
\
One calorie = 1000 calories / 4180 J
BMR is the amount of energy you would use per day if you stayed in bed all day, only performing vita processes
→ calculated based on the consumption of oxygen
→ generally estimated using a calculation that takes into account four variable
Ch 9.2 - What and How Much We Need to Eat
Carbohydrates
- The main source of energy for the human body
- Made up of C, H, O
- The main types include Monosaccharides, Disaccharides, and Polysaccharides
- Plants use carbon to create complex molecules such as cellulose
- Foods high in carbs include: vegetables, potatoes, and grains
Monosaccharides
→ made of a singular sugar molecule and doesn’t need further breakdown as it’s the simplest form → immediately available
- eg.1 glucose → provides energy during cellular respiration and physical activities, requires breakdown before being used as a source of energy
- eg. 2,3 - galactose, and fructose
Disaccharides
→ made of two simple sugar molecules, only require the breaking of one bond for usage
- eg. maltose, lactose → milk sugar, and sucrose → table sugar
Polysaccharides
→ made of multiple bonded simple sugars, require bonds breaking before they can be absorbed into the bloodstream → used to store glucose or as a structural molecule
- eg.1 -Starch → energy source for plants
- eg.2 - Glycogen → made and stored in animals, stored up to 12 hours in the liver and muscles for later use, fuel for prolonged exertion, or converted to fats
- eg.3 - Cellulose → has a straight rigid structure that composes the cell walls, and provides the fiber required for moving waste through the large intestine and colon, is extracted from the microbiome in the intestines
Lipids
- Concentrated source of chemical energy for the body
- Composed of C, H, O, and several non-water-soluble organic molecules, such as fats, phospholipids, steroids, and wax
- Triglyceride is composed of glycerol and three hydrophobic fatty acids tails
Triglycerides
→ aid in the absorption of fat-soluble vitamins
→ broken down into glycerol and fatty acids before absorption
- saturated - straight single bond, solid at room temperature, obtained through meat and butter
- unsaturated - bent double bond, can be cis/trans, oils, usually liquid at room temperature, are obtained through plant and fish oils
Fatty Acids
→ need to be obtained from the diet
- eg.1 - Omega-3 fatty acids - unsaturated fats, maintain good health and prevent heart diseases and arthritis, found in fish oils (eg. salmon, mackerel, herring), nuts, seeds, and leafy green vegetables
- eg.2 - Steroids - include testosterone and estrogen, and cholesterol, used in the production of fat-soluble hormones
- eg.3 - Phospholipids/cholesterol - make up the cell membranes
Proteins
- important structural molecules that involve in all of the metabolic activities and are used to generate motion, or serve as a hormone that influences cellular activity in another part of the body
- may be structural, regulatory, contractile, or protective
- Made up of amino acids consisting of C, H, O, N
- there are 20 different amino acids used to build proteins, of which 8 of them need to be obtained from a food source
- the C and N derived become the building block for nucleotides, nucleic acids, proteins, cells, and tissues
- can be obtained from meat, eggs, fish, and cheese; beans, lentils, seeds, and nuts
Water
- Important for chemical reactions, digestion of food, and eliminating waste products
- to regulate blood volume, regulate body temperature, and keep the skin moist
- our bodies are made up of 55% to 60% water, as well as in cell cytoplasm
Vitamins and Minerals
- vitamins are essential nutrients that are only needed in small amounts
- vitamins regulate cell functions, growth, and development
- classified as fat-soluble (vitamins A, D, E, and K) and water-soluble (vitamins B and C)
Vitamins A, D, and K can be produced in our bodies
- vitamin A - converted from beta-carotene found in green vegetables, carrots, egg yolks, and livers
- vitamin D - is formed in the skin when the skin is exposed to sunlight
- Minerals are naturally occurring elements that are used to carry out metabolic processes and to build/repair cells
- eg.1 - calcium and phosphorus - formation of bone
- eg.2 - sodium - involved in nerve impulse transmission and in muscle contraction
