Chapter 18 - The Circulatory System: Blood
18.1 General Aspects of Blood
The circulatory system consists of the heart, blood vessels, & blood
The term cardiovascular system refers only to the heat & vessels
The Purposes of Blood Circulation
Fundamental purpose of the circulatory system is to transport substanes from place to place
Functions include:
Transport
Blood carries oxygen from the lungs to all of the body’s tissues, while it picks up carbon dioxide from those tissues & carries it to the lungs to be removed from the body
Picks up nutrients from the digestive tract and delivers them to all of the body’s tissues
Carries metabolic wastes to the kidney fro removal
Carries hormones from endocrine cells to their target organs
Transports a variety of stem cells from the bone marrow and other origins to the tissues where they lodge and mature
Protection
Blood plays several roles in inflammation, a mechanism for limiting the spread of infection
WBCs destroy microorganisms & cancer cells and remove debris from the tissues
Antibodies and other blood proteins neutralize toxins and help to destroy pathogens
RBCs bind foreign antigens and transport them to liver and spleen for disposal
Platelets secrete factor that initiate blood clotting and other processes for minimizing blood loss, and contribute to tissue growth and blood vessel maintenance
Regulation
By absorbing or giving off fluid under different conditions, blood capillaries stabilize fluid distribution in the body
By buffering acids and bases, blood proteins stabilize pH of the extracellular fluids
cutaneous blood flow is extremely important in dissipating metabolic heat from the body. Shifts in blood flow regulate body temperature by routing blood to the skin for heat loss or retaining in deeper in the body to conserve heat
usually from protiens
Components and General Properties of Blood
4-6 liters in human adult
liquid connective tissue
composed of an extracellular matrix
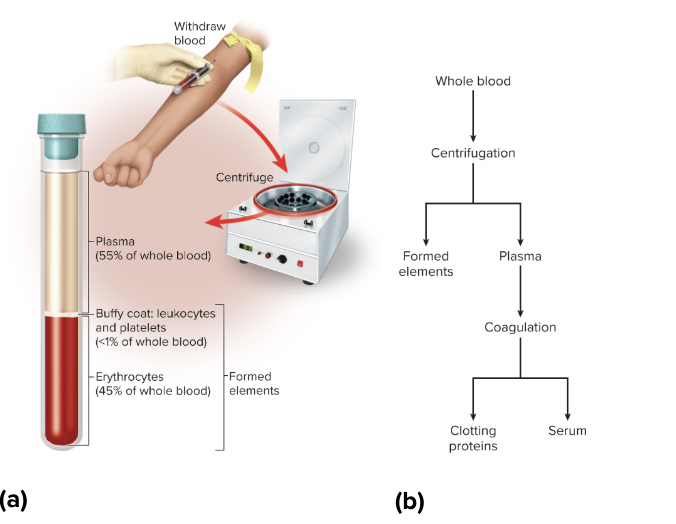
Plasma: a clear light yellow fluid constituting a little over half of the blood volume
Suspended in the plasma are the formed elements-cells and cell fragments including RBCs, WBCs, & platelets
they are called formed elements as they are contained by a plasma membranes
The formed elements are classified as follows:
Erythrocytes (RBCs)
Leukocytes (WBCs)
Granulocytes
Neutrophils (5 lobed nucleus)
Eosinophils
Basophils
Agranulocytes
Lymphocytes
Monocytes
Platelets (not cells) - fragments of cells found in bone marrow
Blood fractionation: the separation of blood into its basic components, is based on centrifugation and coagulation
serum = coagulated serum
RBCs or erythocytes are the densest elements & settle to the bottom
General Properties of Blood
pH: 7.35-7.45
Hematocrit (packed cell volume):
Females: 36% to 48%
Males: 41% to 53%
Hemoglobin:
Female: 11-16 g/dL
Male: 14-18 g/dL
RBC count:
Female: 4.2-5.4 million/μL
Male: 4.6-6.2 million//μL
Platelet count: 130,000-360,000/μL
Total WBC count: 5,000-10,000/μL
0.9% saline in blood plasma,
Blood Plasma
complex mixture water, proteins, nutrients, electrolytes, nitrogenous wastes, hormones, and gases
Albumin is the smallest and most abundant plasma protein
it serves to transport various solutes and buffer the pH of blood plasma
contributes two physical properties
viscosity & osmotic pressure
Globulins are divided into three subclasses from smallest to largest
Alpha - Beta - Gamma globulins
Play various roles in solute transport, clotting, and immunity
Fibrinogen: sticky protein that forms the framework of a blood clot
Composition of Blood Plasma
Nutrients
Glucose (dextrose): 70-110mg/dL
Electrolytes
Sodium: 135-145 mEq/L
Calcium: 9.2-10.4 mEq/L
Potassium: 3.5-5.0 mEq/L
Chloride: 100-106 mEq/L
Bicarbonate: 23.1-26.7 mEq/L
Nitrogenous Wastes
Urea: 10-20 mg/dL
Creatinine: 0.6-1.5 mg/dL
Nitrogenous wastes
toxic end products
most abundant is urea
Blood Viscosity & Osmolarity
viscosity is the resistance of a fluid to flow, resulting from the cohesion of its particles
simply, it is the thickness or stickiness of a fluid
