Chapter 24
Coordinating Care for Patients With Infectious Respiratory Disorders
Respiratory tract is the common site of infection by pathogens due to direct exposure to microorganisms.
Upper respiratory tract
As environmental air is inhaled, the first line of defense lies within the upper respiratory tract
consists of the nasal cavities, the pharynx, and the larynx.
cilia hairlike projection transports any particles trapped by the mucous lining back into the nasopharynx and oropharynx. This mechanism is called the mucociliary escalator.
The tonsils and adenoids (lymphoid organs) play an integral role in the development of an immune response to pathogens remaining in contact with the mucoid surfaces of the throat through trapping and filtering
The larynx (voice box), which houses the epiglottis, provides mechanical protection of the airways.
During breathing, the epiglottis remains open to allow air to pass into the trachea. While food and fluids are swallowed, the epiglottis closes, directing solid material into the esophagus and preventing aspiration, or movement of gastric contents into the airways.
house small numbers of bacteria e.g. Staphylococcus, Streptococcus, spirochetes, mycobacteria, Pseudomonas, Proteus, and Enterococcus.
This “normal flora” functions to maintain a healthy respiratory status by competing with pathogens for attachment sites in the respiratory mucous lining and producing bactericidal substances that destroy harmful microorganisms.
Lower respiratory tract
The trachea marks the beginning of the lower respiratory tract, along with the bronchi, bronchioles, and alveoli.
A layer of ciliated cells and the mucous-secreting cells within the trachea, bronchi, and bronchioles protect the lower respiratory tract via the mucociliary escalator from smaller-size particles that have avoided the upper airway defenses
The lower respiratory tract houses no resident flora and is considered a “sterile site
if pathogens enter the lowest portion of the respiratory tract, alveolar macrophages are the most important means of eliminating microorganisms from this area by phagocytosis.
Establishment of respiratory tract infection: for respiratory infection to be established in the lower respiratory tract
Avoidance of trapping in the mucociliary layer of the upper respiratory tract.
Avoidance of the phagocytic action of the alveolar macrophages in the lower respiratory tract
Infectious organisms must be airborne (particles less than 5 µm that remain suspended in the air for a prolonged time) and have the ability to remain virulent (toxic) while in the air.
There must be sufficient numbers of infectious organisms inhaled and deposited on susceptible tissues within both the upper and lower respiratory tracts, preventing innate protective mechanisms from functioning effective.
The inflammatory response of the respiratory tract
once pathogens are established in the respiratory tract, an inflammatory response is initiated.
Direct stimulation by infecting organisms leads to the secretion of pro-inflammatory cytokines (interleukin [IL] and tumor necrosis factor [TNF]) by airway epithelial cells.
Neutrophils (a type of white blood cell [WBC]) are recruited to the infected alveoli along with other immune cells and serum components
Capillary permeability increases, and the alveoli fill with fluid and plasma proteins.
This accumulation of exudate (a mass of cells and fluid) provides the perfect medium for the proliferation of the infecting organism(s) and assists with movement to other nearby alveoli
this causes hypoxia depending on its severity.
Influenza
Human influenza viruses are divided into three types, designated as A, B, and C.
Influenza A viruses are made up of two viral proteins
hemagglutinin (H) and neuraminidase (N).
Influenza B is not broken down into subtypes but can be categorized by different strains.
Influenza types A and B are responsible for epidemics of respiratory illness that occur mostly during the winter months.
The most extensive and severe outbreaks are from influenza A because of the tendency of the H and N antigens to mutate.
Influenza C has no symptoms at all or a very mild respiratory illness.
does not have serious public health concerns.