- eg.3 - iron - component of the blood protein hemoglobin → binds with oxygen
- eg.4 - fluorine, zinc, and copper - present in trace amount
Healthy diet
- carbohydrate that provides 55% of a person’s energy needs
- Vegetables and fruits that provide fiber (cellulose)
- Lipids should constitute no more than 30% of energy intake
- protein is recommended to prove 10% - 30% of energy
Maintaining a balance
Requires a balance in the level of physical activity, amount of food consumed, and the type consumed
Ch 9.3 - Introduction to Digestion
Specialized Digestive System
Gastrovascular cavity: a simple, sac-like digestive cavity that has only one opening through which food is taken in and waste is expelled
The structure of the Human digestive system
Gastrointestinal tract (GI tract): the passageway that extends from the mouth to the anus in which the process of digestion takes place
Main components of the GI track
- oral cavity
- pharynx
- esophagus
- stomach
- small intestines (duodenum, jejunum, and ileum)
- large intestines (ascending colon, transverse colon, descending colon, sigmoid colon)
- anus
Accessory organs
- salivary glands (Sublingual gland, Parotid gland, Submandibular gland
- liver
- gall bladder
- pancreas
Ch 9.4 - Digestion in the Mouth and Stomach
Physical and Chemical Digestion in the mouth
Enzyme: any protein-made chemical produced by the cells that facilitate biochemical reactions in the body, such as those involved in digestion and metabolism
\
Amylase: an enzyme that breaks down complex carbohydrates\
Mucus: a protective secretion produced by the epithelial cells that form the mucous membrane\
Esophagus: an organ consisting of a long muscular tube that passes food from the pharynx to the stomach → allows the food to intake the temperature of the body\
Peristalsis: the rhythmic, involuntary wave-like contractions of the smooth muscles of the gastrointestinal tract
Food is broken down into smaller pieces → digestion begins
- incisors and canines → grab and cut the food
- premolars and molars → grind and crush food
The presence of food triggers the salivary glands to secrete saliva that contains amylase
→ breaks down starch to disaccharides
→ dissolves food particles, making it possible to taste the food
→ the mucus acts as a lubricant and aid in swallowing
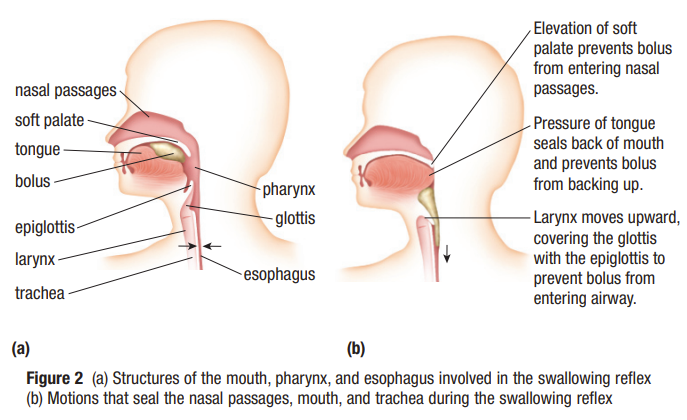
The tongue pushed the bolus into the back of the mouth to be swallowed
- the soft palate is raised → prevent food from entering the nasal passage
- the larynx is raised against the epiglottis → covers the entrance to the trachea → prevents food from entering the lungs
Food moves from the mouth to the long, muscular tube called the esophagus that carries food from the pharynx to the stomach → peristalsis activates from the stretching of the walls
→ ensures the movement of food down the esophagus and into the stomach and through the entire digestive system
The Structure of the Stomach
Sphincter: the circular muscle that contracts to close an opening in the body
\
Chyme: a semi-liquid mixture of food and gastric juice
The movement of food in and out of the stomach is controlled by circular muscles called sphincters → more than 50 in the human body
- \
Ch 10.1 - The Need for a Respiratory System
Aerobic Cellular Respiration: The Need for Oxygen
Aerobic cellular respiration: the series of chemical reactions that occur in the cell that provides energy and consume oxygen
\
Phosphorylation: the addition of a phosphate group to a molecule, the phosphate group is added to ADP, creating the ATP molecule
Cells use oxygen to obtain energy from food → aerobic cellular respiration
Glucose + oxygen → carbon dioxide + water + energy
about 64% of the energy released is released as thermal energy → maintain a constant body temperature, and 36% is stored in adenosine triphosphate
- ATP is formed when energy from the breakdown of glucose is used to attach a phosphate group onto adenosine diphosphate
Cellular respiration shows the storage of energy by conversion of ADP to ATP and the release of some energy as thermal energy
Glucose + oxygen + adenosine diphosphate + phosphate → carbon dioxide + water + adenosine triphosphate + thermal energy
Gas exchange and Ventilation
Gas exchange: the process whereby the body cells obtain oxygen and get rid of carbon dioxide