whole blood is 4.5 to 5.5 more vicious than water, plasma alone is 2 times more viscous than water
viscosity governs the flow of blood through the blood vessels
osmolarity refers to the total concentration of solute particles. The rate of transfer of fluid between
The movement of fluid in the capillaries and tissues depends mainly on their relative osmolarity between the two
The osmolarity of the blood is mainly a product of the sodium and protein concentration and the number of RBCs called the Colloid Omnotic Pressure
How Blood Is Produced
Everyday, an adult typically produces 400 million platelets, 200 billion RBCs, and 10 billion WBCs
In animals that produce eggs, embryonic hematopoiesis occurs in the yoke sac
there, Blood islands produce primitive stem cells that migrate to the bone marrow, liver, spleen, & thymus
from infancy, the red bone marrow produced all 7 kinds formed elements while lymphocytes are produced in lymphoid tissue, especially the thymus, tonsils, lymph nodes, spleen, and mucous membranes
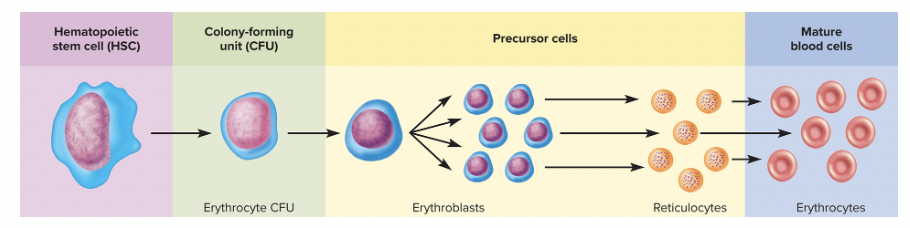
All formed elements trace their origins to these hematopoietic stem cells (HSC)
HSCs maintain a small but persistent population in the bone marrow
some become colony forming units (CFUS) which are destined to produce one or the other of the formed units
18.2 Erythrocytes
Erythrocytes or RBCs
Have two principal functions:
pick up oxygen from the lungs and deliver it to tissues elsewhere
pick up carbon dioxide from the tissues and unload it in the lungs
Erythrocyte Form and Function
RBCs are discoidal cells with a biconcave shape, a thick rim and a thing shrunken center
speculate that it maximizes surface area to volume thereby promoting quick diffusion
Diameter of 7.5 micrometer
RBCs lose their nucleus and organelles during maturation
Rely on anaerobic fermentation to produce ATP, hence do not consume O2 they transport
Their cytoplasm consists mainly of a solution of 33% hemoglobin, a red pigment about 280 molecules per cell
The cytoplasm contain carbonic anhydrase which catalyzes the reaction CO2 + H2O >< H2CO3
The glycolipids in the plasma membrane determine the blood type
On its inner surface two cytoskeletal proteins, spectrin and actin, give the membrane resilience & durability
allows RBC to stretch, bend, & fold through small capillaries an then spring back into shape
Hemoglobin
Hemoglobin consists of four protein chains called globins
Two of them, alpha, the other two beta
Fetal hemoglobin (HbF) has two gamma chains in place of beta chains
HbF binds oxygen more tightly than HbA (adult hemoglobin) does; this enables the fetus to extract oxygen from the mother’s bloodstream
Quantities of Erythrocytes and Hemoglobin
Hemocrit: packed cell volume, the percentage of whole blood volume
Values tend me be lower in women than in men because
androgens stimulate RBC production, and men have higher androgen levels than women
most women of reproductive age have periodic menstrual losses
the hemocrit is inversely proportional to percentage body gat, which is greater in women than in men on average
The Erythrocyte Life History
Erythropoiesis begins with a HSC becomes an erythrocyte colony-forming unit (CFU) with receptors for erythropoietin (EPO) , a hormone secreted by the kidneys
EPO stimulates the CFU to transform into an erythroblast which multiply, build up a large cell population and being to synthesize hemoglobin
The erythroblast’s nucleus shrivels and is exuded through the plasma membrane…the resulting cell is now called a reticulocyte
Reticulocytes enter the circulation, and the polyribosomes (which give the recticulocyte its name) disintegrate, the cell now becoming a mature RBC
reticulocytes normally constitute 0.5 to 1.5% of circulating RBCs. Blood loss would lead to an increase in the reticulocyte count
Reticulocytes do not have nucleus
Erythrocyte Homeostasis
RBC count is maintained in a classic negative feedback amnner
If the RBC count drops, it can result in hypoxemia
People who live in places with high elevations will tend to have higher RBC counts than those who live in places of lower elevation.