Risk factor for influenza infection
age: young children -2 year
older adult of 65 yr
due to an immature or less active immune system
Occupation: healthcare worker, family career, daycare provider, and early childhood educator
Environment: affects people who live in dormitories, military quarters, and long-term care facilities
Immune system compromise: cancer pt on chemo, transplant pt receiving antirejection medications, HIV/AIDs with CD4+ count of less than 200cells
Chronic illness: pt with DM, renal failure, asthma, cardiac and respiratory disease have higher risk of developong serious complications
Pregnancy: pregnant women, those planning on and those who have given birth are greater risk of developing pneumonia
Influenza is transported through aerosolization of small droplets (particles less than 5 µm that settle within 3–6 feet from point of release) from an infected individual’s sneezing or coughing or by direct contact with fomites.
Fomite carry organisms and facilitate transfer from one person to another using objects like stethoscope, scissor and pen.
Over a period of approximately 4 to 6 hours, these infected cells reproduce and spread the virus to other respiratory cells, extending the infection throughout the respiratory tract.
The incubation period (from the time of initial droplet inhalation to symptom development) lasts approximately 18 to 72 hours.
The severity of the symptoms and subsequent illness are dependent on the amount of viruses shed during the replication phase and the number of respiratory cells affected.
Virus shedding usually ends 2 to 5 days after symptoms first appear; therefore, it is important to remember that individuals are infectious for up to 7 to 10 days.
Clinical manisfestation
rapid onset
fever, headache, sore throat, severe nasal congestion, cough, myalgia or muscle aches and pains, malaise (the general feeling of being unwell), and fatigue.
Management
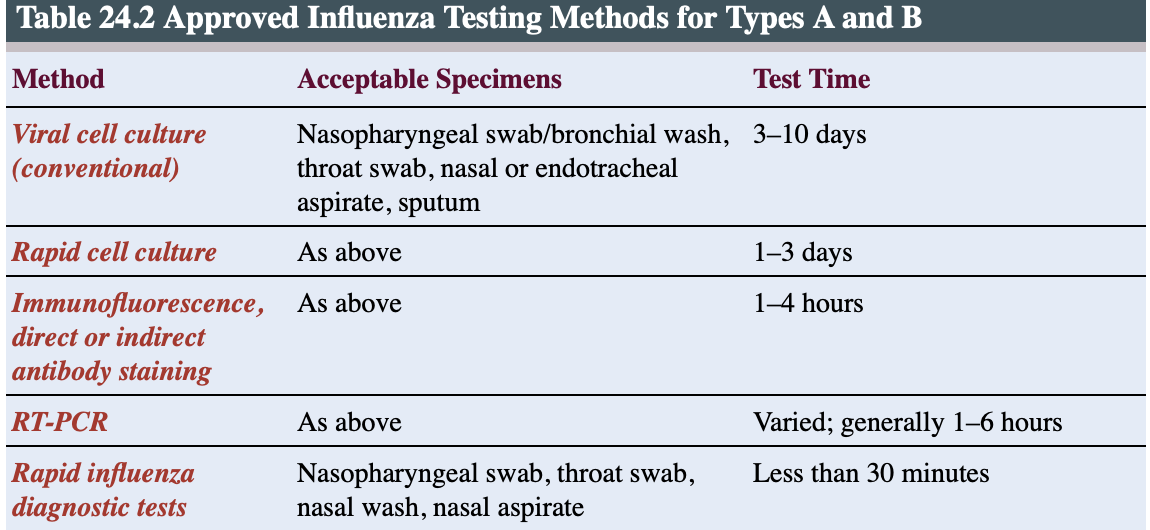
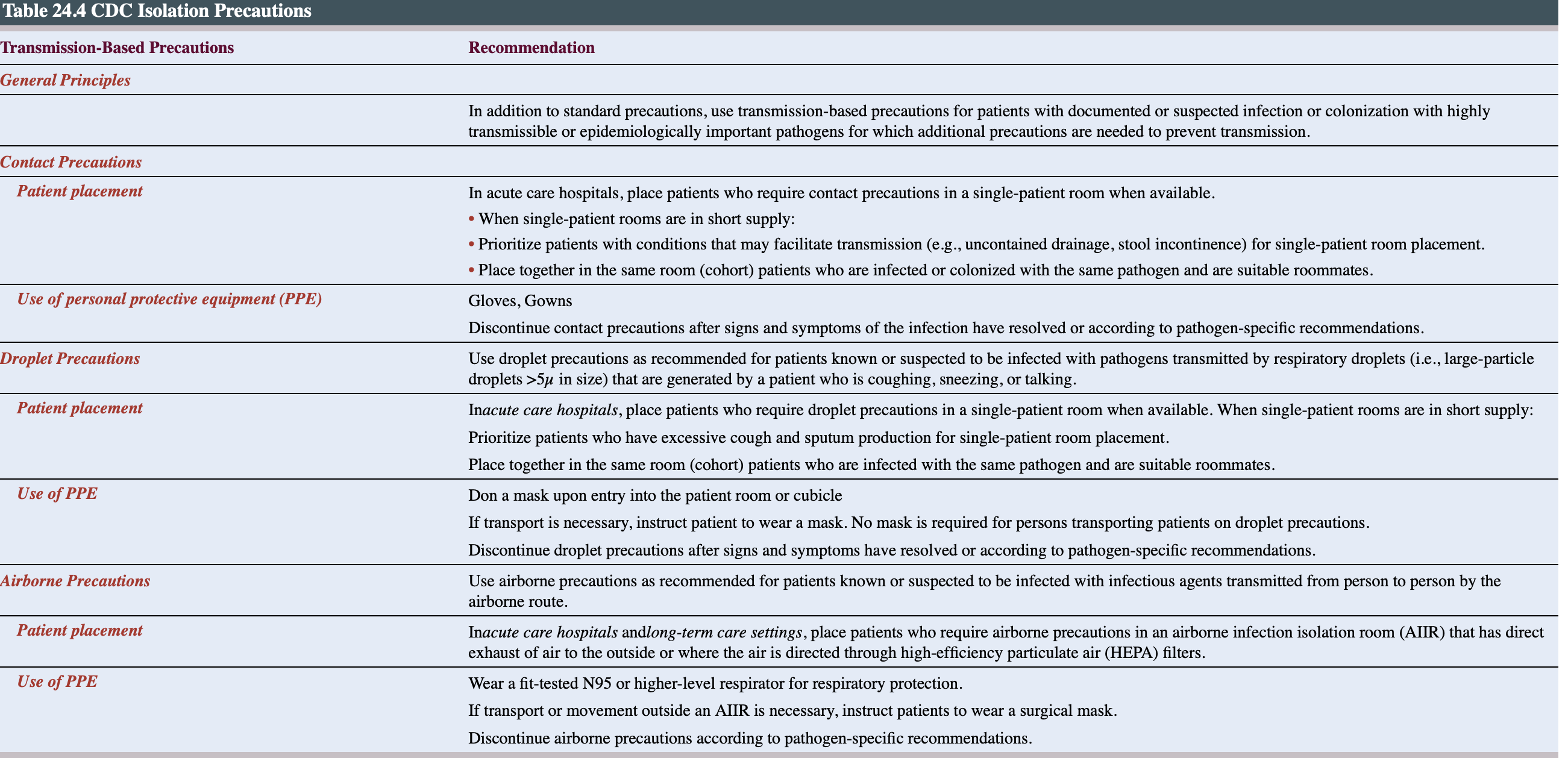
gold standard: sampling the respiratory secretion for viral culture
takes up to 10 days to get confirmation
The most commonly utilized tests for influenza are called rapid influenza diagnostic tests (RIDTs).
The identification of an influenza virus infection can be made in less than 30 minutes via nasopharyngeal/throat swab or nasal washings/aspirate.
Circulating antibodies can be detected in the blood of individuals with an influenza infection within 2 weeks after initial infection.
Specific laboratory tests conducted are hemagglutination inhibition, complement-fixation, and enzyme-linked immunosorbent assay.
