Lecture 12_Muscles-2
Events at the Neuromuscular Junction(NMJ) 9.1
Action potential arrives at axon terminal of motor neuron.
Voltage-gated Ca2+ channels ope. Ca2+ enters the axon terminal moving down its electrochemical gradient.
Ca2+ entry triggers ACH(neurotransmiter) to be released by exocytosis.
ACh diffuses across the synaptic cleft and binds to its receptors on the sarcolema.
ACh binding opens ions channels in the receptors that allow simultaneous passage of Na+ into the muscle fiber and K+ out of the muscle fiber. More Na+ ions enter the muscle fiber than K+ ions exit, which produces a local change in the membrane potential called the end plate potential.
ACh effects are terminated by its breakdown in the synaptic cleft by Acetylcholinesterase and diffusion away from the junction.
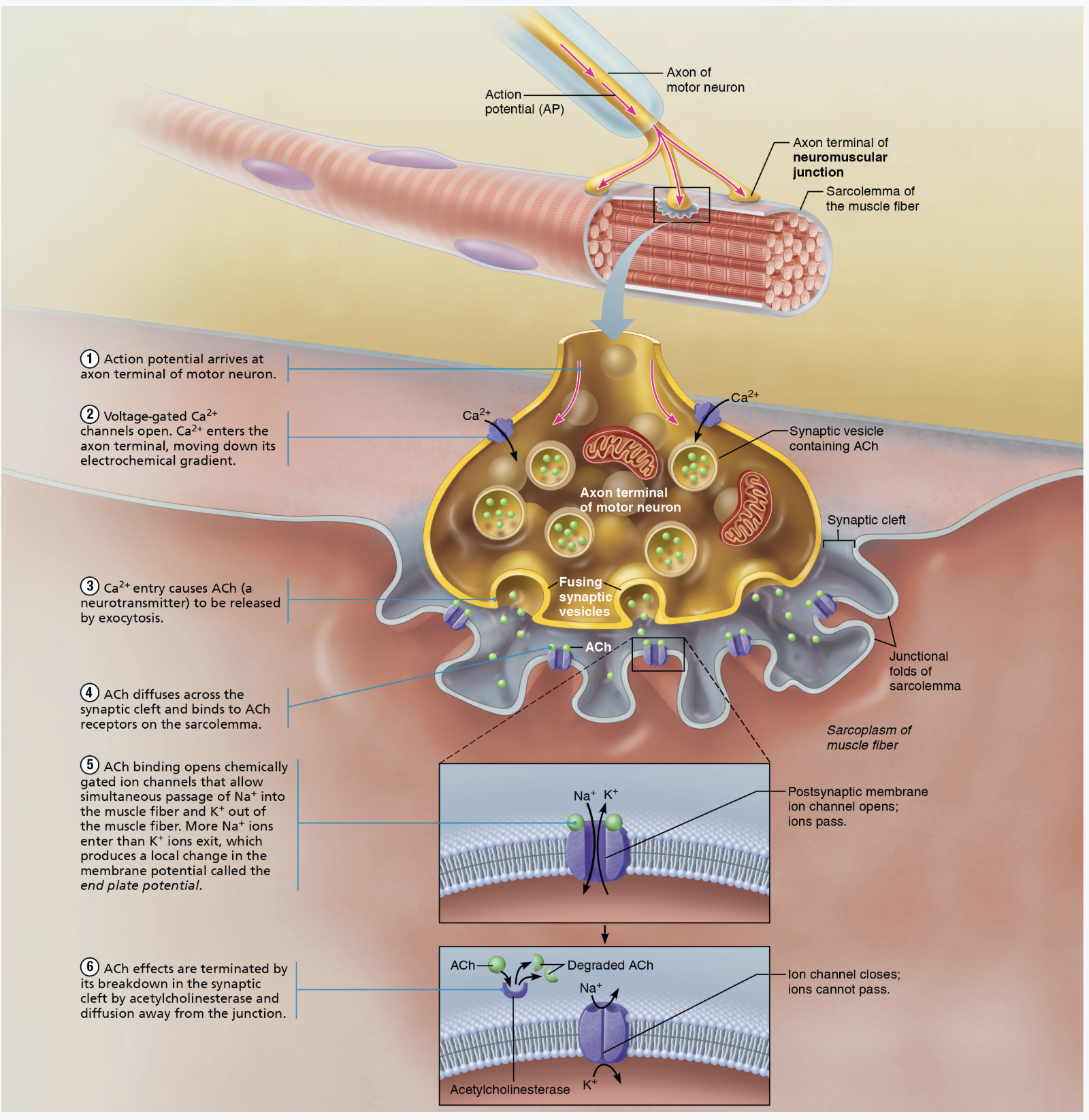
This process ensures that the muscle fiber is only stimulated when necessary, preventing continuous contraction and allowing for precise control of muscle movements.