This is because of the lower O2 level
Iron Metabolism
iron is a critical part of the hemoglobin molecule
Men and women lose iron at different levels
Men: 0.9 mg
Female (of reproductive age): 1.7mg
Erythrocyte Death & Disposal
RBCs die in the spleen
Hemolysis, the rupture of RBCs, releases hemoglobin and leaves empty plasma membranes
The membranes are digested by macrophages in the liver and spleen
Macrophages will begin the disposal process by separating the heme from the globin
They will hydrolyze the globin into free amino acids which can be metabolized as fuel or recycled for protein synthesis
Heme must have its iron removed by the macrophage which then converts the rest to biliverdin which is further converted into bilirubin
bilirubin makes people look jaundice
Erythrocyte Disorders
Primary Polycythemia
RBC excess d/t cancer of the erythropoietic line of the red bone marrow
Secondary polycythemia
characterized by RBC counts as high as 6 to 8 million RBCs/uL
most often caused bby smoking, air pollution, emphysema, high alt., excesive aerobic exercise, or other factors that create a state of hypoxia
Anemia
Three categories
inadequate erythropoiesis
iron-deficiency anemia
Hemorrhagic anemia
hemophilia
hemolytic anemia
SC, penicillin allergy, malaria
SC
Hereditary disease, recessive gene
a single amino acid change in the beta chains of hemoglobin
HbS does not bind to O2 as well as HbA
SC are sticky and tend to agglutinate, especially in low O2 situations
The clumping blocks vessels leading to joint pain, stroke, heart failure
SC disease verses SC trait
survival advantage
for those with sickle cell trait in the areas of the world with malaria-protects them from the disease, likely the reason the gene persists
18.3 Blood Types
Overview
Ancient Greek physicians attempted to transfuse blood from one person to another by squeezing it from a pig’s bladder through a porcupine quill into the recipient’s vein
Karl Landsteiner discovered blood types A, B, and O in 1900
Blood types related to surface antigens
all cells have surface antigens
an antigen is a complex molecule made up of proteins, glycoproteins, and glycolipids, unique to everyone
They are present to identify self, against foreign antigens
If foreign antigen is detected, an immune reaction occurs leading to the development of an antibody against the foreign antigen
The antigen-antibody complex then leads to an immune reaction to rid the body of the foreign substance
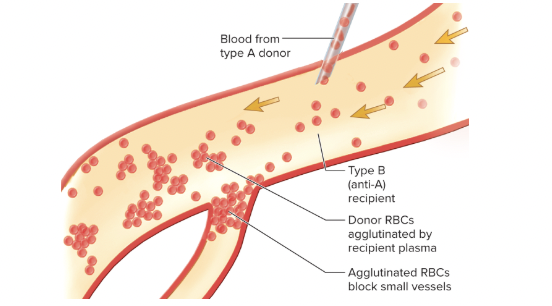
In the case of RBCs, the reaction an agglutination reaction
in which each antibody molecule binds to two or more foreign cells and stick them together - repetition of this process produced large clumps of cells that can cause complications of the transfusion reaction
Being transfused with mismatched blood will lead to this reaction, and if severe enough, can lead to death
The ABO Group
Formed by A, B, and O
Determined by the hereditary presence or absence of antigens A and B on the RBCs
A person’s ABO blood type can be determined by placing one drop of blood in a pool of anti-A serum and another drop in a pool of anti-B serum.