Treatment
annual vaccination
side effect low grade fever and soreness
Do not give it to pt with egg allergies since it contains inactive egg protein
Appropriate time for vaccination is is in the early fall before the “flu season” begins.
Medication
mild influenza- relief symptoms
Antipyretics/analgesics for fever and aches, adequate fluid intake to avoid dehydration, and rest are typically prescribed.
For more serious forms of influenza or widespread local outbreaks, several antiviral medications are available for prophylaxis or treatment.
Antiviral medications does not “cure” the flu; however, further viral replication within the respiratory tract is impaired.
The best results are achieved when antiviral medications are initiated within 24 to 48 hours of symptom onset
Complication
Primary influenza viral pneumonia is the least common but severe complication of influenza infection and occurs more frequently in individuals over the age of 65 years with or without chronic underlying illness.
marked by progressive shortness of breath, persistent fever, and cardiovascular compromise.
Nursing interventions
Tachypnea: 1st compensatory mechanism to decrease oxygen delivery.
(Tachypnea and tachycardia decrease cardiac output, reducing perfusion and peripheral oxygen saturation)
Tachycardia: second compensatory mechanism
Decreased oxygen saturation: Impaired gas exchange at the alveolar level results in hypoxia.
Fever occurs as a part of the inflammatory response
Neurological function: Agitation, restlessness, anxiety, lethargy, and fatigue results due to decreased tissue perfusion from altered alveolar gas exchange.
Breath sounds: Adventitious breath sounds such as rhonchi, crackles, and rales may be audible on lung assessment from fluid and exudates filling the alveoli.
Audible wheezing is a result of airway reactivity due to inflammation and/or bronchospasm.
General appearance: sudden onset of fever, chills, muscle aches, and fatigue in a generally ill-appearing patient
Peripheral pulse: Diminished tissue perfusion causes blood to be shunted away from peripheral areas to the main core body organs.
Peripheral pulses diminish, and skin becomes moist and pale.
Peripheral cyanosis (bluish color to the nailbeds) is a late sign of tissue hypoxia.
Lab values: Arterial blood gases (ABGs): Primary respiratory infections may initially cause a respiratory alkalosis (increased pH, decreased carbon dioxide [CO2]) in response to tachypnea.
As the condition progresses, a respiratory acidosis (decreased pH, increased carbon dioxide [CO2]) will develop.
Positive RIDTs: These tests are sensitive, so a positive test is indicative of the presence of flu.
Actions
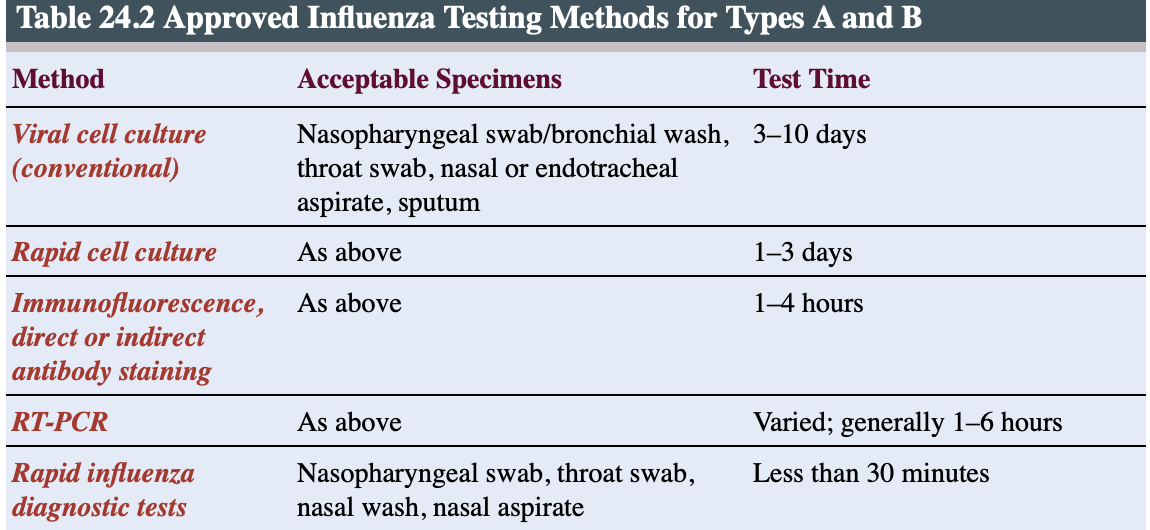
Place patient on droplet precautions to avoid viral transmission.