\
Ventilation: the process in more complex organisms that ensures a flow of oxygen-rich to the lungs
Simple organisms such as sponges and jellyfish have simple gas exchange
- oxygen diffuses directly from the surrounding environment through the cell membrane
- carbon dioxide diffuses from the cells through the cell membrane into the environment
In mammals, gas exchange occurs in the lungs and in the bloodstream
- oxygen is transported through the bloodstream and diffuses into all the cells
- carbon dioxide is transported through the bloodstream to the lungs
the process of moving oxygen-rich air to the lungs and carbon dioxide-rich air away from the lungs → ventilation/breathing
Ch 10.2 - Respiratory Structures and Processes
Respiratory Structures in Mammals
- a thin permeable respiratory membrane through which diffusion can occur
- a large surface area for gas exchange
- a good supply of blood
- a breathing system for bringing oxygen-rich air to the respiration membrane
The Structure of the Lungs
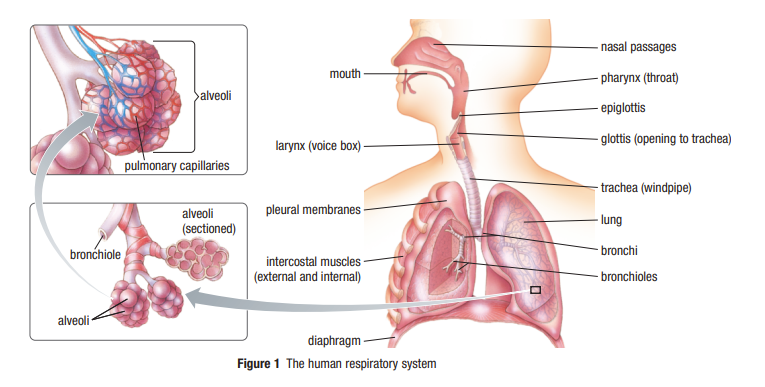
Trachea: the tube leading from the mouth towards the lungs
\
Bronchus: one of the two main branches of the trachea that lead towards the lungs\
Bronchiole: a tiny branch of a bronchus that connects to a cluster of alveoli\
Alveolus: a tiny sac at the end of a bronchiole that forms the respiratory membrane
Nasal Passage (conductive zone)
- mouth and nose intake air and breathe out waste
- air is warmed, moistened, and filtered
- lined with tiny hairs and mucus → filters out and trap dust and other airborne particles → prevent them from entering the lungs
Pharynx (conductive zone)
- passage from the nasal cavity and larynx and esophagus
- part of the respiratory and digestive system
Larynx (conductive zone)
- passageway for air only (to only the trachea)
- covered by the epiglottis
Larynx: Epiglottis (conductive zone)
- a membrane that covered the larynx when you swallow → direct food into the esophagus
- remain open during breathing → air flows into the trachea
Trachea (conductive zone)
tube that carries air from the nasal passage to the bronchi
contains C-shaped rings of cartilage → supports the 24/7 opening
line with mucus-producing cells (goblet cells) and cilia → protects the lungs from foreign matter
→ mucus traps dust
→ the wave-like motions of the cilia sweep the trapped material upwards for swallowing or through coughing/sneezing
Bronchi (conductive zone)
- tubes that carry air from the trachea to the bronchiole and alveoli
- site where the respiratory system splits into L and R
Bronchiole (conductive zone)
- the airways end in clusters of tiny sacs called alveoli
Alveoli
- each cluster is surrounded by a network of capillaries
- only one cell thin
- approximately 150 mils in each lung → provide the necessary surface area for gas exchange
Diaphragm
- muscle located under the lungs
- when it contracts and relaxes it changes the volume inside the lungs → changes the pressure inside the lungs)
Gas exchange in the alveoli
The air that reaches the alveoli is at around 37C and moist
- oxygen can’t diffuse across the respiratory membrane unless it’s dissolved in liquid
The membrane of the alveoli is only one cell layer thick → little distance between the air in an alveolus and the blood in the capillaries
- oxygen and carbon dioxide can easily diffuse across the respiratory system membrane
The network of capillaries encapsulates the alveoli → an adequate supply of blood for the oxygen to diffuse into and carbon dioxide to diffuse from
Mechanism of Ventilation
Diaphragm: a large sheet of muscles located beneath the lungs that are the primary muscle in breathing
\
External intercostal muscle: a muscle that raises the rib cage, decreasing pressure inside the chest cavity\
Pleural membrane: a thin layer of connective tissue that covers the outer surface of the lungs and lines the thoracic cavity\
Pneumothorax: a collapsed lung caused by the introduction of air between the pleural membrane
- The lungs had a thin permeable respiratory membrane, a large surface area for gas exchange, and a good supply of blood
- ventilation is a breathing system for bringing oxygen-rich hair to the respiratory membrane
When the air pressure inside the lungs is lower than the atmospheric pressure → air is forced into the lungs