AB exhibits conspicuous agglutination in both antisera
type A or B agglutinates only in the corresponding antiserium
Type O does not agglutinate in either

Type O is the most common while AB is the rarest
universal donor Type O
universal recipient Type AB
In transfusions, it is imperative that the donor’s RBCs not agglutinate as they enter the recipients bloodstream
The Rh Group
Named for the rhesus monkey
genotype DD or Dd are considered Rh-positive (Rh+) and those that lack the antigen (dd) are Rh-negative (Rh-)
Also O+ for Rh+ or for AB-, Rh-
Other Blood Groups
Duffy, Kell, Kidd, Lewis, and MNS
These rarely cause transfusion reaction but useful for legal purposes as paternity and criminal cases
Maternal-Fetal Mismatches
Hemolytic disease of the newborn (HDN) or erythroblastosis fetalis
Occurs when a woman has a baby with a mismatched blood type-most famously when she is Rh- and carries Rh+
First pregnancy normal
Second pregnancy she produced antibodies and if she becomes pregnant again with an Rh+ fetus, those antibodies can pass through the placenta and agglutinate the fetal erythrocytes, thus the baby is born with hemolytic anemia
18.4 Leukocytes
Overview
Least abundant of the formed elements
WBC count of 5000 to 10000 WBCs per microliter
However, a large percentage of WBC exist outside the circulatory system, in various tissues. They enter and leave the blood
They are different from RBCs in that they retain their nucleus and organelles
All WBCs have granules in their cytoplasm, and their staining differentiates the varius types of WBCs
Two types of WBCs have no granules, called agranlocytes, lymphocytes, and monocytes
Types of Leukocytes
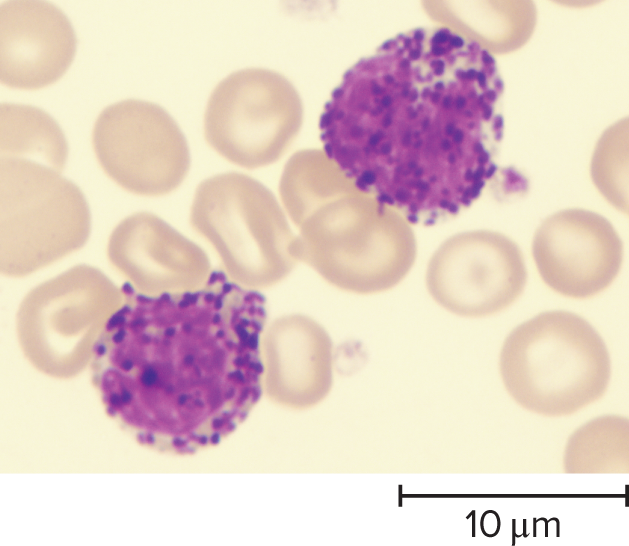
Granulocytes
neutrophils, eosinophils, & basophils'