Generation of an Action Potential
Resting Sarcolemma Polarized: At rest, the sarcolemma (muscle cell membrane) is polarized with a resting membrane potential.
Action Potential (AP): Changes in electrical charges across the membrane occur in three phases:
End Plate Potential (EPP)
Depolarization
Repolarization
Events in Generation of an Action Potential
End Plate Potential= Local depolarization: caused by ACh binding, opening chemically gated (ligand) ion channels:
Sodium (Na+) diffuses inward and Potassium (K+) diffuses outward.
More Na+ inwards so interior of sarcolema become less negative leads to local depolarization known as the End Plate Potential.
Depolarization= generation and propagation of an action potential:
This is characterized by:
Spread of local depolarization to adjacent areas of the sarcolemma.
Opening of voltage-gated Na+ channels results in Na+ influx, decreasing membrane voltage toward threshold potential.
If the threshold is reached, an Action Potential(AP) is initiated and spreads across the sarcolemma, leading to muscle fiber contraction.
Repolarization: Restoring electrical conditions of (RMP) resting membrane potential:
Na+ channels close and voltage-gated K+ channels open, leading to K+ efflux which restores polarity.
The muscle fiber enters a refractory period and cannot be stimulated until repolarization is complete.
Excitation-Contraction (E-C) Coupling
Purpose: Transmits the Action Potential along the sarcolemma, leading sliding of myofilaments.
Latent Period: Time between the initiation of the AP and the start of contraction.
AP propagates along the sarcolemma and down T-tubules; voltage-sensitive proteins stimulate Ca2+ release from the sarcoplasmic reticulum (SR).
Ca2+ ions are necessary for contraction.
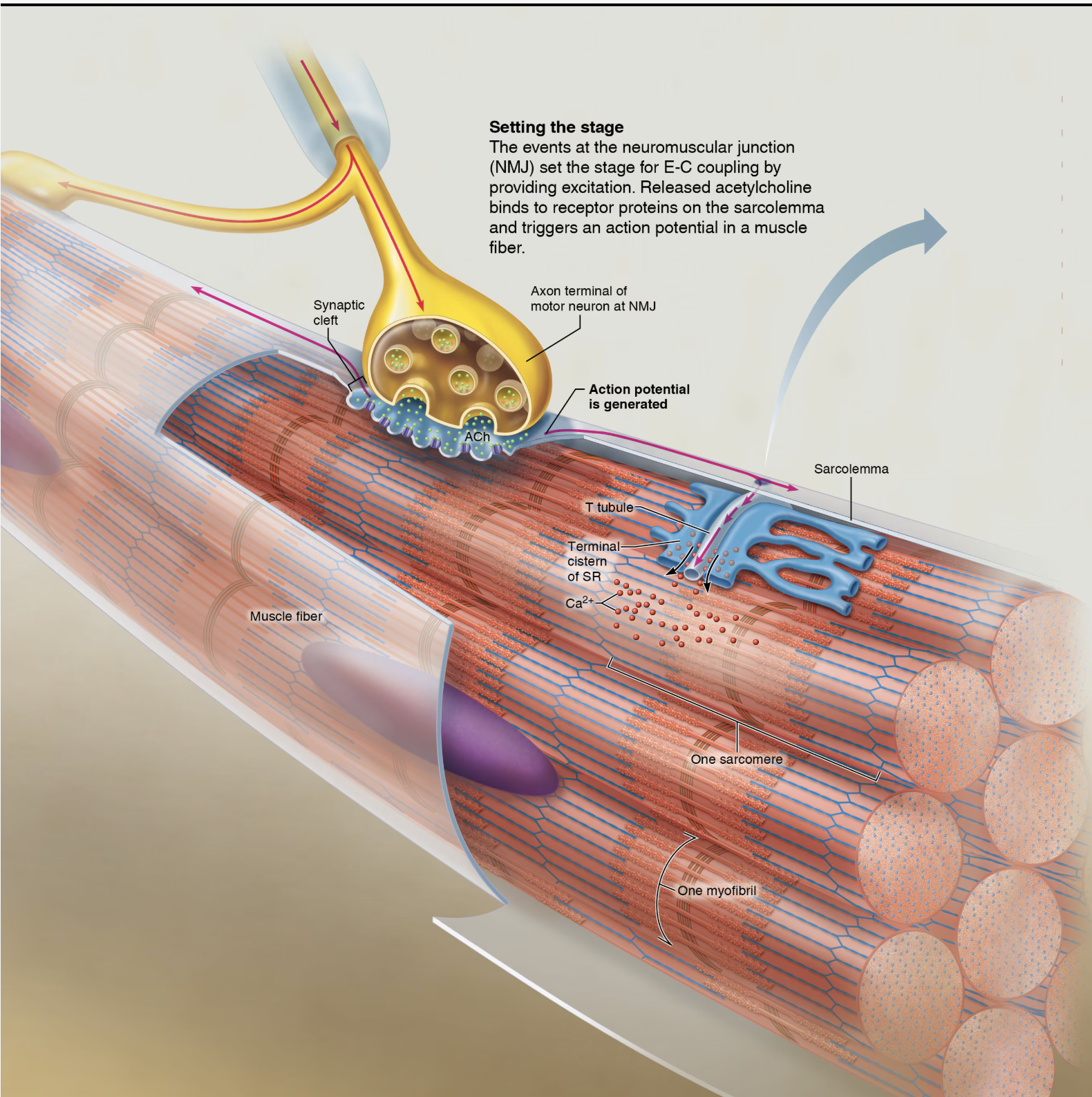
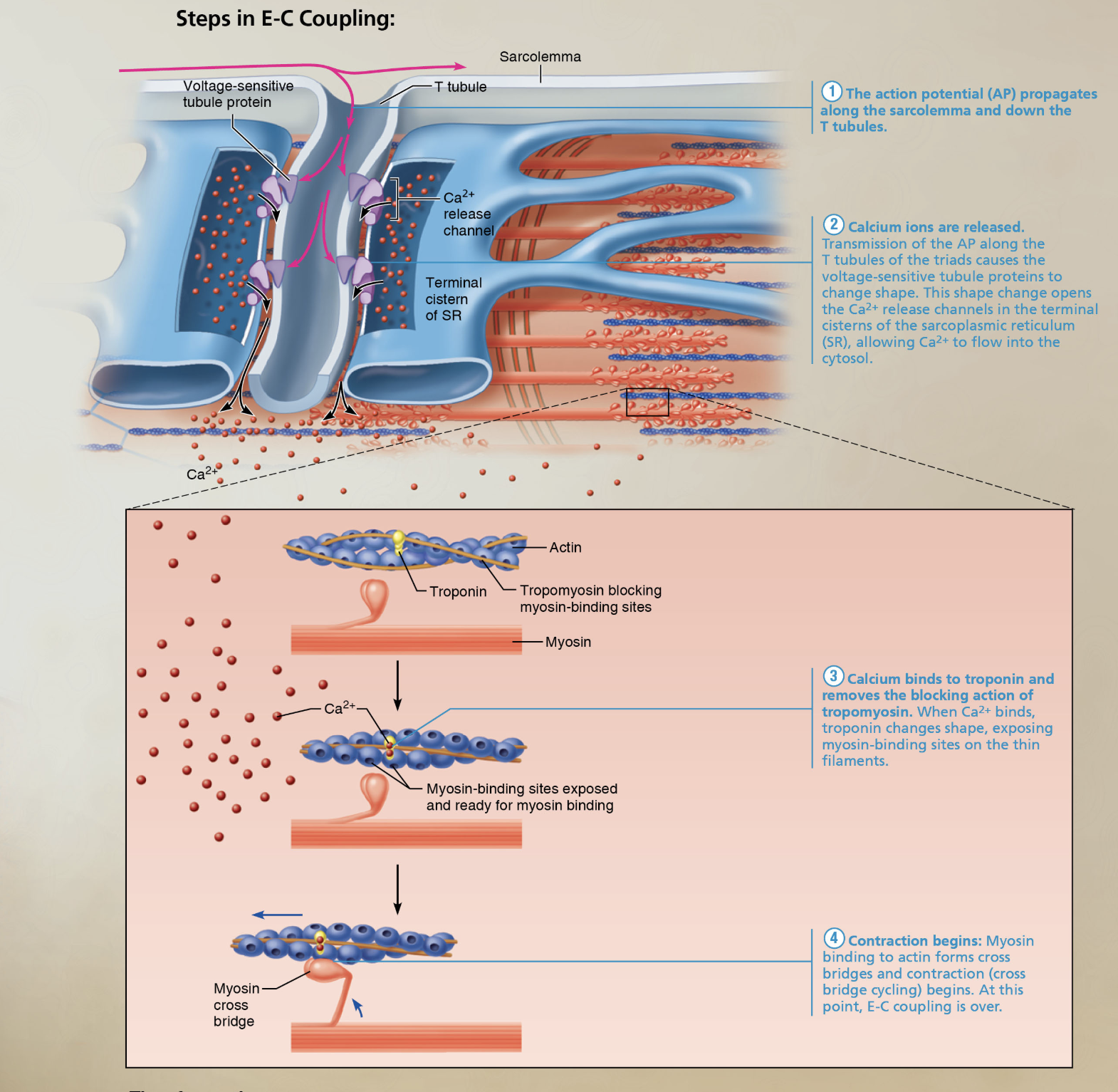
Steps in E-C Coupling:
The action potential(AP) propagates along the sarcolemma and down the T tubules.
Calcium ions are released: Transmission of the AP along T tubules of the triads causes the voltage-sensitive tubule proteins to change shape. this shape change opens the Ca2+ release channels in the terminal cisterns of the sarcoplasmic reticulum (SR), allowing Ca2+ to flow into the cytosol.
Ca2+ binds to troponin and removes the blocking action of Trompomyosin. When Ca2+ binds, troponin changes shape, exposing binding sites for Myosin(active sites)on the thin filaments.
Contraction begins: Myosin binding to Actin forms cross-bridges and contraction (cross bridge cycling) begins. At this point, E-C coupling is over.
Channels Involved in Initiating Muscle Contractions.
Nerve impulse reaches axon terminal = Voltage-gated calcium channels open = ACh released to synaptic cleft.
ACh binds to its receptors on sarcolemma = opens Ligand-gated Na+ and K+ channels = end plate potential.
Opens Voltage-gated Na+ channels = AP propagation.
Voltage-sensitive proteins in T tubules changes shape = SR releases Ca2+ to cytosol. The increase in cytosolic Ca2+ concentration initiates muscle contraction by binding to troponin, causing a conformational change that moves tropomyosin away from the myosin-binding sites on actin filaments.
Calcium Role in Contraction
At low intracellular Ca2+ concentration:
Tropomyosin blocks active sites on actin, preventing myosin attachment.
