Lecture 5: Alteration in Neurological Function
Brain Trauma:
traumatic brain injury- a traumatic insult to the brain
resulting physical, intellectual, emotional, social, and vocational changes (idk if that means it does or it can result in)
caused 50% by motor vehicle accidents, 21% falls, 29% by violence and sports
head injuries are broadly categorized into blunt and open trauma
blunt trauma (closed, nonmissile)
head strikes hard surface or a rapidly moving object strikes the head
the dura remains intact and brain tissues are not exposed to the environment
the trauma causes focal (local) or diffuse (general) brain injuries
open trauma (penetrating, missile)
injury breaks the dura and exposes the cranial contents to the environment
the trauma causes primarily focal injuries ex. weapon (idk what weapon is doing here)
coup injury
injury directly below (i think below as in below the cranium) the point of impact
objects such as a baseball bat striking the front of the head usually produce only coup injuries
contrecoup injuries
injury on the pole opposite the site of impact
objects striking the side of the head produces contrecoup injury
the injury is caused by the skull on the other side. the brain moves and collides with the hard surface of the cranium
i think for a fall or impact, the initial impact puts energy into the skull in the opposite direction (for every action there is an equal and opposite reaction and also maybe rebounding?) and then it moves and collides w the other side of the cranium). thats how i understand it at least
compound fractures
compound fractures are caused by objects striking the head with great force or by the head striking an object forcefully
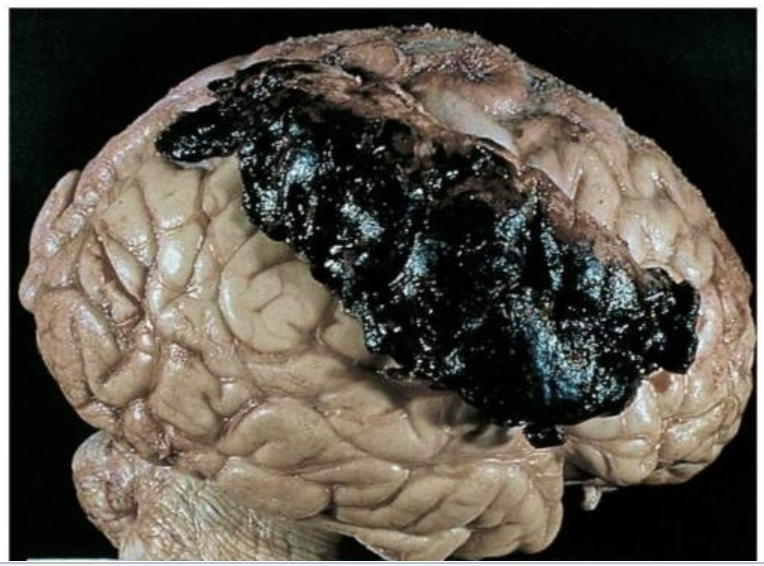
focal brain injury:
focal brain injury is specific observable brain lesion
epidural hemorrhage, subdural hematoma, and intracerebral hematoma
hemorrhage- active bleeding, hematoma- accumulated blood post (or during) active bleeding (usually once it stops or slows down)
epidural being the only hemorrhage is probably random
force of impact typically produces contusions (bruise produced by bleeding into the skin)
contusions can cause
extradural (epidural) hemorrhages or hematomas (collection of blood in soft tissue)
subdural hematomas
intracerebral hematomas

diffuse brain injury:
diffuse brain injury or diffuse axonal injury (dai) results from
shaking, inertial effort
acceleration/deceleration (ex. rotational acceleration can cause shearing, tearing, or stretching of nerve fibers that can lead to axonal damage)
axonal damage- shearing, tearing, or stretching of nerve fibers
severity of damage corresponds to the amount of shearing force applied to the brain and brain stem
dai categories:
mild concussion
classical concussion
diffuse axonal injuries (dai): mild, moderate, and severe
first 2 are categories of diffuse brain injuries (dai seems to be used a little more broadly in these slides) while the last is specifically categories of dai
mild concussion:
temporary axonal disturbances causing attention and memory deficits but no loss of consciousness
3 forms of mild concussion:
1- confusion, disorientation, and momentary amnesia (partial or total loss of memory)
2- momentary confusion and retrograde amnesia develops after 5-10 min
3- confusion w retrograde and anterograde amnesia develops after impact
classic cerebral concussion:
grade 4 (might be connected to 1,2 & 3 from the last slide bc i think theyre all grades of concussions just 4 is classic while 1-3 is mild)
disconnection of cerebral systems from the brain stem and reticular activating system
physiologic and neurologic dysfunction without substantial anatomic disruption
loss of consciousness (<6 hrs)
anterograde and retrograde amnesia
diffuse axonal injury:
produces a traumatic coma lasting more than 6 hrs bc of axonal disruption
3 forms of dai
mild- post traumatic coma hasts 6-24 hrs
moderate- actual tearing of some axons in both hemispheres
severe- involves severe mechanical disruption of many axons (extending to diencephalon)
diencephalon- part of the brain right above the brain stem, contains thalamus, hypothalamus etc.