when the air pressure inside the lungs is higher than the atmosphere pressure → air is forced out of the lungs
- airflow from an area of high atmospheric pressure to low atmospheric pressure
the thoracic cavity is separated from the abdominal cavity by the diaphragm
Inhalation
- the breathing control mechanisms in the brain cause the diaphragm to contract
- external intercostal muscle contract and pull the ribs upward and outward
→ increase the volume of the thoracic cavity and reduce the pressure inside the lungs → air rushes into the lungs to equalize the pressure → lungs fill with air and stretch and expand
Exhalation
the diaphragm relaxes and returns to its regular domed shape → pushes up on the lungs → external intercostal muscles also relax → ribs fall and return to their resting position
→ the air pressure inside the lungs is now greater than the atmospheric pressure → air is forced out of the lungs
During strenuous exercise/forced exhalation
internal intercostal muscles start contracting and relaxing → pull the rib cage downwards → increase the pressure inside the lungs and force more air out of the lung
The pleural membrane covers the lungs and lines the thoracic cavity
The space between the pleural membrane is the pleural cavity
filled with fluid to prevent the membranes from separating and allow them to slide past each other easily
will separate if the air is introduced to the pleural cavity through a stabbing or broken rib → cause the lungs to collapse
→ pneumothorax
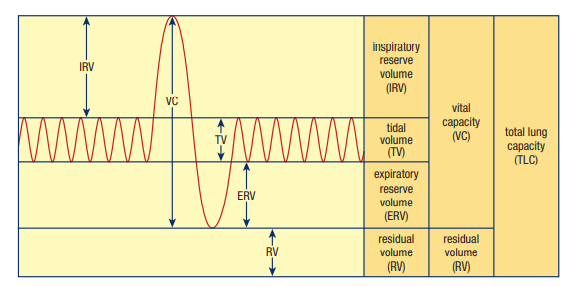
Lung Capacity
total lung capacity: the maximum volume of air that can be inhaled during a single breath
\
Tidal volume: the volume of air inhaled/exhaled during a normal, involuntary breath\
Inspiratory reserve volume: the volume of air that can be forcibly inhaled after a normal inhalation\
Expiratory reserve volume: the volume of air that can be forcibly exhaled after a normal exhalation\
Residual volume: the volume of air remaining in the lungs after a forced exhalation\
Residual volume: the volume of air remaining in the lung after a forced\
Vital capacity: the maximum amount of air that can be inhaled/exhaled
Total lung capacity: is the maximum volume of air that can be taken into the lungs during a single breath
Tidal volume: the normal involuntary breathing, only a small fraction of the total capacity
Inspiratory reserve volume: the amount of additional air that can be inhaled after a normal inhalation
Expiratory reserve volume: the volume of air left in the lungs after exhalation
Residual volume: the volume that is left to prevent the collapse of the lungs even after the expelling of the expiratory reserve volume
Oxygen use
V02: an estimated/measured value representing the rate at which oxygen is used in the body, measured in mL/Kg/Min
\
V02max: the maximum rate at which oxygen can be used in an individual, measured in mL/Kg/Min
V02max: the maximum amount of oxygen that an individual can be used during sustained, intense physical activity
V02: function of the amount of oxygen delivered to the body in a given time
Respiratory Structure in fish
The respiratory system in many aquatic animals involves gills
- gills are extensions of the body surface, folded and branched structures that provide a maximum surface area through which oxygen can be absorbed and carbon dioxide removed
- Gills are located underneath a protective bony flap at the side of the head
- movement of mouth and bony flap in some fish helps move water through the mouth and over the gills
→ ensure a constant supply of oxygen-rich water to the gills
→ eg.1 Cartilaginous fish (great white shark) - have to swim continuously to ensure that water is flowing over the gills
Fish gills are made up of several gill arches that are made up of rows of feathery gill filaments → a network of capillaries fills the gill filaments
- blood flows through the capillaries in the opposite direction to the flow of oxygen-rich water over the filaments
Countercurrent exchange maximizes the amount of oxygen that diffuses into the blood
- blood with a lower oxygen concentration is always adjacent to water with a higher oxygen concentration
- more oxygen diffuse from water to the blood when the oxygen concentration difference is great
The air we breathe
At high altitude, a given volume of air contains fewer air than it does at sea level