Muscle is relaxed.
At higher Ca2+ concentrations:
Ca2+ binds to troponin, moving tropomyosin away from myosin-binding sites.
Myosin heads attach to actin, causing sarcomere shortening and muscle contraction.
When stimulation ceases, Ca2+ is pumped back into SR and relaxation occurs.
Cross Bridge Cycle
Continues as long as Ca2+ signal and adequate ATP present.
Cross Bridge Formation: Energized myosin head attaches to actin thin filament.
Working (power) Stroke: Myosin head pivots, pulling the thin filament toward the M line.
Cross Bridge Detachment: ATP attaches to myosin, detaching it from actin.
Cocking of Myosin Head: energy from hydrolysis of ATP cocks myosin head into high-energy state.
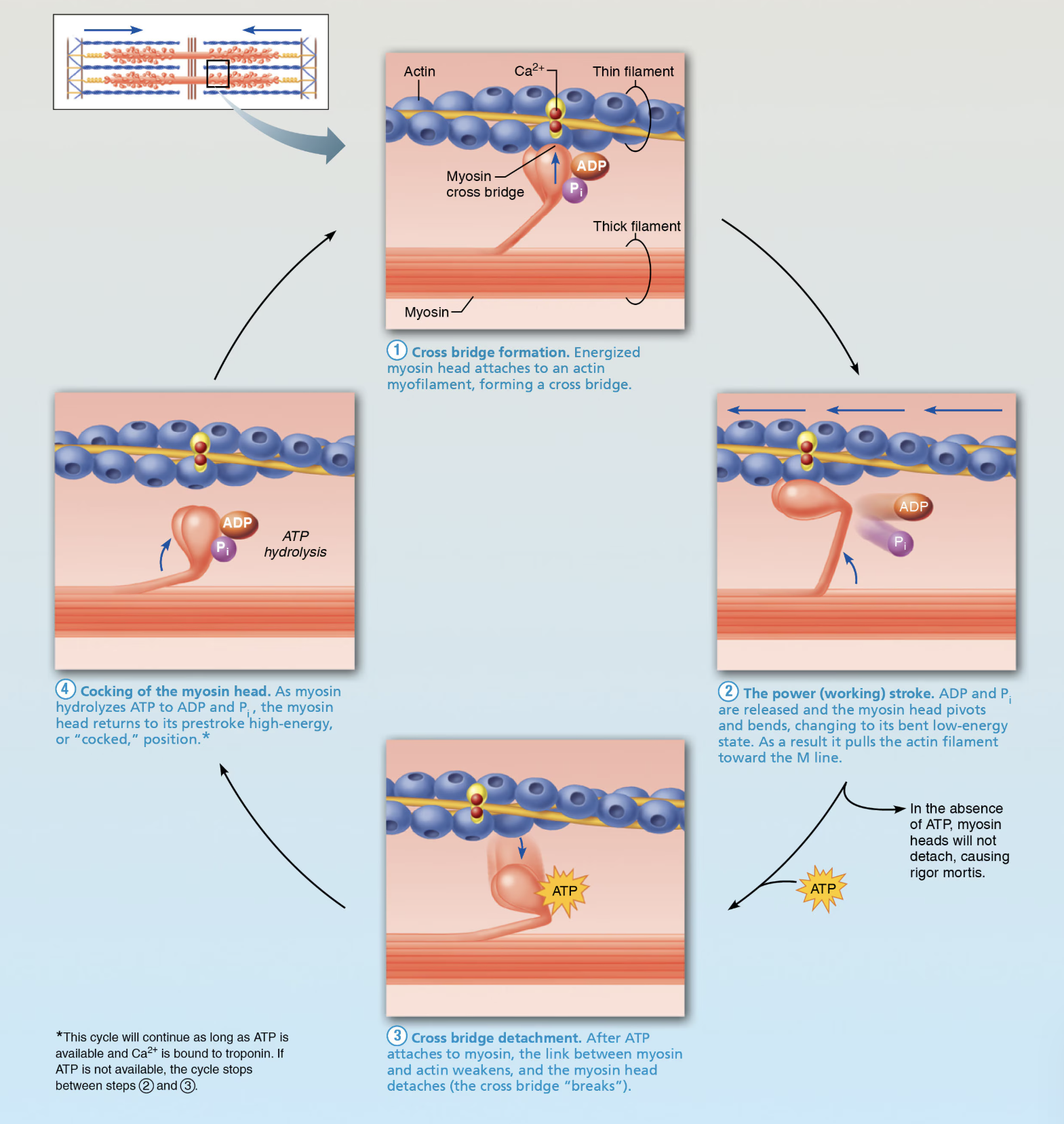
Homeostatic Imbalance
Rigor mortis
Cross bridge detachment requires ATP.