clinical manifestation of focal brain injury:
loss of consciousness (no longer than 5 min)
loss of reflexes
results the individual to fall to the ground
cessation of respiration
bradycardia and low blood pressure
increasing in csf pressure
ecg and eec (electroencephalographic) changes
returning to full alert- minutes to days (full level of consciousness may never return)
for diagnoses ct scan and mri should be done
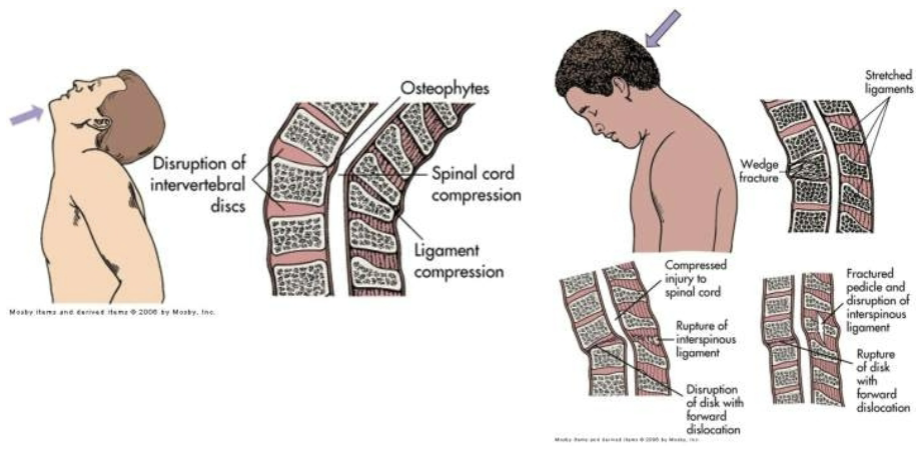
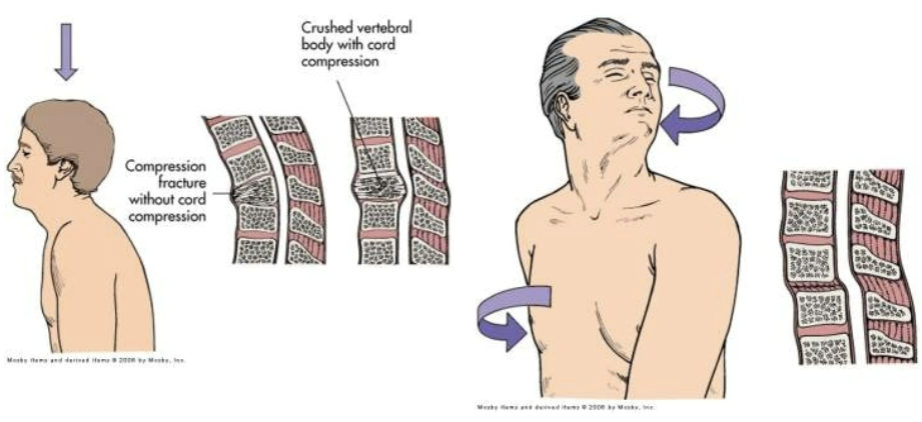
spinal cord trauma:
most commonly occurs due to vertebral injuries
vertebral injuries can be classified as
simple fracture ex. fracture of transverse or spinous process
compressed fracture ex. fracture that leads to compression of vertebral body
the vertebral body fractures which lessens its structural strength and causes it to be compressed which can put pressure on the spinal cord and surrounding nerves
comminuted (burst) fracture- vertebral body is shattered into fragments
dislocation
traumatic injury of vertebral and neural tissues are caused due to compressing, pulling, or shearing forces
most common locations: cervical (1,2 4-7) and t1-l2 lumbar vertebrae
locations reflect most mobile portions of vertebral column and the locations where the spinal cord occupies most of the vertebral canal
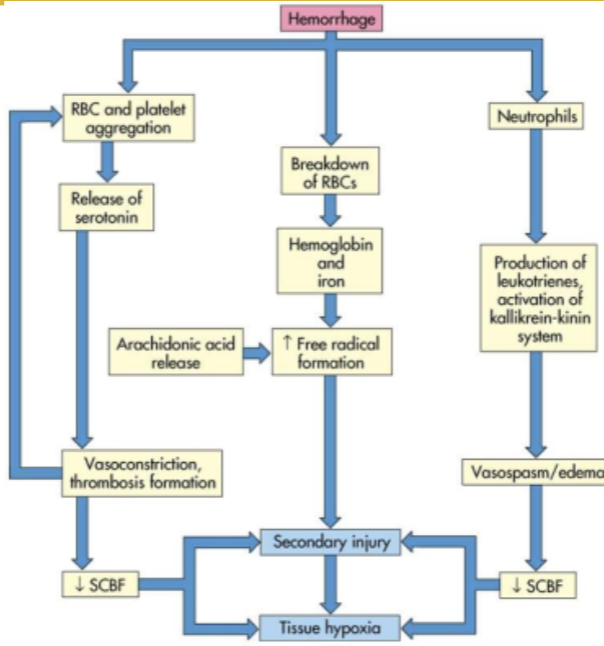
spinal shock (may last 7-20 days or more)
normal activity of the spinal cord ceases at and below the level of injury. sites lack continuous nervous discharges from the brain
complete loss of reflex function (skeletal, bladder, bowel, sexual function, thermal control, and autonomic control)
loss of motor and sensory function depends on level of injury
paraplegia
quadriplegia
autonomic hyperreflexia (dysreflexia)
massive, uncompensated cardiovascular response to stimulation of the sympathetic nervous system
stimulation of the sensory receptors below the level of the cord lesion
there are pictures of normal and dysreflexia pathways but they’re super blurry
degenerative disorders of the spine:
occur in the vertebral disk
degenerative disk disease (ddd)
common in individuals 30 and older
normally no signs functional incapacity
occurs due to biochemical and biomechanical alterations of intervertebral disk tissue
spondylolysis- degenerative process of vertebral column, associated with soft tissue
spondylolisthesis- slip of vertebra due to stress
spinal stenosis- narrowing of spinal canal ex. due to annulus
annulus fibrosis is the tough, outer layer of the intervertebral discs and if its degenerated or damaged, the inner pulpous part of the intervertebral disc can bulge or herniate out into the spinal canal (which narrows it)
(these 3 things can result from ddd)
low back pain
herniated intervertebral disk caused by trauma or degenerative disk disease
cerebrovascular disorders:
the common clinical manifestation of cerebrovascular disease is CVAs
cerebrovascular accidents (cvas) (commonly called a stroke, refers to a sudden interruption of blood flow in the brain, ‘accident’ bc it is sudden and unexpected)
thrombotic stroke