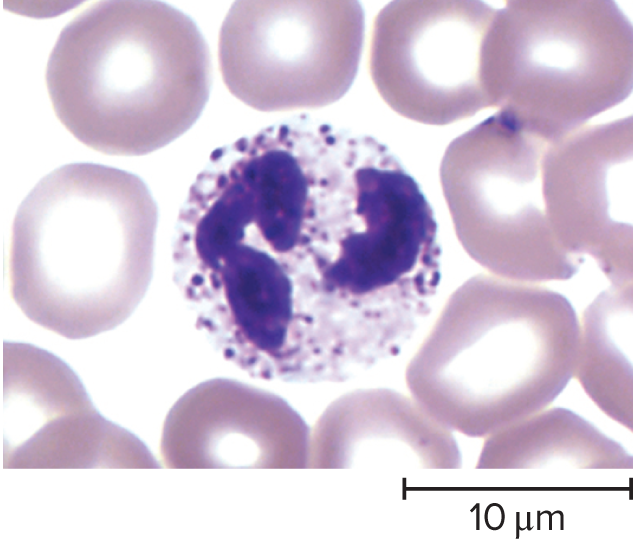
Neutrophils
60 to 70% of leukocytes
has 4 to 5 lobed nucleus
absolute count around 4100
increase in bacterial infections
phagocytize bacteria
release antimicrobial chemicals
Basophils
<0.5% of WBCs
Large U shaped or S shaped nucleus
coarse large blue to violet granules in cytoplasm
increase in chickenpox, sinusitis, diabetes, myxedema, and polycythemia
secretes histamine which dilates blood vessels, and heparin and anticoagulant and promotes movement of other WBCs and prevents clumping
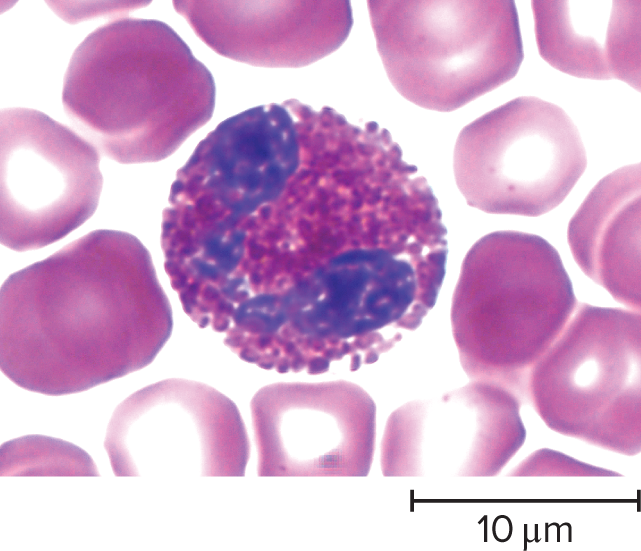
Eosinophil
2% to 4% of WBC count
nucleus usually has two large lobes connected by thin strand
increases in parasitic infections, allergies, collagen diseases, and diseases of spleen and CNS
release enzymes that weaken or destroy parasites such as worms
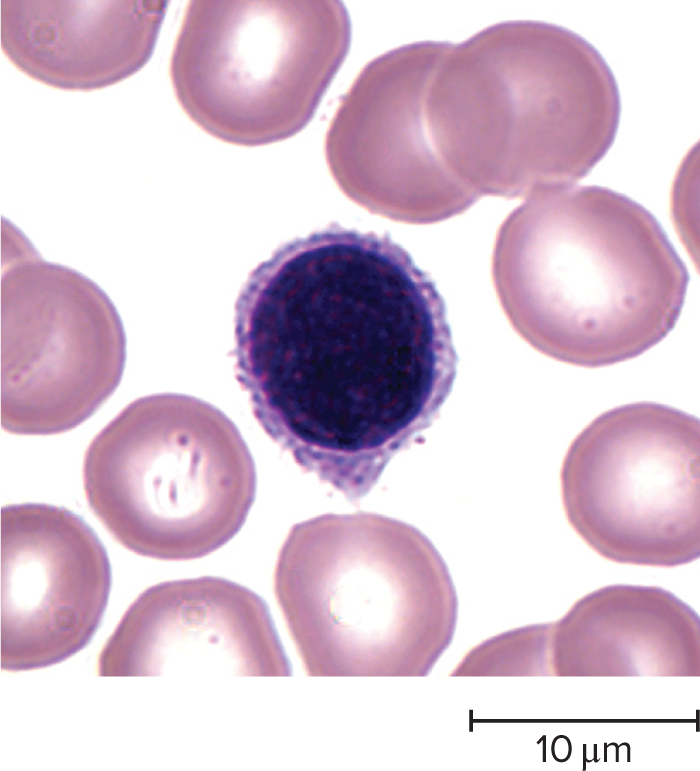
Lymphocytes
25-33% WBC count
small in diameter, a little larger than RBCs
nucleus is large and fills most of the cell
increases in diverse infections, destroys cancer cells, foreign cells, and infected cells
coordinates actions of other immune cells
secretes antibodies
serve in immune memory
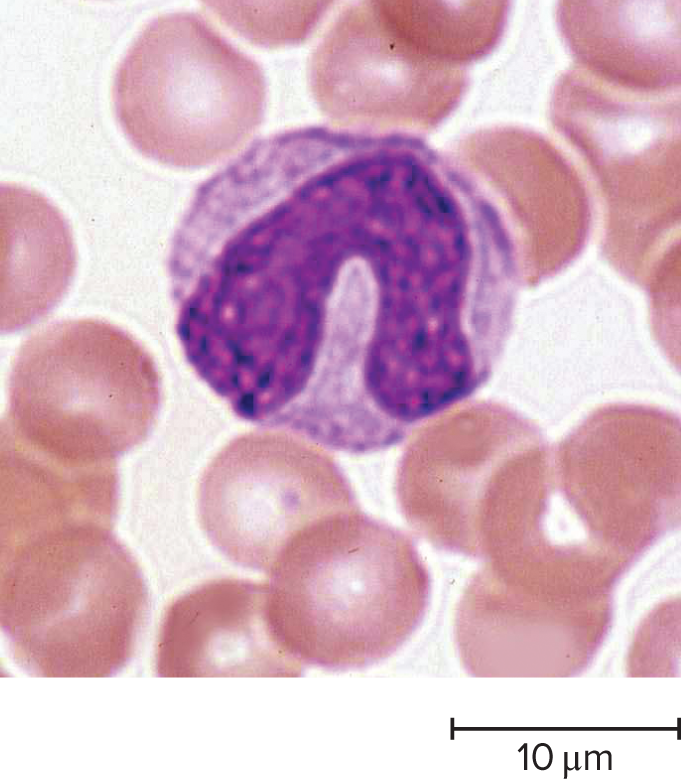
Monocytes
3%-8% of WBCs nucleus avoid or horseshoe shape
abundant cytoplasm with sparse nonspecific granules
increase in viral infections and inflammation
differentiate into macrophages, phagocytize pathogens, dead neutrophils and other dead cells
Present antigens to activate other cells of the immune system
Leukocyte Life History
Leukopoiesis production of WBC begins with hematopoietic stem cells
Myleoblasts → granulocytes
Monoblasts → monocytes
Lymphoblasts → produce all lymphocyte types
Leukocyte Disorders
WBC below 5,000 is called Leukopenia