3-4 hours after death muscles begin to stiffeb with weak rigidity at 12 hours post mortem.
Dying cells take in Ca2+ = cross bridge formation.
No ATP generated to break cross bridges.
Muscle Mechanics and Types of Contractions
Same principles apply to contraction of single fiber and while muscle.
Muscle Tension: Force exerted by a contracting muscle on an object.
Load: The opposing force exerted on the muscle by the weight of the object to be moved.
Isotonic Contractions
Muscle changes in length while lifting load:
Concentric: Muscle shortens and does the work(e.g., lifting a book): muscles shortens because muscle tension exceeds load.
Eccentric: Muscle generates force as it lengthens (e.g., lowering a boo, calf muscle as you walk up a steep hill).
Isometric Contractions
Load greater than tension(contractile force)muscle can develop.
Tension increases to muscle’s capacity, allowing the muscle to maintain a stable position without changing its length (neither shortens nor lengthens).
Cross bridges form between actin and myosin filaments, enabling the muscle fibers to generate force while maintaining their length during isometric contractions. This type of contraction is crucial for activities such as holding weights in a fixed position or stabilizing joints during movement.
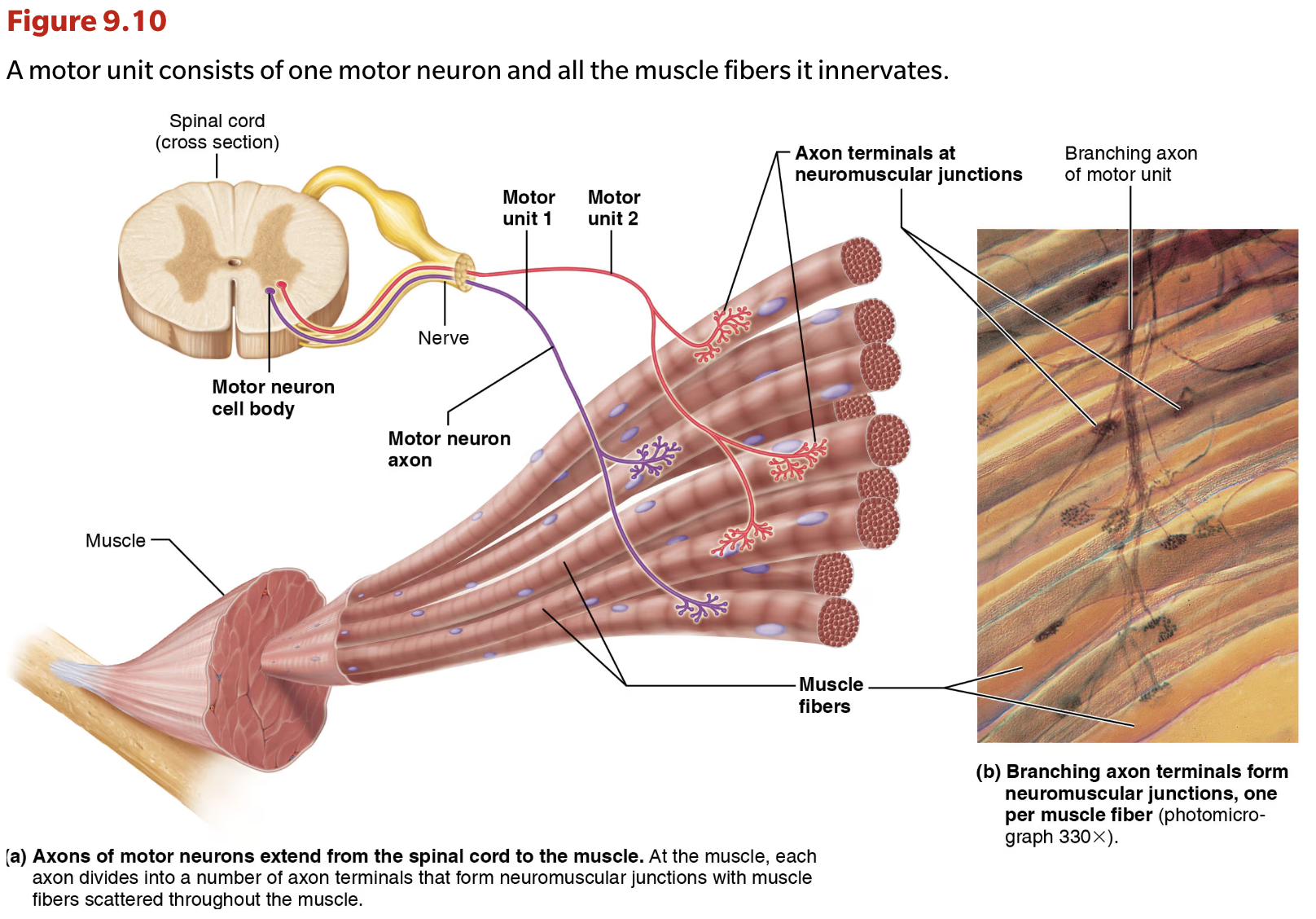
Motor Unit = motor neuron and all (four to several hundred) muscle fibers/cells it supplies.
Each muscle is served by at least one motor nerve:
Motor nerve contains axons of up to hundreds of motor neurons.
Axons branch into terminals, each of which results in a NMJ (neuromuscular junction) with a single muscle fiber.