→ the concentration/density of air molecules decrease
The SI unit for pressure is pascal (Pa)
- a force of one newton exerted in an area of one square meter, measured in kilopascal (kPa)
Partial Pressures
Partial pressure: the pressure of each of the individual gases that make up the total pressure of a mixture of gases
The total air pressure of a mixture = sum of partial pressures of its component gases
- eg.1 - the atmospheric pressure at sea level is 101.3 kPa, and since oxygen constitutes 20.9% of the atmosphere → the partial pressure of oxygen is 20.9%% of 101.3 kPa
- eg.2 - the gases stay in solution as long as the liquid is under pressure, after the pop bottle is opened, the CO2 will continue to escape until the partial pressure of the CO2 in the pop is the same as the partial pressure of the CO2 in the air above it
Oxygen transport and diffusion
Plasma: the liquid component of blood in which blood cells are suspended
Oxygen moves from the air in the alveoli into the bloodstream → partial energy of oxygen is lower
Ch 11.2 - Blood: A Fluid Tissue
What is in Blood
Blood is a connective tissue that consists of cells suspended in an intercellular matrix
- Cellular components: Red blood cells, White cells, Platelets
- Intercellular matrix: plasma
Plasma
Serum: the fluid that results when the cells, platelets, and fibrinogen have been removed from whole blood
- protein-rich liquid in which blood cells and platelets are suspended
- over 90% is water and contains oxygen, proteins, and nutrients such as glucose, minerals, vitamins, CO2, and other waste products
- Albumins: determines the amount of water entering/leaving the bloodstream by osmosis → helps balance the amount of water within the body and maintain the appropriate volume of blood
- Gobulins: transport lipids, cholesterol, some fat-soluble vitamins, and some minerals
- Immunoglobins: help fight infectious diseases
- Fibrinogen: aid in blood clotting, and other clotting factors removed are serum
- carries several dissolved ions: Na+, K+, Ca 2+, Cl-, HCO3- → high concentration of Na ions creates an osmotic pressure gradient and cause water to enter the bloodstream → total volume of the blood increases and the blood pressure increases
Red Blood Cells (Erythrocytes)
- biconcave disks → has 20 - 30% greater surface area for gas exchange
- doe not have a nucleus → maximize the oxygen carry capacity
- to carry oxygen from the lungs to the body cells, and to carry CO2 from the body cells back to the lungs
- oxygen attaches to the hemoglobin molecules in the erythrocytes
- formed from stem cells in the marrow of the vertebrae, ribs, breastbones, skill, and bones of arms and legs
- the number of erythrocytes is maintained by a feedback system - oxygen level falls below a certain level → brain signals the production of erythropoietin that stimulates the production of erythrocytes
White Blood Cells (Leukocytes)
- the first line of defense against harmful bacteria, viruses, and other pathogens
Granular
- have granules in the cytoplasm
- neutrophils, eosinophils, basophils
- contain chemicals that attack foreign material and microorganisms
- attracted to the site of an infection/injury and kill bacteria
Agranular (Lymphocytes and Monocytes)
- specialized for engulfing bacteria
- Lymphocytes produce antibodies that attack invading microorganisms
- Monocytes enlarge to become macrophages to clean up bacteria, dead cells, and other debris
- use phagocytosis to destroy bacteria/harmful substances → engulf the bacteria within the cell membrane → release enzyme to destroy itself and the target → leave behind pus
Platelets
- small cell fragments produced from stem cells in bone marrow
- essential in blood clotting
- the platelets stick to collagen fibers in the blood vessels when they break → more and more platelets stick to the fibers and clot to seal the hole → fibrinogens convert into fibrin that traps more platelets and blood cells and pull the hole close
- a dislodged clot can move through the blood vessels and block the flow of blood → blockage in the brain can cause a stroke or physical and mental disabilities
Counting blood cells
Anemia: a condition of a low erythrocyte count/a low hemoglobin level which leads to low oxygen levels