arterial occlusions caused by thrombi formed in arteries supplying the brain or in the intracranial vessels
transient ischemic attacks
embolic stroke
fragments that break from a thrombus formed outside the brain
(for both of these) i don’t think the location the clot formed is important to the classification, just whether it was the thrombus or an embolus
hemorrhagic stroke- ex. caused by hypertension
lacunar stroke- a type of ischemic stroke that happens when blood flow to a small area of the brain is blocked ex. caused by thickening of arterial wall
cerebral infarction- area of brain loses blood supply bc of vascular occlusion
cerebral hemorrhage- ex. caused by hypertension
intracranial aneurysm
may result from
arteriosclerosis
hardening/thickening of the arterial wall, can cause an aneurysm bc arteriosclerosis weakens the arterial wall bc it makes it stiffer and bulge under pressure (when it should be able to expand and contract based on blood flow), also bc it causes structural changes which can cause an imbalance of forces acting on the wall which can cause weak spots, and also bc the added layers increase the blood pressure in that area (bc narrower = increased pressure) which can add more stress to weak areas
congenital abnormalities
trauma
inflammation
infection
it is asymptomatic, but clinical manifestation may arise from cranial nerve compression
the signs vary, depending on location
diagnosis: mri, ct scan
treatment: surgery
under cva bc it can lead to an actual cva (so considered a type of cva once it leads to the stroke)
vascular malformations
symptoms include
nondescriptive chronic headache
50% experience seizure disorders caused by compression
50% experience hemorrhage (subarachnoid, subdural, or intracerebral)
diagnosis: ct scan, mri, transcranial doppler, and mra (magnetic resonance angiography)
treatment: surgery
under cva bc it can lead to an actual cva (so considered a type of cva once it leads to the stroke)
subarachnoid hemorrhage
blood escapes from defective or injured vasculature into the subarachnoid space
manifestations
headache, nausea, neck stiffness, photophobia (light sensitivity)
kernig sign- straightening the knee w the hip and knee in a flexed position produces pain in the neck and back
brudzinski sign- passive flexion of the neck produces neck pain and increase rigidity
headache:
migrane headache
trigger factors ex. stress, hunger, weather change, noise
cluster headache
several attacks can occur during the day for a periods of days followed by a long period of spontaneous remission
chronic paroxysmal hemicrania
cluster type headache that occurs with more daily frequency but w shorter duration
tension type headache
mild to moderate bilateral headache w a sensation of a tight band or pressure around the head
central nervous system tumors:
cranial tumors
primary intracerebral tumors (gliomas)
astrocytoma
oligodendroglioma
ependymoma
primary extracerebral tumors (extracerebral is outside brain but inside cranium)
meningioma
nerve sheath tumors
metastatic carcinoma
i dont think this should be under primary extracerebral tumors bc it wouldn’t really originate as extracerebral….
