Lecture 9: Alteration in cardiovascular function
diseases of the arteries and veins:
arteriosclerosis
chronic disease of the arterial system characterized by:
abnormal thickening and hardening of the vessel walls
smooth muscle cells and collagen fibers migrate to the tunica intima (causing thickness and stiffness of tunica intima)
this leads to narrowing of the artery lumen
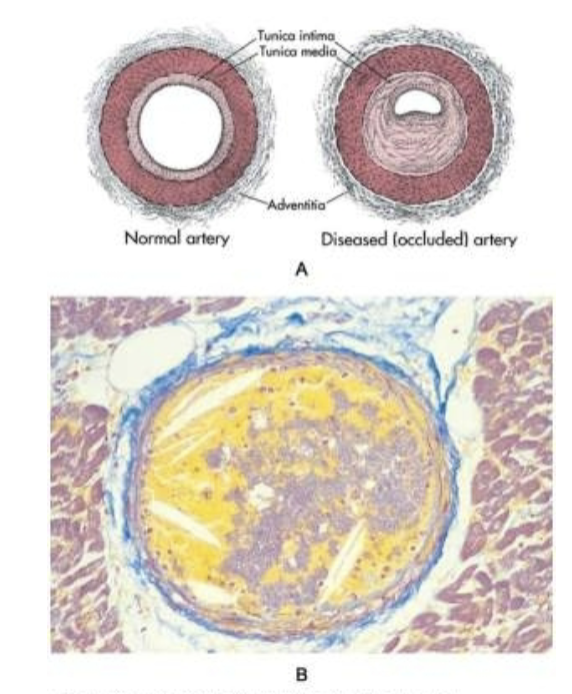
atherosclerosis
atherosclerosis is a form of arteriosclerosis
thickening and hardening is caused by accumulation of lipid-laden macrophages in the arterial wall
this leads to formation of lesion called plaque
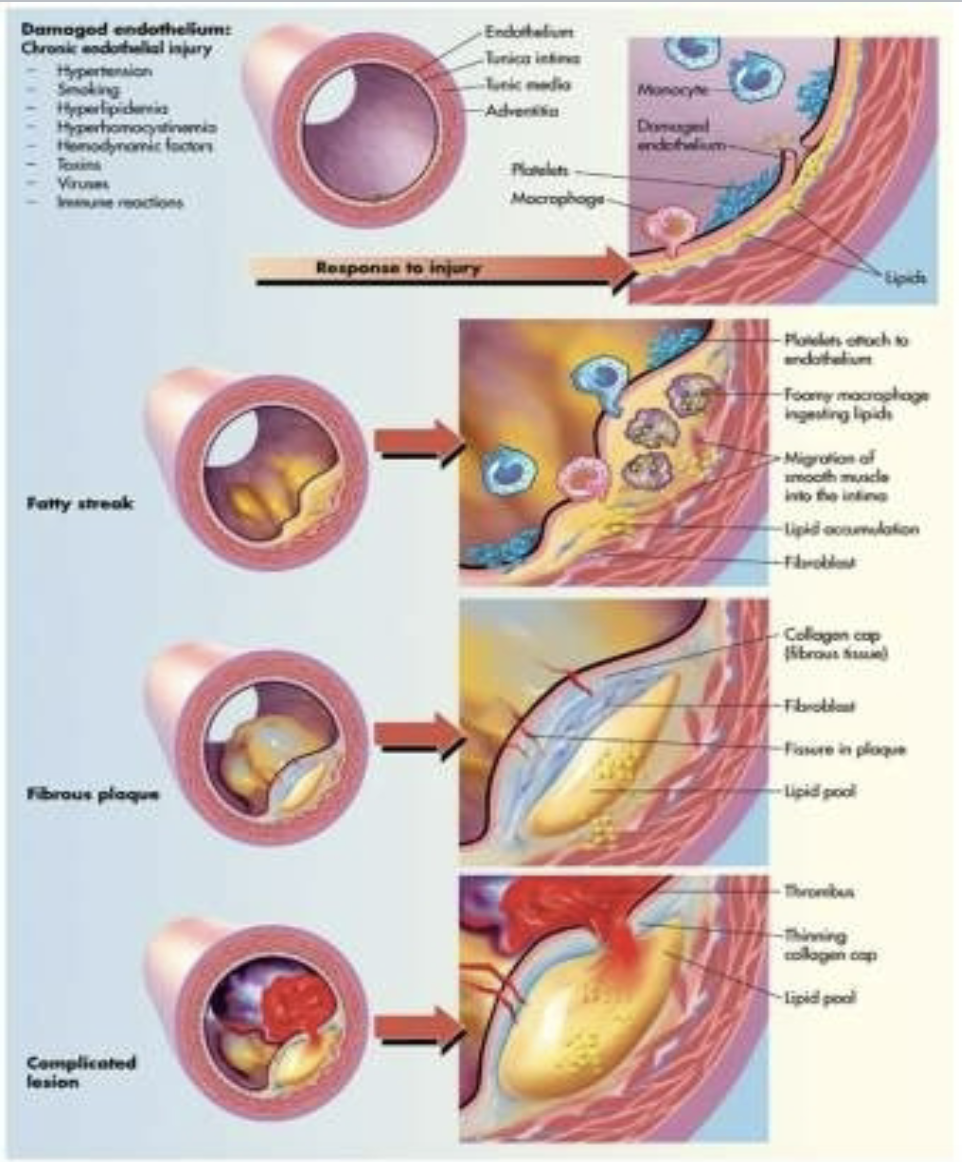
atherosclerosis is an inflammatory disease, that progresses from endothelial injury to formation of the plaque
the possible cause of injury could be smoking, diet, hypertension, diabetes, high levels of ldl… (… == etc.?)
erythrocyte sedimentation rate is an indirect measure of atherosclerotic plaque
progression
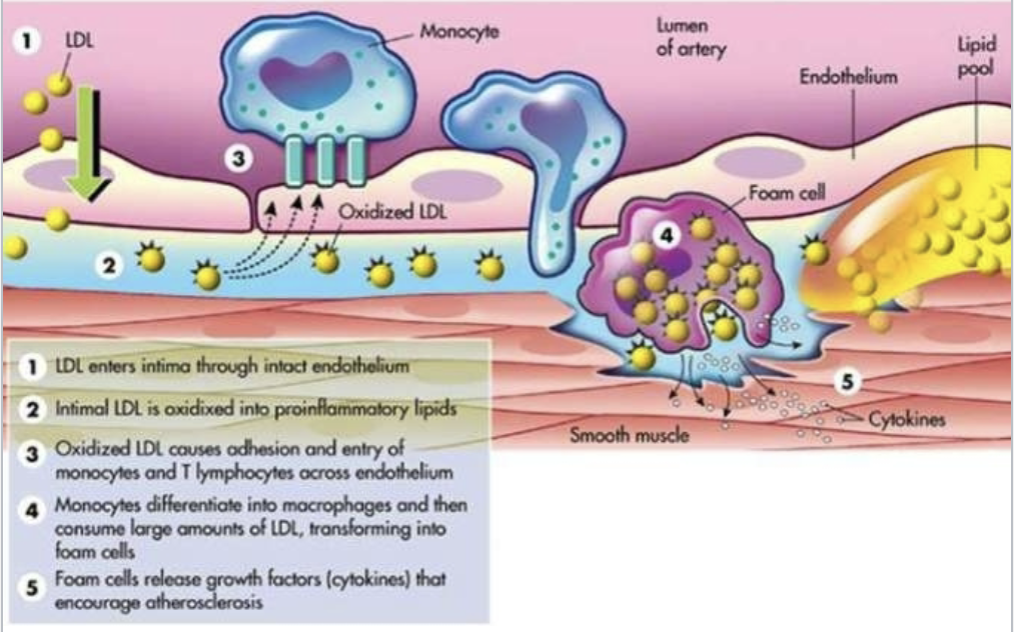
once endothelial cells are injured they become inflamed and cannot make normal amount of antithrombotic and vasodilating cytokines and leads to formation of atherosclerosis
macrophages adhere to injured endothelium and release enzymes and toxic oxygen radicals
oxygen radicals (oxidative stress) oxidize ldl and further injure vessel