Muscle fibers from one motor unit are spread throughout, causing a weak contraction of entire muscle.
Motor units contract asynchronously to help prevent fatigue.
Muscle Twitch
Response of a motor unit to a single action potential(stimulus) of it’s motor neuron-myogram.
Latent Period: No muscle tension; events of Excitation-contraction coupling: no muscle tension.
Period of Contraction: Cross-bridge formation; tension (contractile force) increases.
Period of Relaxation:Ca2+ reentry into SR(sarcoplasmic reticulum) leads to tension decline.
Muscle contracts faster than it relaxes.
Graded Muscle Responses
Varying strength of contraction for different demands.
Required for proper control of skeletal movement.
Responses graded by
Changing frequency of stimulation.
Changing strength of stimulation.
Muscle Metabolism
Energy Sources for Contraction:
ATP is the primary energy source for muscle contraction; only available for 4-6 seconds.
ATP is regenerated from:
Direct phosphorylation of ADP by creatine phosphate.
Anaerobic glycolysis generating lactic acid.
Aerobic respiration, yielding 32 ATP per glucose.
Muscle Fatigue
Physiological inability to contract despite stimulation caused by ionic imbalances, prolonged exercise, lactic acid accumulation, and total lack of ATP.
Factors Influencing Force of Contraction
Number of cross bridges attached is affected by:
Number of fibers stimulated.
Fiber size and hypertrophy.
Frequency of stimulation.
Muscle stretch.
Muscle Fiber Types
Classified by speed of contraction and metabolic pathways:
Slow oxidative fibers.
Fast oxidative fibers.
Fast glycolytic fibers.
Most muscles have a mixture of fiber types; genetic factors influence distribution.