PPE: mask, gown, gloves, and eye protectant.
administer humidified supplemental oxygen.
HOB- semi fowler 30””
Medication administration
administer antipyrectic as needed
antiviral:Early administration of antiviral medications (within 24–48 hours of symptom onset)
analgesic:Pain relief can increase comfort and allow for mobilization and effective coughing/expectoration of respiratory secretions.
fluid intake: Replacing insensible losses from fever and tachypnea allows for optimal cardiovascular performance and liquefaction of respiratory secretions.
Nutritional intake: frequent small meal high in protein
Obtain cultures: before the administration of antiviral medications.
need to assess for the presence of bacterial infection before presence is masked by medication administration
Teaching
Hand washing is essential to prevent the spread of the virus to others.
Disinfect frequently used objects and surfaces.
Limit contact with others for up to 10 days after the first symptoms appear or for at least 24 hours after fever has gone.
(viral shedding last 10 days and up to several weeks.
Report worsening shortness of breath; change in amount, color, and viscosity of pulmonary secretions; and recurrent fever. viral infections can be mild at first, rapidly progressing to primary viral pneumonia or secondary bacterial pneumonia.
increase fluid intake
Antiviral medications do not “cure” the flu; they just shorten the duration and severity of symptoms and may prevent serious complications.
flu vaccination every year.
Puemonia
One-third of these cases occur in persons over 65 years of age.
Risk factors for the development of pneumonia among the adult population include
Advanced age
long-term care residence
smoking
chronic respiratory disease (asthma, emphysema)
immune system dysfunction (malignancy, transplantation, HIV/AIDS)
altered mental status; prolonged immobility
aspiration of stomach contents or foreign material
prolonged nothing-by-mouth (NPO) status
diminished cough, gag, and/or swallow reflexes
exposure to air pollutants, gases, or noxious inhalants
hospitalization for longer than 48 hours.
Types of pneumonia
community-acquired pneumonia (CAP)
methicillin-resistant Staphylococcus aureus (MRSA)
community-acquired pneumonia (MRSA CAP)
hospital-acquired pneumonia (HAP)
healthcare-associated pneumonia (HCAP).
Community-acquired pneumonia occurs in individuals who have not been recently hospitalized or are living outside of a healthcare/long-term care facility e.g streptococcus pneumoniae most causative organism
Methicillin-resistant CAP results from colonization of MRSA within the upper respiratory tract. This can produce mild, virtually asymptomatic illness that is customarily treated on an outpatient basis with oral antibiotics.
Hospital-acquired pneumonia develops in patients after 48 hours of hospital admission. The diagnosis of healthcare-associated pneumonia is made 48 to 72 hours after admission and is accompanied by the following risk factors:
• Recent antibiotic therapy
• Receiving immunosuppressive therapy
• Diagnosed with a chronic disease
• Treated within healthcare facilities, such as dialysis clinics, adult daycare centers, and rehabilitation facilities, where they are in frequent, close contact with healthcare personnel and other patients who may be colonized with various infection-causing organisms
Pneumonia caused by atypical organisms is often associated with mild respiratory illness. Examples of atypical organisms are Mycoplasma, Chlamydophila (from handling birds), Legionella (present in intricate water delivery systems), and Bordetella pertussis (responsible for whooping cough).