A hemocytometer is used to estimate the number of erythrocytes, leukocytes, and platelets
Ch 11.3 - Blood Vessels
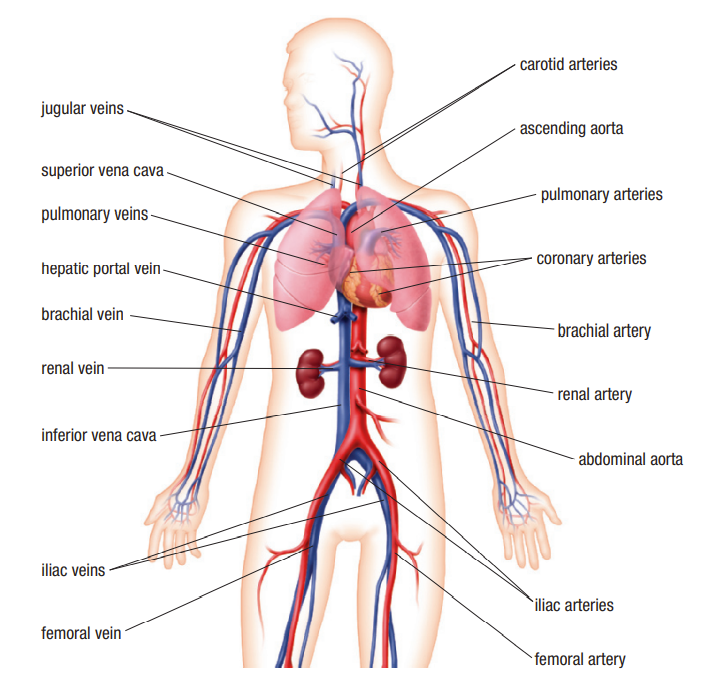
Arteries
Aorta: the largest blood vessel in the body, connected directly to the heart, the aorta branches into arteries that carry oxygenated blood to body tissues
\
An artery carries blood away from the heart toward the body’s tissues
The walls of arteries are composed of three layers
- the outer layer of connective tissue -contains elastin fibers that give the vessel elasticity → ensure the continuous flow of blood even when it’s relaxed
- the middle layer of smooth muscle
- the smooth inner layer called the endothelium
pressure increase when the ventricle contract to pump blood → arteries expand slightly → the elasticity of the outer layer allows the arteries to return to their original size → push blood farther into the downstream vessels
artery expands when blood is forced through → can be felt as a pulse if the artery is fairly large, closed to the skin, and in front of a bone
Arterioles
Arteriole: the smallest artery with smooth muscles in the walls
Since the arterioles have smooth muscles in their walls, they can be controlled by the nervous system
- signals from the nerves can regulate the diameters of the arterioles and control the blood flow to certain parts of the body
Controlling blood flow in arterioles
Vasodilation: an increase in the diameter (dilute) of arterioles that increases the blood flow to tissues
\
Vasoconstriction: a decrease in the diameter of arterioles that decreases the blood flow to the tissue
Nerve impulses cause the relaxation of smooth muscles in the arterioles → increase the diameter of blood vessels → increase the flow of blood to the skin and produce a red look
- cooling strategy - warm blood close to the surface of the skin loses thermal energy to the surrounding environment → vasodilation
Nerve impulses cause the smooth muscles in the arterioles to contract → the diameter of the blood vessel narrows → blood flow is restricted
- restricting blood flow to the skin prevents thermal energy loss to the environment
Capillaries
Capillaries are the smaller blood vessels that branch from the arteriole
Capillaries form networks of blood vessels that supply oxygen and nutrients to every cell throughout the body tissue → merge and form larger blood vessels on the opposite or venous side of the capillary network
Fluid Exchange
Differences in pressure and water concentration lead to the exchange of fluids in the capillary networks
- Arteriole - high fluid pressure on the arterial side of the capillary network → water diffuses from the blood into the tissue fluid → reduce concentration in blood, increase the concentration of dissolved substances and proteins in the blood
- Venule - concentration of water in the blood is less than the concentration of water in the tissue → remainder of the water enters the lymphatic system → maintain a balance between fluids in the circulatory system and the tissues
Controlling blood flow in capillaries
The pre-capillary sphincter muscles where capillaries branch off function as the dilation and constriction of arterioles
- blood is not needed in a particular capillary network → pre-capillary sphincter contract to reduce blood flow
- during exercise → arterioles and sphincters fully relax to allow blood flow to the muscles
Capillaries’ small diameter allows for only single file movements and decreases the rate of blood flow
millions of capillaries in a network create a total cross-section much greater than that of the arterioles and the artery
→ provides time for diffusion of substances into and out of the capillaries
Venules and Veins
Venule: the smallest vein formed by the merging of capillaries
Venules and veins carry deoxygenated blood containing CO2 and other waste products
Veins consist of
- a layer of connective tissue
- a thinner layer and less elastic middle layer of smooth muscle → internal diameter of veins is greater than that of arteries
- valve → ensure the blood flows in only one direction
- *skeletal muscles → contract to squeeze the veins → increase the pressure in the veins and pushes the blood towards the heart
Blood tends to pool in the lower extremities → lower body doesn’t move or contract enough to allow the blood to return to the heart → decrease in the circulation to the brain → faint