for both of the above primary means it starts there (so primary intracerebral originated in the brain)
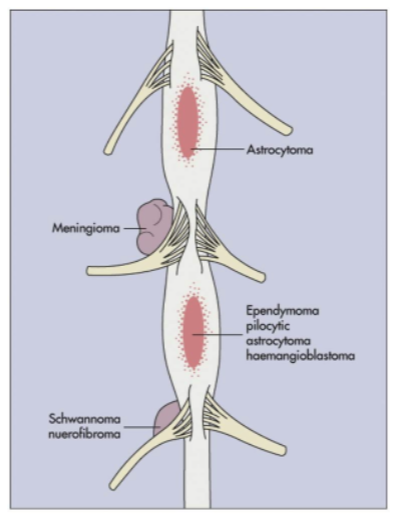
spinal cord tumors
intramedullary tumors (within the spinal cord itself)
extramedullary tumors
intradural
extradural
manifestations
compressive syndrome (spinal cord or surrounding structures is compressed)
irritative syndrome (spinal cord or nerve roots is irritated either by chemicals released, local inflammation caused by the tumor, or direct contact)
syringomyelic syndrome- inflammation of spinal cord
infection and inflammation of the cns:
cns may be affected directly by bacteria, virus, fungi, protozoa, and rickettsiae (rickettsiae are a type of bacteria but they have unique characteristics and modes of transportation)
meningitis
bacterial meningitis primarily (an) infection of (the) pia mater and (pia) archnoid
aseptic (viral, nonpurulent (no pus), (and) lymphocytic (elevated number of lymphocytes)) meningitis (aseptic here means non bacterial)
fungal meningitis
tubercular (tb) meningitis (also caused by a bacteria but bacterial meningitis listed above is probably from a different bacteria)
encephalitis
inflammation of brain tissue
acute febrile illness, usually of viral origin w nervous system involvement
most common forms of encephalitis are caused by arthropod borne viruses and herpes simplex virus
neurologic complications of aids:
human immunodeficiency associated cognitive dysfunction
hiv myelopathy (disease of the spinal cord)
hiv neuropathy
aseptic viral meningitis
opportunistic infections
cytomegalovirus infections (usually very mild symptoms unless immunocompromised)
parasitic infection
cns neoplasms (abnormal growth of tissue)
peripheral nervous system disorders:
acons traveling to and from cns can be injured
neuropathies (damage to nerves)
generalized symmetric polyneuropathies
symmetric involvement of sensory, motor, or autonomic fibers
generalized neuropathies
affect the cell body of only one type of peripheral neuron
i think polyneuropathy is a type of neuropathy that specifically affects multiple nerve types)
symptoms: muscle strength and muscle tone are affected
many neuropathies can be reversed by eliminating the cause if possible
plexus injuries
involves the nerve plexus distal to the spinal roots but proximal to the formation of the peripheral nerves
neuromuscular junction disorders:
nerve impulse at neuromuscular junction are disrupted due to
nutritional deficit, certain drugs (ex. reserpine)
certain disorders that disrupt the synthesis or packaging of neurotransmitters or release of the neurotransmitter
alterations in arousal: (as in awakeness)
can be:
strutural
divided by location above or below tentorial plate (tentorial plate separates the cerebrum and cerebellum)
metabolic
psychogenic
coma is produced by either
bilateral hemisphere damage or suppression
brain stem lesions or metabolic derangement that damages or suppresses the reticular activating system
clinical manifestations:
level of consciousness changes
pattern of breathing
posthyperventilation apnea (phva)
cheyne-stoke respirations (csr) (cyles of deep, rapid breathing followed by periods of apnea)
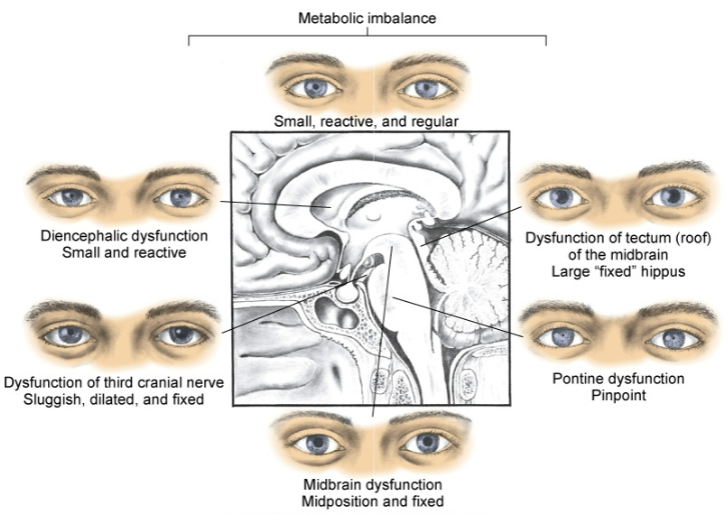
pupillary changes
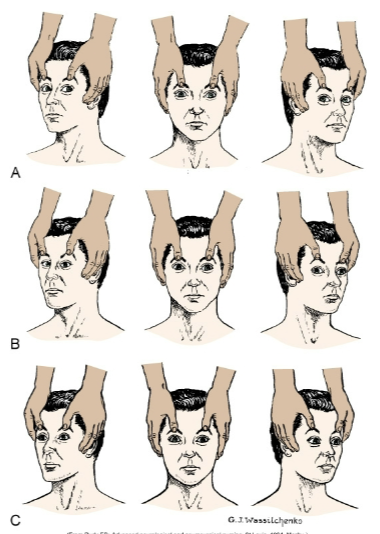
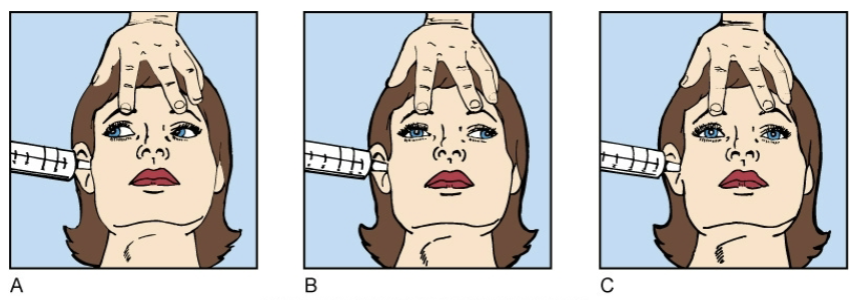
oculomotor responses (movement by the ocular muscles aka movement of the eyeball)
motor responses
vomiting, yawning, hiccups