Pathophysiology of pneumonia
Pneumonia is an inflammation of the lung parenchyma (functional lung tissue) resulting from a bacterial, viral, or fungal infection.
Organisms continue to proliferate at the alveolar level. As the inflammatory response unfolds, protein-rich fluid and exudates fill the alveoli, impairing the exchange of oxygen and CO2.
A ventilation–perfusion mismatch results from adequate blood flow to a nonfunctioning(dead space), fluid-filled alveolar unit.
Organism can be can localize to one or more lobes (lobar or multilobar pneumonia) or spread throughout the lung parenchyma
Bacteria causing pneumococcal pneumonia (S. pneumoniae) can gain access to the bloodstream, leading to septicemia and septic shock.
Clinical manisfestation
Fever
Tachypnea/dyspnea
Tachycardia
Chills
Cough, productive or nonproductive- thick sputum
Pleuritic chest pain- rubbing, stabbing and sharp pain
Fatigue
Myalgia/arthralgia
in severe form
purulent or blood streaked sputum
hypotension
dysrhythmia
morbidity from severe infectious pneumonia include:
1. Altered mental status
2. Respiratory rate greater than 30 breaths per minute
3. Hypotension (systolic blood pressure less than 90 mm Hg)
4. Heart rate greater than 125 beats per minute
5. Body temperature less than 95°F (35°C) or greater than 104°F (40°C)
6. Arterial blood pH less than 7.35
7. Serum sodium level less than 130 mg/dL
8. Hematocrit less than 30%
9. PaO2 less than 60 mm Hg on supplemental oxygen greater than or equal to 40%
10. Presence of pleural effusion on chest x-ray or computed tomography (CT) scan
Medical management
increase WBC and elevated band neutrophils indicate acute inflammation
increase C-reactive protein test and detect presence ofm inflammation and infection. value 30-300mg/dL in viral and bacterial pneumonia.
ABGs: respiratory alkalosis; decrease CO2, increased pH due to tachypnea then progress to respiratory acidosis with elevated CO2, decreased paO2 and decreased pH occurs.
Sputum cultures will reveal a preliminary category of the offending organism by Gram stain and confirm the specific organism after 24 to 48 hours of incubation in the laboratory.
Chest x-rays may or may not show infiltrates and can be up to 72 hours behind in their ability to reveal an infectious process.
CT scans may demonstrate consolidation and presence of pleural effusion.
Treatment
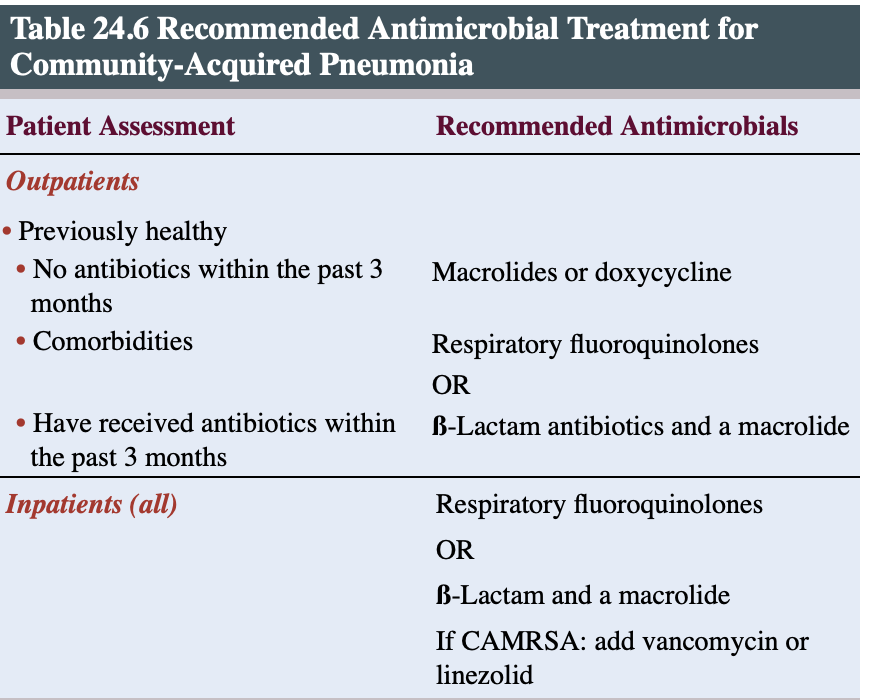
Uncomplicated pneumonias can be effectively treated in the outpatient setting.