seen in lead, arsenic, and mercury poisoning
WBC count above 10,000 is called leukocytosis
usually indicated allergy, infection, or other diseases
Leukemia
cancer of hematopoietic tissues that usually produces an extraordinarily high number of circulating leukocytes and their precursors
Classified as Myeloid or Lymphoid and Acute or Chronic
Myeloid Leukemia is marked by uncontrolled granulocyte production
Lymphoid Leukemia involved uncontrolled lymphocyte or monocyte production
Acute Leukemia appears suddenly, progresses rapidly, and causes death w/in few months
Chronic Leukemia develops more slowly and may undergo undetected for months to years
18.5 Platelets and the Control of Bleeding
Platelet Form and Function
are not cells but fragments of marrow cells called megakaryocytes
normal platelet count is 130,000 to 400,000 platelets
the count can vary under different circumstances
platelets contain lysosomes, mitochondria, granules filled with platelet secretions, microfilaments, and granules; and a system of channels called the Open Canalicular system which opens onto the platelet surface

Functions of Platelets:
secrete vasoconstrictors, chemicals that stimulate spasmodic constriction of broken vessels and help to reduce blood loss
stick together to form temporary platelet plugs that seal small breaks in injured blood vessels
secrete procoagulants, or clotting factors, which promote the formation of blood clots more durable than platelet plugs
initiate the formation of clot-dissolving enzyme that dissolves blood clots that have outlasted their usefulness
secrete chemicals that attract neutrophils and monocytes to sites of inflammation
they internalize and destroy bacteria