brain death (total brain death):
body can no longer maintain internal homeostasis
brain death criteria:
completion of all appropriate and therapeutic procedures
unresponsive coma (absence of motor and reflex responses)
no spontaneous respirations (apnea)
brain death (brain stem death):
brain death criteria:
no ocular responses
isoelectric eeg (shows no detectable brain activity)
persistence 6-12 hrs after onset
cerebral death:
cerebral death (irreversible coma) is death of the cerebral hemispheres exclusive of the brain stem and cerebellum
no behavioral or environmental responses
the brain can continue to maintain internal homeostasis
survivors of cerebral death: (one of the below, not all)
remain in a coma
emerge into a persistent vegetative state
progress into a minimal conscious state (mcs)
locked in syndrome (pretty sure this can’t happen with cerebral death bc thats paralysis but still cognitively intact, at least partially; chatgpt agrees)
alterations in awareness:
selective attention
ability to select from available, competing environmental and internal stimuli
sensory inattentiveness
extinction
basically, if a person has specific damage on one side of their brain, it will be much harder to register stimulus on the physical side associated with that side of the brain. they wont be able to register (sudden) stimuli on both sides at the same time (the unaffected side will take precedence often even if the affected sides stimulus came first). They will still register one but not the other. if there is no stimulus on the unaffected side, they generally will have no issue registering stimuli on the affected side. (ex. left brain damage, if theres a loud horn honking unexpectedly on the physical left side, they wont register anything (even constant stimuli) on the physical right side)
neglect syndrome
generally associated with damage to the right hemisphere (so affecting the physical left side); both sudden and constant stimuli will be ignored (and totally unaware of its presence) on the physical side associated w the side of the brain thats damaged. this might even apply to themselves (they might neglect personal grooming on that side or even not recognize their own limbs on that side [even if they can see it])
selective attention deficit
memory
amnesia
retrograde amnesia
anterograde amnesia
executive attention deficits
adhd
image processing
seizures:
syndrome vs disease
sudden, transient alteration of brain function caused by an abrupt explosive, disorderly discharge of cerebral neurons
motor, sensory, autonomic, or psychic signs
convulsion
tonic clonic (jerky, contract relax) movements associated with some seizures
idiopathic epilepsy- no underlying cause can be found
some forms of epilepsy do have known causes
etiologic factors
cerebral lesions
biochemical disorders
cerebral trauma
epilepsy
partial seizures
simple, complex, secondary generalized
generalized seizures
absent, myoclonic (brief, shock like jerks), clonic (rhythmic jerking), tonic clonic (tonic == body stiffens), atonic (sudden loss of muscle tone which results in falling/collapsing)
unclassified epileptic seizure
aura (warning signs immediately before a seizure)
prodoma (warning signs that can occur hours or even days before a seizure)
tonic phase
contraction
clonic phase
relaxation
postictal phase
data processing deficits:
agnosia (registers sensory info but cant recognize or interpret it)
tactile, visual, auditory, etc.