oxidized ldl causes smooth muscle proliferation and activate further immune and inflammatory response
oxidized ldl penetrates into the intima of artery and (is) engulfed by macrophages
macrophage filled with oxidized ldl are called foam cell
foam cells form lesion called fatty streak
fatty streak produce more toxic oxygen and leads to fibrous plaque formation
raptor of plaque called complicated plaque can lead to formation of thrombus
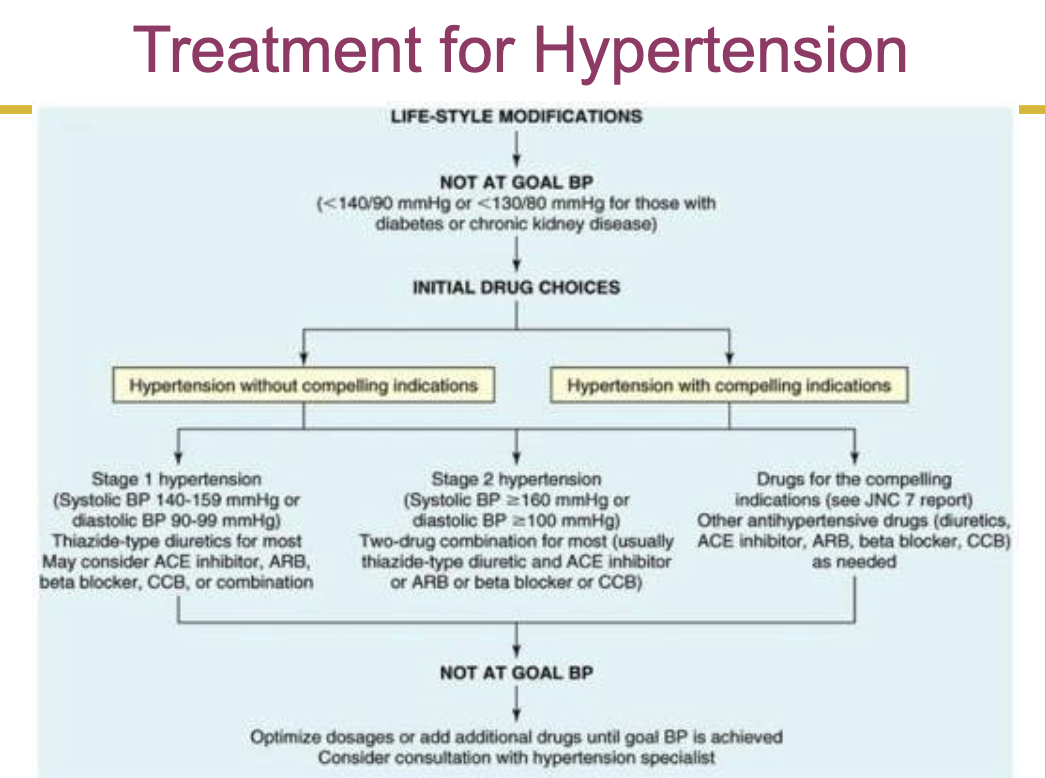
hypertension
sustained elevation of arterial blood pressure
hypertension could lead to ischemia of the tubule in kidney, where ischemia of tubule will lead to dysfunction of glomeruli
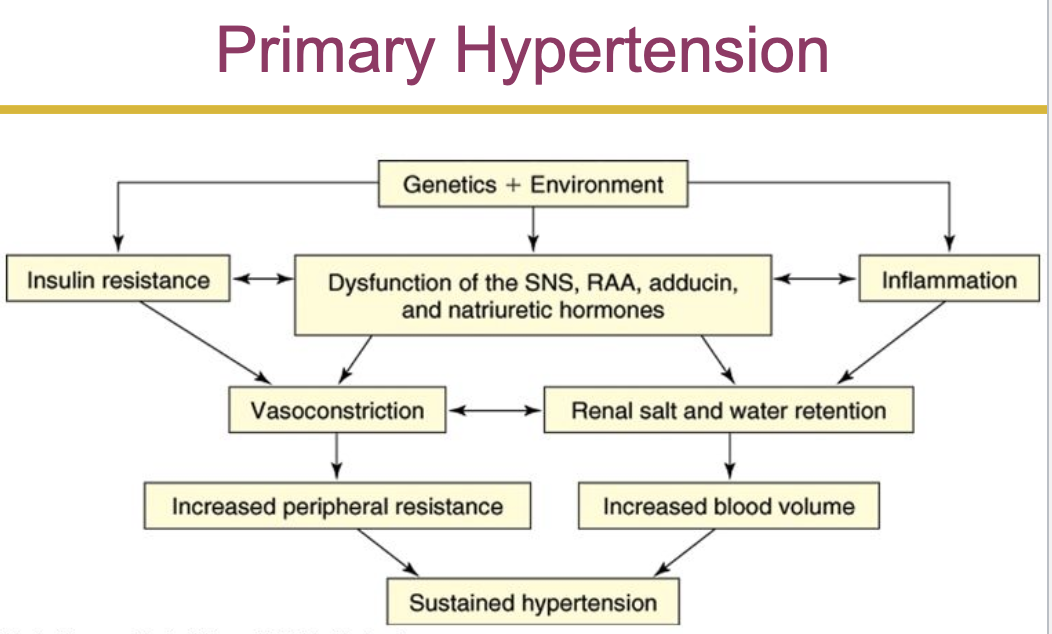
primary hypertension
aka essential or idiopathic hypertension
genetic and environmental factors
affect 90-95% of individuals with hypertension
in healthy individual the renin angiotensin system provides important homeostatic balance
angiotensin 2 is responsible for the hypertrophy of myocardium associated with hypertension
secondary hypertension
caused by a systemic disease process that raises peripheral vascular resistance or cardiac output
isolated systolic hypertension
elevations of systolic pressure are caused by increases in cardiac output, total peripheral vascular resistance, or both
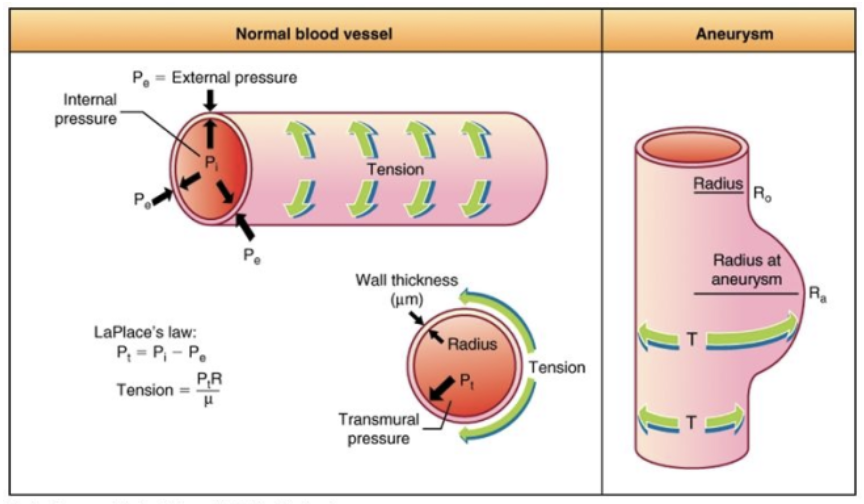