secrete growth factors that stimulate mitosis in fibroblasts and smooth muscle and thereby help to maintain and repair blood vessels
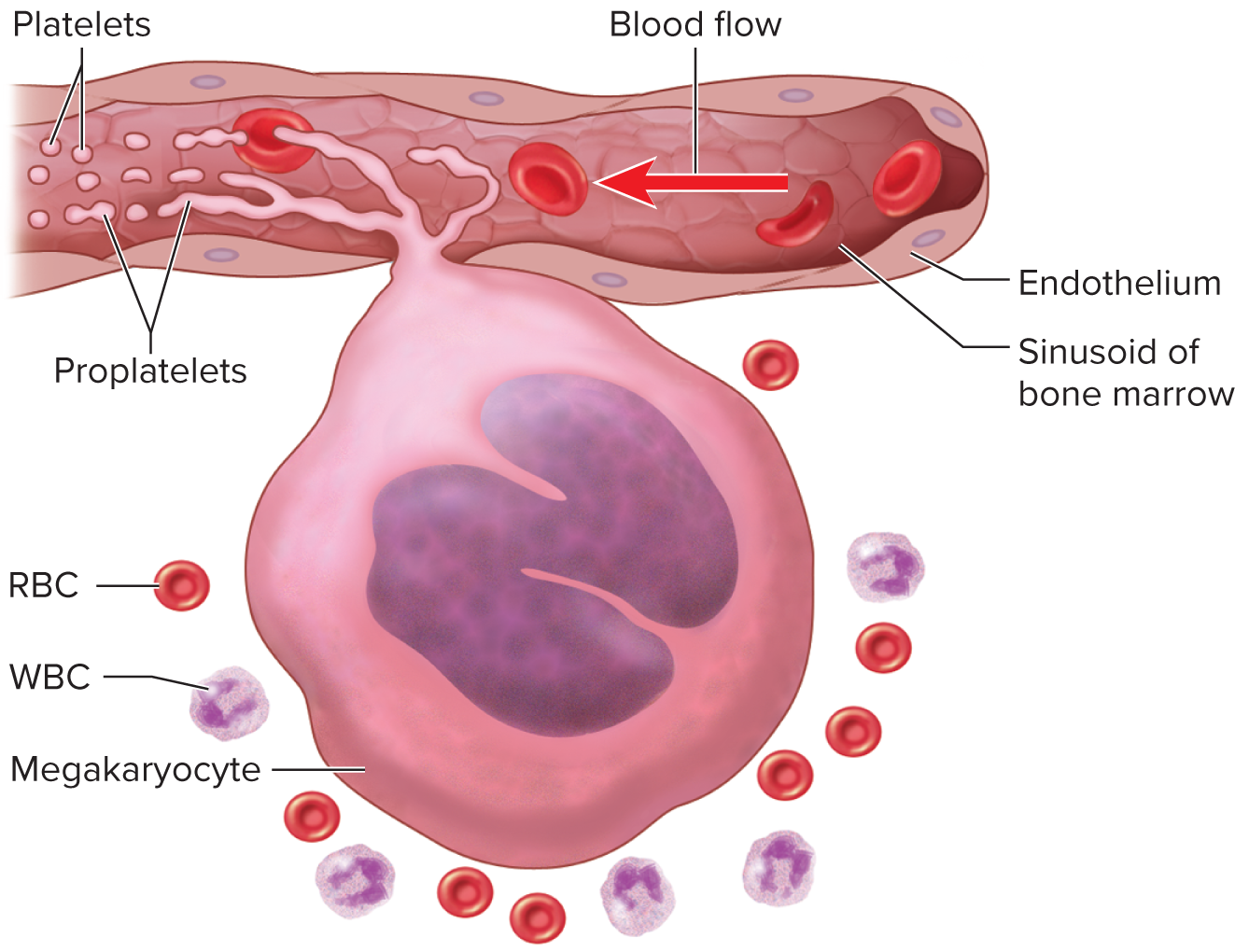
Platelet Production
The production of platelets is called thrombopoiesis
It is stimulated by a hormone from the liver and kidneys called thrombopoletin
Under its influence hscs become megakaryoblasts
It duplicates itself to become a megakaryocyte
They are gigantic cells, up to 150 micrometers in diameter
Most live in the bone marrow adjacent to blood-filled spaces called sinusoids
It sprouts long tendrils called proplatelets that protrude through the endothelium, which breaks off pieces that become platelets
More platelets leave the lung that proplatelet enter
Circulation lifespan is 5 to 6 days
25 to 40% of platelets are stored in the liver
Hemostasis
Three hemostatic mechanisms
vascular spams, platelet plug formation, and blood clotting
Vascular spasm
protection against blood loss
prompt constriction of broken vessel
triggered by injury which stimulate pain receptors
Platelet Plug Formation
When a vessel is broken, collagen fibers of its wall are exposed to the blood - contact with collagen or other rough surfaces, platelets grow long spiny pseudopods that adhere to the vessel and to other platelets creating a large mass of cells
This mass is called the platelet plug
Coagulation
Objective is to convert the plasma protein fibrinogen into Fibrin, a sticky protein that adheres to the walls of a vessel
Extrinsic Mechanism
initiated by clotting factors released by the damaged blood vessel and perivascular tissues
comes form external forces to the blood itself
intrinsic mechanism
only uses clotting factors found in the blood itself
Reaction Cascade
a series of reactions, each of which depends on the product of the preceding one.