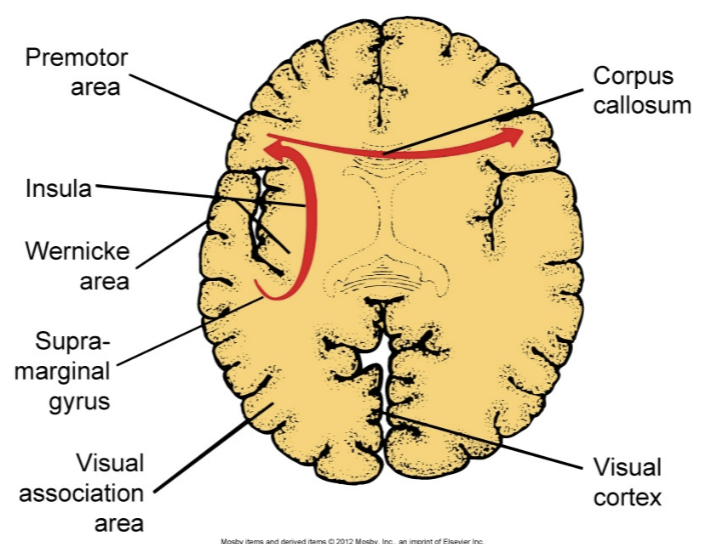
dysphasia
expressive dysphasia (difficult to speak or write coherently, words typically are said properly but either not right words or not right order. they usually know what they want to say but cant make a coherent sentence. might also struggle w word retrieval)
receptive dysphasia (difficulty understanding spoken and written language)
transcortical dysphasia (difficulty w both)
aphasia (generally a more severe or complete version of dysphasia)
acute confusional states (acs):
transient disorders of awareness that result from cerebral dysfunction
secondary to drug intoxication, metabolic disorder, or nervous system disease
delirium
hyperkinetic (excessive or abnormal movement)
hypokinetic (reduced or slower movement)
these 2 are under delirium bc delirium can cause these in specific form (ex. restlessness or lethargy)
dementia:
progressive failure of cerebral functions that is not caused by an impaired level of consciousness
losses:
orientation
memory
language
judgement
decision making
alzheimer disease (ad):
familial, early and late onset
nonhereditary (sporadic, late onset)
theories
mutation for encoding amyloid precursor protein
alteration in apolipoprotein e
loss of neurotransmitter stimulation of choline acetyltransferase
neurofibrillary tangles (abnormal aggregates of a specific protein found inside neurons; accumulation of these tangles disrupts the normal functioning of neurons)
senile plaques (aka amyloid plaques, abnormal clumps of protein that accumulate btwn neurons in the brain, disrupt cell communication and trigger inflammatory responses which leads to neuronal damage and cognitive decline)
clinical manifestations:
forgetfulness
emotional upset
disorientation
confusion
lack of concentration
decline in abstraction, problem solving, and judgement
diagnosis is made by ruling out other causes of dementia
cerebral hemodynamics:
the dynamic of blood flow in the brain, including the regulation, distribution, and alterations in cbf
cbf (cerebral blood flow)
cpp (cerebral perfusion pressure)
cbv (cerebral blood volume)
cerebral oxygenation
increased intracranial pressure (iicp):
normal 5-15mmHg
caused by an increase in intracranial content
tumor growth, edema, excessive csf, or hemorrhage
stage 1
the body can compensate for iicp, may not have noticeable symptoms but may experience slight changes in consciousness or subtle neurological signs. cerebral perfusion is maintained
stage 2
compensatory mechanisms start to fail, symptoms: slight changes in mental status (ex. confusion or lethargy), decrease in the ability to maintain normal blood flow to the brain etc. may be increased blood pressure (to try to maintain normal brain perfusion)
stage 3
significant elevation of icp leading to reduced cerebral perfusion. symptoms: altered level of consciousness, severe headache, pupillary changes, abnormal posturing (body positioning) etc. risk of brain herniation increases
stage 4
most critical stage, often referred to as herniation, there is a life threatening increase in icp that leads to brain herniation and severe neurological impairment. symptoms: coma, loss of reflexes, cardiovascular instability etc.
herniation syndromes:
supratentorial herniation:
uncal
uncus (small structure on the medial surface of the temporal lobe) or hippocampal gyrus (or both) shifts from the middle fossa through the tentorial notch into the posterior fossa