Veins and blood vessels become less elastic as people age → may damage the valve in the veins of the lower leg → greater accumulation of blood in the veins that don’t rebound → varicose veins
Blood pressure
Systolic pressure: the blood pressure in the arteries when the heart contracts
\
Diastolic pressure: the blood pressure in the arteries when the heart relaxes
A specific volume of blood can be accommodated within the walls of the circulatory system
- since blood vessels are elastic → some increase in blood volume can be tolerated
- the elasticity of the blood vessel walls exerts an opposite force on the blood → increasing blood pressure
Blood pressure is measured by a sphygmomanometer
cuff is inflated until the blood flow in the brachial artery is stopped,
pressure sensors detect the vibrations of the blood flowing through the artery → systolic pressure → pressure in the artery when the heart contracts
→ 120 mmHg for young adults
second reading is taken when the heart is relaxed and blood is flowing through the artery → diastolic pressure
→ 80 mmHg for young adults
→ blood pressure decreases as blood flows away from the heart to the veins and back to the heart
- greatest drop is from when the blood flows from the arteries to the arterioles and capillaries
Hypertension
Hypertension: consistent blood pressure above the range of normal values, aka high blood pressure
Factors that influence blood pressure
- diameter of the blood vessels
- the level of physical activity
- temperature
- body position
- diet
- stress
- age
- medication
Hypertension
- kidney diseases can cause more fluid to be retained in the blood → increase blood volume → increase blood pressure
- medication
- age → walls of blood vessels lose some elasticity and can’t stretch as much → pressure increases as the available volume doesn’t change
- diets high in sodium create high levels of sodium since kidneys can’t eliminate the excess → increase sodium concentration in blood → water move into the blood by osmosis → increase in blood volume and elevate the blood pressure
Hypertension forces the heart to work harder to pump blood → heart attack/stroke, rupture of blood vessels in organs
Appropriate diet, weight loss, regular exercise, or medication can reduce pressure through vasodilation or by reducing the retained water in the blood
Ch 11.4 - The Cardiac Cycle and Circulation
Structure of the Heart
Pericardium: a two-layered fluid-filled membrane that surrounds the heart and prevents friction between the heart and other tissues and organs
\
Coronary blood vessel: a blood vessel that circulates blood to and from the muscle cells of the heart
The septum separates the heart into an L and R pump, each with an atrium and a ventricle
Atria receive blood and pump it into the ventricles that pump blood out into the pulmonary circuit and the systemic circuit
- R - pulmonary circuit to the lungs
- L - systemic circuit to the rest of the body
The walls of the ventricles are much thicker than the walls of the atria → ventricles have to pump blood over a longer distance and through capillary networks
- layers of muscles in the ventricle are arranged spirally around the heart → produce a twisting motion that wrings the blood out when contracted
The heart is surrounded by two-layered connective tissues with fluids between the layer called the pericardium → protects the heart from friction with other tissues and organs in the thoracic cavity as the heart beats
The coronary blood vessels of the heart provide oxygen and nutrients to the muscle cells and remove waste products
coronary arteries branch from the aorta, coronary veins join to form the coronary sinus that empties directly into the R atrium
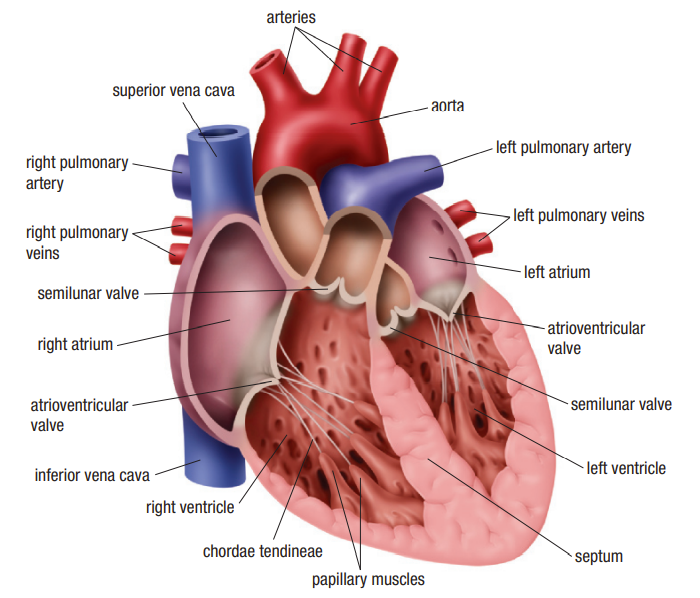
Circulation
Semilunar valve: the valve located between the L ventricle and the aorta and the R ventricle and the pulmonary arteries to prevent the backflow of blood when the ventricle relaxes
\
Atrioventricular valve: the valve located between each atrium and ventricle to prevent the backflow of blood from the ventricles to the atria\
Chordae tendineae: tendons that support the atrioventricular valves
Gas exchange
blood carries oxygen around the body → oxygen diffuses out of the blood into the cell → deoxygenated blood enters venules (that form the larger veins) → inferior and superior Vena Caca enter R atrium with blood from the body