More severe cases require hospitalization and supportive care. Because pneumonia may result in hypoxia, the administration of oxygen to reverse or prevent hypoxia is an essential first step.
patient work chronic lung pathology such as COPD require careful monitoring due to high concentration of oxygen can depress their drivve to breathe.
adequate hydration is also an important intervention to support the patient’s cardiovascular status and assist in thinning respiratory secretions for easy expect.
Medication
Bronchodilator therapy with albuterol (short-acting selective beta-2 adrenoceptor agonist) or Combivent (slow-onset anticholinergic agent) delivered either by aerosol nebulization or by metered-dose inhaler will open swollen and narrowed airways and promote ease of breathing.
Antibiotic therapy broad spectrum is initiated
for hospital-associated pneumonia (HAP), antibiotic are emphiric- treatment based on clinical experience before organism is identified- Pseudomonas aeruginosa is the major pathogen associated with HAP.
Complication
Severe MRSA CAP can lead to a necrotizing bacterial pneumonia requiring hospitalization.
In aspiration pneumonia, the acidity of stomach contents is caustic to the delicate lung tissue.
A necrotizing pneumonia may develop, resulting in fibrosis and scarring of the lung tissue.
Pulmonary fibrosis and pulmonary hypertension from severe pulmonary infections can impair lung function after the respiratory infection resolves.
Most antibiotics do not cross the blood–brain barrier, making the central nervous system a potential site of bacterial spread via the bloodstream.
Acute meningitis can occur as a complication of pneumococcal pneumonia.
empyema, a collection of purulent material in the pleural space, another possible complication, should be drained by the insertion of a chest tube.
Pleurodesis, the injection of a sclerosing or scarring agent into the pleural space, causing the visceral and parietal pleura to “stick together,” may be performed after the empyema has been resolved to prevent recurrence.
bacteremia
atelectasis- complete or partial collapse of the lungs seen in post op or immobile pt.
septic shock and acute respiratory failure with organ damage
Evidence of organ impairment/failure due to decreased tissue perfusion includes:
• Agitation/confusion: It is important to stress that this may be the only presenting sign/symptom in those over 65 years of age.
• Peripheral cyanosis
• Central cyanosis
• Decreased urinary output/elevated creatinine level
• Hypoactive bowel sounds
• Increased liver function laboratory values (aspartate aminotransferase/alanine aminotransferase)
Nursing interventions
Tachypnea: 1st compensatory mechanism to decrease oxygen delivery.
(Tachypnea and tachycardia decrease cardiac output, reducing perfusion and peripheral oxygen saturation)
Tachycardia: second compensatory mechanism
Decreased oxygen saturation: Impaired gas exchange at the alveolar level results in hypoxia.
Fever occurs as a part of the inflammatory response
Neurological function: Agitation, restlessness, anxiety, lethargy, and fatigue results due to decreased tissue perfusion from altered alveolar gas exchange.
Diminished cough, gag, and swallow reflexes resulting from altered levels of consciousness can contribute to aspiration risk.
Breath sounds: Adventitious breath sounds such as rhonchi, crackles, and rales may be audible on lung assessment from fluid and exudates filling the alveoli.
Respiratory secretions: Purulent and/or bloody secretions may result from a buildup of exudate in the alveoli.
Peripheral pulses diminish, and skin becomes moist and pale. Peripheral cyanosis (bluish color to the nailbeds) is a late sign of tissue hypoxia.