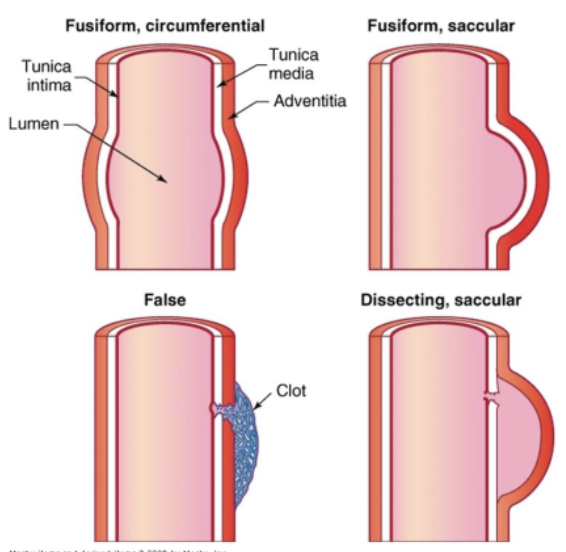
aneurysm
local dilation or outpouching of a vessel wall or cardiac chamber
plaque formation (in atherosclerosis) erodes the vessel wall and could cause aneurysms
thrombus formation
blood clot that remains attached to the vessel wall
roughening, inflammation, and traumatic injuries of the endothelium, and low blood pressure of the vein or artery promote clot formation
thromboembolus is a detached thrombus
embolism
bolus of matter that is circulating in the bloodstream
dislodged thrombus, air bubble, amniotic fluid, aggregate of fat, bacteria, cancer cells, or a foreign substance
deep vein thrombosis is the usual source of pulmonary emboli
peripheral artery disease
atherosclerotic disease of the arteries that perfuse the limbs
intermittent claudication
obstruction of arterial blood flow in the iliofemoral vessels resulting in pain with ambulation
peripheral artery disease:
thromoboangiitis obliterans (buerger disease) is an inflammatory disorder of small and medium sized arteries in the feet and sometimes in the hands
mainly in young men who smoke
resulting in the formation of nonatherosclerotic lesions
causes pain, tenderness, and hair loss in the affected area
symptoms are caused by slow, sluggish blood flow
can often lead to gangrenous lesions
raynaud phenomenon and raynaud disease