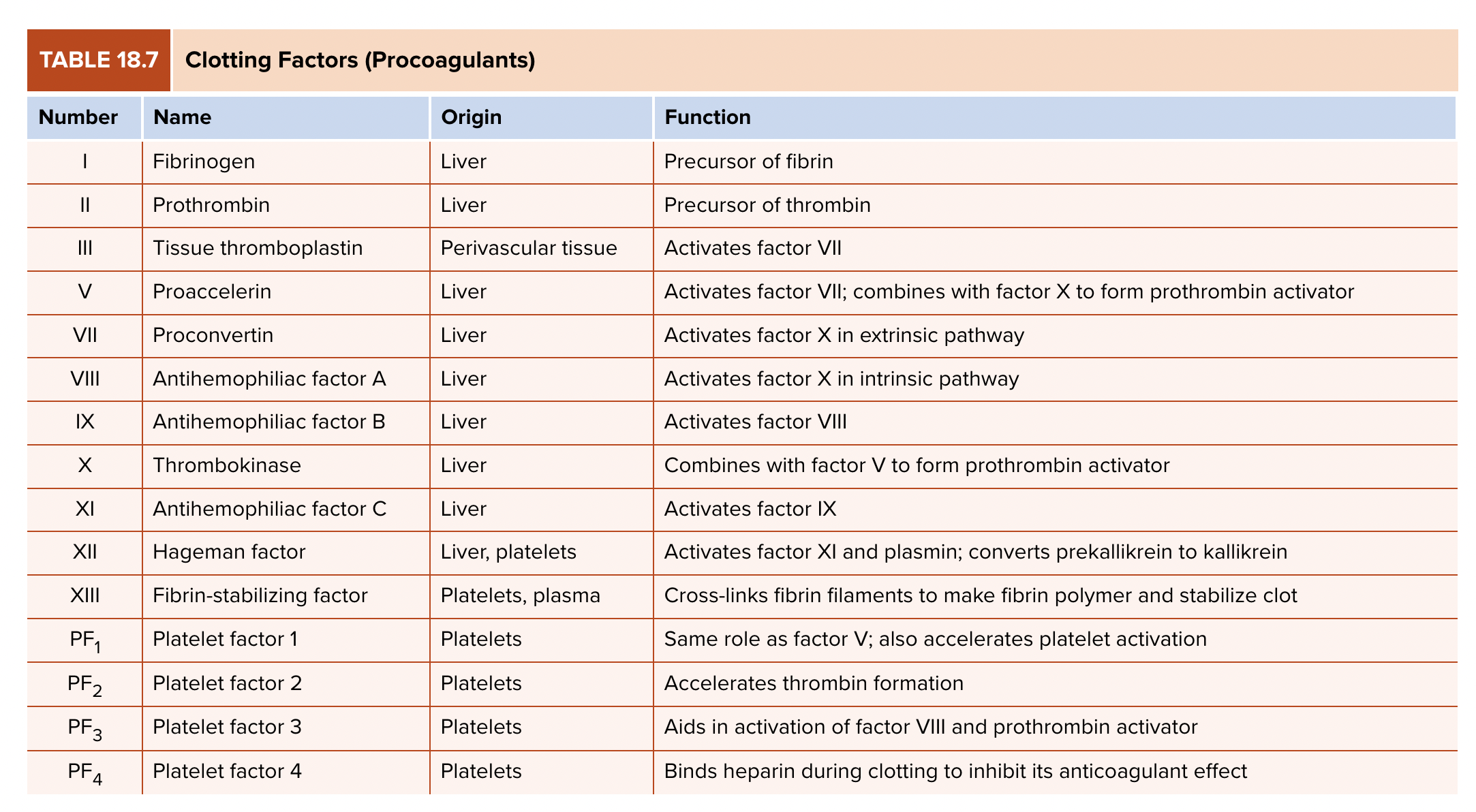
Factor VIII deficiency leads to hemophilia
Thrombosis - abnormal clotting of the blood in an unbroken vessel, slowest, do not move
Embolus - clot that travels through the bloodstream
DIC (Disseminated intravascular coagulation) - widespread clotting within broken vessels, limited to one organ or occurring throughout the body. Marked by widespread hemorrhaging, congestion of the vessel with clotted blood, and tissue necrosis in blood deprived organs