Labs
Sputum microbiology: report organism and antibiotics organism is sensitive to
ABGs: Bacterial respiratory infections may initially cause primary respiratory alkalosis (increased pH, decreased CO2) due to increased respiratory rate. As the condition progresses, a primary respiratory acidosis will occur (decreased pH, increased CO2).
Insensible losses from fever and tachypnea along with decreased intake from malaise and increased work of breathing can lead to more serious tachycardia and dehydration.
Actions
Administer humidified oxygen as ordered.
Administer antibiotics as ordered
Pulmonary hygience such as
Incentive spirometry
Coughing and deep breathing
Postural drainage
Vibration/percussion
Early mobility
this done in an effort to mobilize respiratory secretion and allow expectoration- reduces the incidence of atelectasis and worsening pneumonia in hospital patients.
Position: HOB 30” semi fowler- prevent aspiration and facilitate lung expansion
side to side turning assist with alveolar recruitment
For infiltrates of only one lung, when turning, preferentially position the patient with the good lung down to maximize perfusion to the functional alveolar units.
Monitor I&O: Optimal fluid balance assists with thinning respiratory secretions for ease of expectoration and maintains adequate tissue perfusion/oxygenation.
Small, frequent meals that are high in protein and vitamins are recommended.
Assess cough, gag, and swallow reflexes before offering food and drink. If reflexes are impaired, maintaining NPO status or initiating enteral feedings via a feeding tube may be required until a formal swallow evaluation can be
obtained.
Approach activities of care with intervals of rest. Fatigue and decreased tissue oxygen delivery limit activity tolerance.
Teaching
Hand hygiene and respiratory etiquette
Introduce strategies to combat fatigue and conserve energy; adequate rest
stress the importance of finishing all medication even if patients begin to feel better. Antibiotics offer a “cure” for bacterial infections. Incomplete treatment can lead to a recurrence of symptoms and the emergence of drug-resistant organisms.
Adequate nutrition is essential for healing and recovery from respiratory infections.
Understanding of signs and symptoms indicating worsening respiratory status
Encourage “at-risk” patients to get a pneumonia vaccine annually.
Tuberculosis
significant and potentially life-threatening respiratory infection caused by the organism Mycobacterium tuberculosis, an aerobic acid-fast bacillus (AFB).
majority of these new cases occurring in the United States were caused by reactivated latent tuberculosis infection (LTBI).
Populations living outside of the United States,
low socioeconomic groups that have obstacles in accessing healthcare
racial and ethnic minorities have the highest incidence
TB affects blacks, Hispanics, and Asians.
Tuberculosis is also a persistent problem in the homeless and incarcerated populations.
Persons infected with HIV or who have AIDS are at exceptional risk of contracting TB or reactivating latent TB- immunosuppression and the risk of contracting and spreading new strains of drug-resistant TB (MDR TB).
Tuberculosis is the leading killer of people with HIV infection.
Pathophysiology and clinical manifestations
transmitted by aerosolized droplets inhaled from the coughing or sneezing of an infected individual.
Droplets of M. tuberculosis are tiny and can remain suspended in the air for several hours.
transmission of active tubercule bacilli have shown that in close-contact situations, those whose sputum is infected with AFB are most likely to transmit the infection.
estimated that up to 3,000 infectious nucleated droplets can be released in one cough
most of the bacilli remain within the upper airway and rarely cause active disease.
Bacilli that manage to evade the mucociliary escalator defense are deposited within the alveoli and are quickly engulfed by phagocytic pulmonary macrophages.
Once they are ingested by the macrophages, there is a slow but continued multiplication of the Mycobacterium.
Tuberculosis is classified as follows:
• Latent tuberculosis infection (LTBI)
• Primary tuberculosis infection (PTBI)
• Primary progressive TB infection (PPTBI)
• Drug-resistant M. tuberculosis (MDR TB)