a vasospastic disorder of the small arteries and arterioles of the fingers and less commonly the toes
diseases of the veins:
varicose veins
a vein in which blood has pooled
distended, tortuous (twisted, elongated, or abnormally curved), and palpable veins
caused by
trauma or gradual venus distention
damage to the valves with veins
coronary artery disease:
any vascular disorder that narrows or occludes the coronary arteries
atherosclerosis is the most common cause
coronary artery disease can diminish the myocardial blood supply until deprivation impairs myocardial metabolism enough to cause ischemia
cardiac cells can withstand ischemic conditions and still return to a viable state for 20 min
(im assuming they can withstand it for 20 min)
risk factors
dyslipidemia- elevated plasma lipoproteins
hypertension- increases the risk by 2-3 fold
cigarette smoking- nicotine stimulates release of epinephrine and norepinephrine
epinephrine and norepinephrine stimulate release of free fatty acid
epinephrine and norepinephrine increases heart rate and blood pressure
smoking also increases ldl and decreases hdl- indicator of atherosclerosis formation
hdl is protective for the development of atherosclerosis
ldl is manufactured by the liver and primarily contains cholesterol and protein
diabetes mellitus increases the risk by 2 fold for death and 6 fold for stroke
obesity/sedentary lifestyle
myocardial ischemia
local, temporary deprivation of the coronary blood supply
develops if the supply of coronary blood cannot meet the demand of myocardium for oxygen and nutrients
caused most commonly by formation of atherosclerotic plaque in the coronary circulation
some plaque are unstable and rupture resulting thrombus formation
myocardial ischemia can also be caused by hypotension or low oxygen delivery
if the vessel obstruction is not reversed, myocardial ischemia leads to myocardial infarction
manifestation
stable angina- chronic coronary obstruction that causes reoccurring pain
prinzmetal angina- occurs bc of vasospasms of one or more coronary arteries and often during sleep. causes unpredictable pain
silent ischemia- myocardial ischemia that does not cause detectable symptoms
angina pectoris- chest discomfort (pain) caused by myocardial ischemia
the pain is presumably caused by lactic acid build up
the pain is usually relieved by rest
diagnosis
ecg during the attack of angina (most individuals will have normal ecg in the absence of pain)
ecg could give indication of coronary artery involved
exercise stress testing
spect (single photon emission computed tomography)
treatment
coronary angiography
coronary artery bypass graft
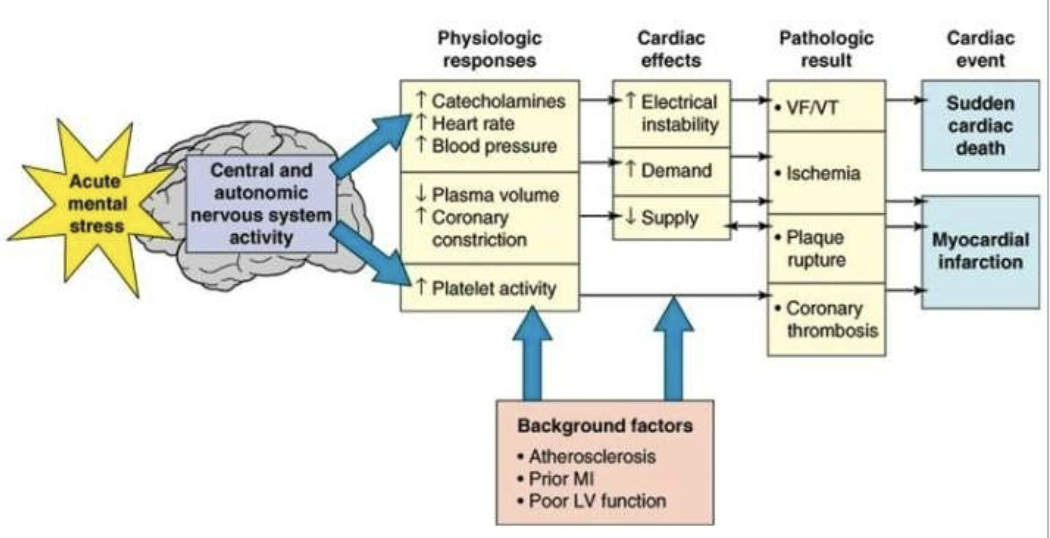
progression of atherosclerosis plaque could be sudden and lead to acute coronary syndrome