Deoxygenated blood
R atrium → forces blood in R ventricle → contracts to force blood into the pulmonary arteries
Oxygenated blood
lungs → pulmonary veins → L atrium → contracts and squeezes blood into L ventricle → contracts and forces blood out the aorta → branch into major arteries
Four valves in the heart ensure the single-direction flow of the blood
semilunar valve: where ventricles meet pulmonary arteries and aorta - prevent blood from flowing back the ventricles when they relax
atrioventricular valve: between the atria and the ventricles - prevent the blood from flowing back to the atria through the support of chordae tendineae that are attached to papillary muscles → prevent the valve from opening backward into the atria during ventricular contraction
→ bicuspid valve (L)
→ tricuspid valve (R)
The Cardiac Cycle
Cardiac cycle: the contractions and relaxation of the heart muscle during a complete heartbeat
\
Diastole: the period of the cardiac cycle when the ventricles are relaxed, blood fills the ventricles\
Systole: the period of the cardiac cycle when the ventricles contract, blood is ejected from the ventricles
The cardiac cycle refers to a complete heartbeat with a contraction and relaxation of each chamber of the heart → occur in a specific sequence with an overlap in the various phase
Diastole: the period of relaxation and filling of the heart with blood
→ relaxed atria begin to fill with blood → pressure pushes the atrioventricular valves open → blood fills the relaxed ventricles and are filled with blood when the muscular walls of atria contracts
Systole: the period of contraction and emptying of the heart
→ the contraction of the ventricles marks the beginning of systole → increasing pressure forces the atrioventricular valve shut → blood is pushed through the semilunar valve and into the arteries → ventricle relax and increases in volume → pressure in the ventricles decrease → the semilunar valves close to prevent backflow
Heart Soundlab - the closing of the L valve
DUBB - the closing of the R valve
→ can be listened to through the stethoscope
Regulation of Heart Rhythm
Myogenic muscle: the muscle that can contract and relax without input from an external source
\
Sinoatrial node: a mass of muscle and nerve cells in the R atrium, that initiate the heartbeat and maintain the regular rhythm\
Atrioventricular node: a mass of conducting cells that transmit the signals from the SA node to the muscles of the ventricles\
Purkinje Fiber: a conducting fiber that carries the electrical signals from the AV node to the muscle cells of the ventricles\
Electrocardiograph: a device that detects the electrical activities of the heart through electrodes placed on the body’s surface
Heart muscles can contract and relax on their own without stimulation from an external source → myogenic muscle
- ensures the heart will continue to beat even if the nervous system is damaged
Heartbeat is initiated in the Sinoatrial node (the R atrium) → reaches the Atrioventricular node located in the (between R atrium and R ventricle) → Purkinje fibers run down the septum and throughout the muscle cells of the ventricle
- Sinoatrial node acts as a pacemaker that set the normal rhythm of the heartbeat
- heart rate can be adjusted by the sympathetic (nervous system that prepares for stress → increase heart rate → increases flow of blood and oxygen supply) and parasympathetic (a nervous system that conserves energy through muscle relaxation → heart rate returns to normal) nervous system
- heart rate can be affected by emotional and physical stress such as caffeine and nicotine, being overweight and physical activities
Observing and understanding the heartbeat
An electrocardiograph (ECG) is connected to the body through 12 electrodes that are sensitive to small variations in potential differences by the electrical signals in the heart → cause a marker needle to deflect and determine the strength of the current
P wave - contraction of the atria
QRS complex - electrical stimulus moves via the Purkinje fiber to the tip of the ventricle
→ the tip and upward spread - squeeze that force blood out of the aorta and pulmonary arteries
T wave - ventricles recover and prepare for the next contraction