central
downward shift of the diencephalon (region of the brain btwn the cerebral hemispheres and the brainstem) through the tentorial notch
cingulate
congulate gyrus (a curved fold of brain tissue above the corpus callosum) shifts under the falx cerebri (a fold of dura mater)
infratentorial herniation:
cerebellar tonsil shifts through foramen magnum
cerebral edema:
increase in the fluid (intracellular or extracellular) within the brain
types
vasogenic (increased permeability of the blood brain barrier)
cytotoxic (swelling of brain cells from an influx of water bc of cellular injury or metabolic dysfunction)
interstitial (accumulation of csf)
hydrocephalus:
excess fluid within the cranial vault, subarachnoid space, or both
caused by interference in csf flow
decreased reabsorption
increased fluid production
obstruction within the ventricular system
noncommunicating hydrocephalus (aka obstructive hydrocephalus; happens when there is a blockage in the flow of csf in the ventricles)
internal (blockage is in the ventricles, cant flow btwn ventricles)
intraventricular (accumulation in the ventricles)
communicating (extraventricular) hydrocephalus (csf can flow btwn ventricles but cant be properly reabsorbed into the bloodstream)
acute hydrocephalus
normal pressure hydrocephalus
alterations in neuromuscular function:
muscle tone
hypotonia (decreased muscle tone, floppiness or reduced resistance to passive movement)
hypertonia
spasticity (tightness and resistance to movement)
gegenhalten (paratonia) (resistance to passive movement that occurs in response to the external force, the muscle tone increases once the force is applied)
dystonia (involuntary muscle contractions)
rigidity
alterations in movement:
paresis (partial weakness or reduced strength) and paralysis
upper motor neuron syndromes
hemiparesis or hemiplegia
diplegia
paraparesis or paraplegia
quadriparesis or quadriplegia
pyramidal motor syndromes (results from damage to the pyramidal tracts [pathways in the brain that control voluntary movement])
spinal shock (temporary paresis/paralysis)
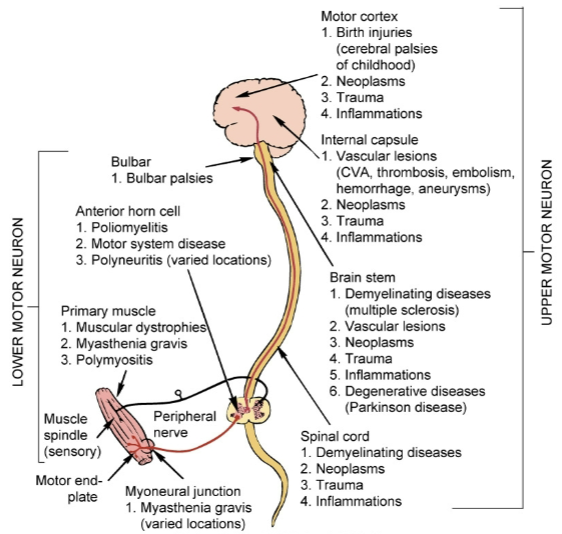
lower motor neuron syndromes
flaccid paresis or flaccid paralysis
hyporeflexia (reduced or diminished reflex responses) or areflexia (no reflex responses)
fibrillation (spontaneous, irregular contractions of individual muscle fibers)
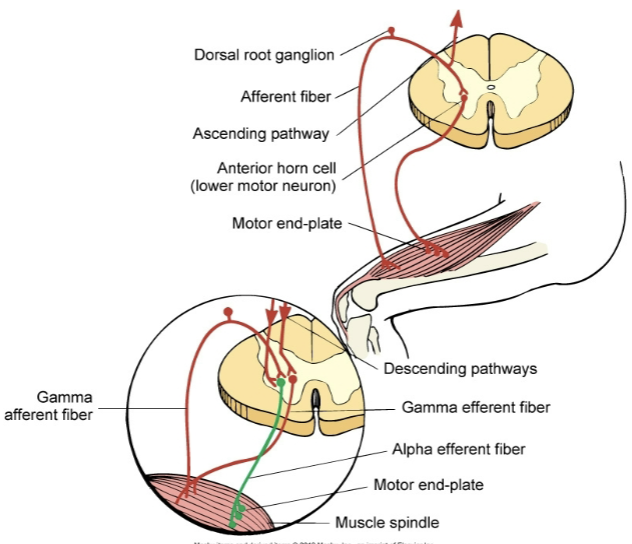
amyotrophies (degeneration and atrophy of muscle tissue from loss of motor neurons)
paralytic poliomyelitis
infectious disease caused by polio virus, leads to inflammation of spinal cord and motor neurons, can result in paralysis and muscle weakness
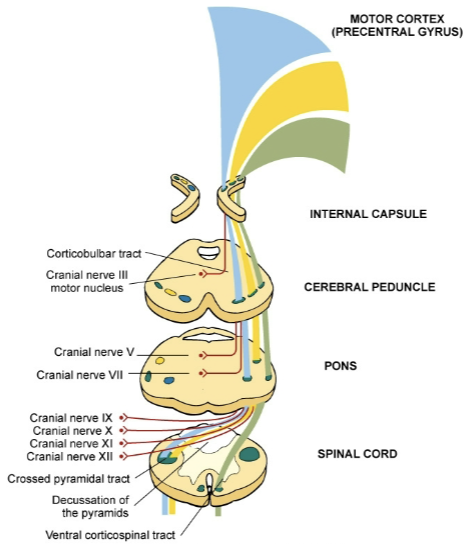
nuclear palsies
disorders that result from damage to the cranial nerve nuclei in the brainstem (leading to deficits in the functions controlled by those nerves)
guillain barre syndrome
autoimmune disorder attacking the peripheral nervous system
progressive bulbar palsy
causes degeneration of the bulbar region (part of the brain stem) which leads to progressive weakness and atrophy of the muscles innervated by cranial nerves
bulbar palsy
like progressive bulbar palsy but results from conditions like stroke or trauma, symptoms either stabilize or improve rather than progressively worsen
hyperkinesia
excessive movement
chorea (involuntary, irregular, unpredictable muscle movements), wandering, tremor at rest
postural tremor etc.