acute coronary syndromes
myocardial infarction
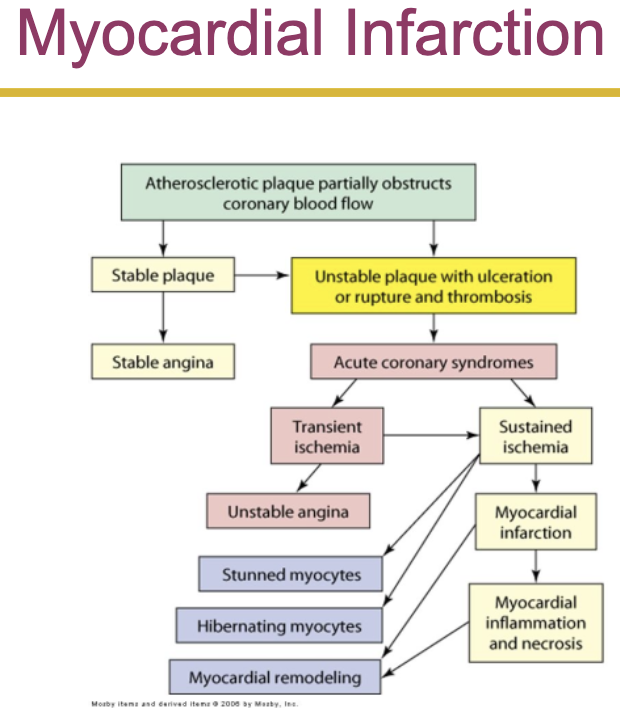
results from prolonged ischemia
prolonged ischemia leads to cellular injury- cardiac cells can withstand ischemic condition for about 20 min before necrosis or cellular death takes place
anaerobic respiration leads to accumulation of lactic acid leads to acidosis
myocardial tissue have poor buffering system
acidosis makes myocardial tissue more vulnerable to damage
mi causes both structural and functional damage
repair- mi causes severe inflammation response that ends w wound repair (synthesis of scar tissue)
when scar tissue replaces the myocardium after a mi, the forming scar tissue is very mushy and vulnerable to injury at about day 10-14 after mi
manifestation
sudden, severe chest pain
symptoms as angina but pain is severe and prolonged in mi
radiation of pain to the left side (arms, jaw, back)
catecholamine causes sympathetic stimulation (causing vasoconstriction- cool and clammy skin)
diagnosis
clinical symptoms: elevated levels of troponin, creatine kinase (ck), and lactic dehydrogenase (ldh)
mi can occur in various regions of heart well
identification of q wave and changes in st segments and t wave can localize the affected area