paroxysmal dyskinesias
dyskinesia- sudden, involuntary, abnormal movements
paroxysm- a sudden, intense episode or attack of a condition or symptom
tardive dyskinesia
tardive- delayed or late onset of symptoms; in this specific context- dyskinesia that develops after prolonged exposure to certain meds
huntington disease
also known as chorea
autosomal dominant hereditary degenerative disorder
severe degeneration of the basal ganglia (caudate nucleus [a part of the basal ganglia]) and frontal cerebral atrophy
depletion of gamma-aminobutyric acid (gaba)
hypokinesia
decreased movement
akinesia
bradykinesia (slowed movement)
loss of associated movement
parkinson disease:
severe degeneration of the basal ganglia (corpus striatum) involving the dopaminergic nigrostriatal pathway
parkinsonian tremor, rigidity, bradykinesia
postural disturbances
autonomic and neuroendocrine symptoms
congitive affective symptoms
secondary parkinsonism (parkinsons symptoms from something else thats not parkinsons)
disorders of posture (stance):
dystonia (involuntary muscle contractions resulting in abnormal postures, twisting movements, or repetitive motions)
dystonic postures and movements
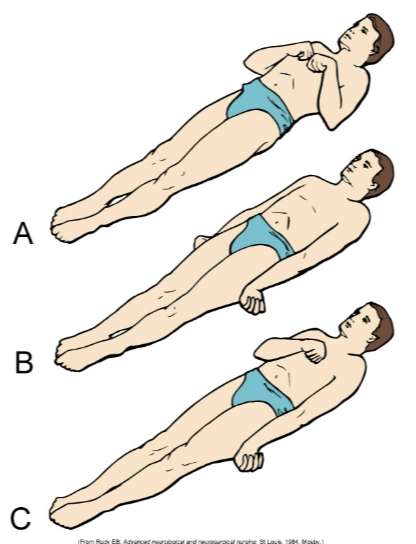
decorticate posture (A; also legs are turned in)
decerebrate posture (B, also back is arched)
basal ganglion posture (stiff/rigid limbs, flexed posture of limbs, stooped/leaning forward trunk)
senile posture (forward flexed trunk, rounded shoulders, slight flexion of hips and knees)
disorders of gait:
spastic gait (stiff/jerky movements, tendency to drag 1/both legs, reduced arm swing on affected side, difficulty w balance/coordination)
scissors gait (legs cross/scissor when walking, narrow base of support, short steps, hypertonia in legs)
base of support: the area beneath a person that supports their weight, determined by the distance btwn their feet when standing/walking
cerebellar gait (unsteady/wide based walking, difficulty w balance, lurching/swaying movements, frequent stumbling/falling)
basal ganglion gait (reduced arm swing, shuffling steps w a short stride length, difficulty initiating movements [freezing], stooped posture)
senile gait (slow/shuffling steps, broad base of support, reduced arm swing, difficulty w balance/coordination)
disorders of expression:
hypermimesis (exaggerated expressions of emotions)
hypomimesis (reduced expressions of emotions)
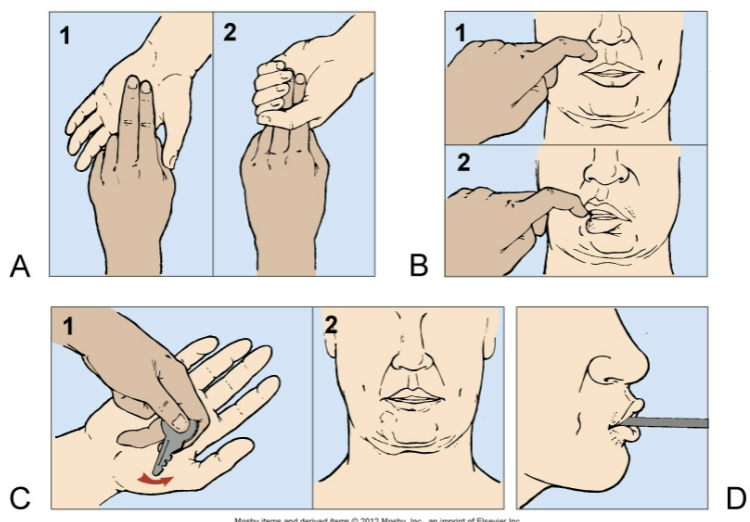
dyspraxias and apraxias (difficulty [dys]/inability [a] planning and executing coordinated movements)
extrapyramidal motor syndromes:
dysfunction of the extrapyramidal system which is part of the motor control pathway in the brain
basal ganglia motor syndromes (caused by dysfunction of the basal ganglia, results in bradykinesia, hypertonia, tremors [specifically resting tremors which happen when not moving the limb], dystonia, chorea etc.)
cerebellar motor syndromes (caused by dysfunction of the cerebellum, results in ataxia, dysmetria, tremors [specifically intention tremors which happen when trying to move the limb], hypotonia, difficulty w balance/posture etc.)
ataxia- lack of coordination and unsteady movements
dysmetria- inability to the control the distance/range of movements