st elevation of electrocardiogram pattern indicate that thrombus in a coronary artery lodged permanently in the vessel and the infarction extends through the myocardium from the endocardium to the epicardium
treatment
immediate admission to hospital
aspirin, heparin, pain killer, (sublingual nitroglycerine and morphine sulfate)
oxygen administration if surgery is not available immediately
disorders of the heart wall:
disorders of the pericardium
acute pericarditis: a sudden onset of severe chest pain that radiates to the back and worsens w respiratory movement and when laying down
(isnt that inflammation bc itis??? symptoms ig?)
disorders of the myocardium:
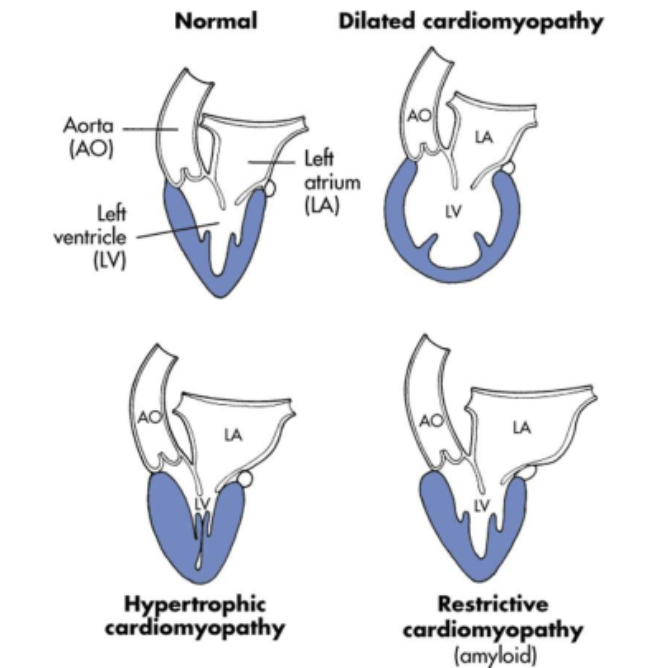
cardiomyopathies- diverse group of disease that primarily affect myocardium
develops as a result of cardiovascular disorder such as ischemic heart
cardiopathy are classified as
dilated cardiomyopathy (congestive cardiomyopathy)- characterized by ventricular dilation and grossly impaired systolic function, leading to dilated heart failure
hypertrophic cardiomyopathy- thickening of myocardium (disproportionate thickening of the interventricular septum)
restrictive cardiomyopathy- usually caused by an infiltrative disease of the myocardium, such as amyloidosis, hemochromatosis, or glycogen storage disease
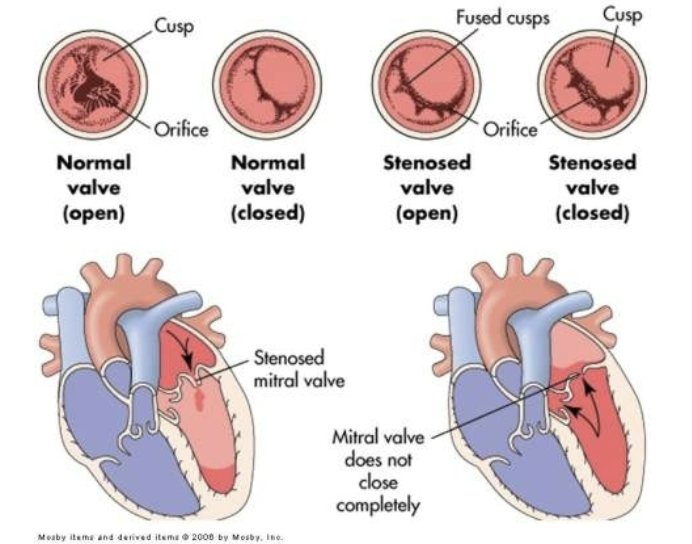
disorders of the endocardium:
disorders of the endocardium (innermost lining of the heart) are damages to the heart valves
valvular dysfunction- rheumatic fever is the primary cause of aortic and mitral regurgitation and stenosis
valvular stenosis- the orifice is constricted and narrowed - increasing the workload of cardiac chamber behind the diseased valve - increasing the pressure to overcome the resistance
aortic stenosis- dyspnea on exertion
mitral stenosis
valvular regurgitation- the valve cusps fail to shut completely permitting back flow of blood
aortic regurgitation
mitral regurgitation
tricuspid regurgitation
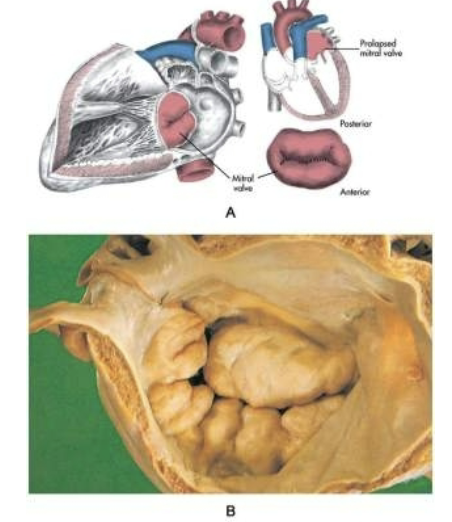
mitral valve prolapse syndrome- cusps of valve billow upward (prolapse) during atrium systole
diagnosis
echocardiography
cardiac catheterization prior to surgery
treatment
temp: diuretics and vasodilators
surgery to repair or replace the valve
cardiac complication of aids:
endocarditis- infective endocarditis is most often caused by bacteria due to genitourinary instrumentation, dental procedure, hemodialysis, and intravenous drug use
cardiomyopathy- dilated cardiopathy is the most common cardiac disorder associated with aids, resulting from myocarditis and infective endocarditis
myocarditis
pericarditis
heart failure:
general term used to describe several types of cardiac dysfunction that result in inadequate perfusion of tissues w blood borne nutrients
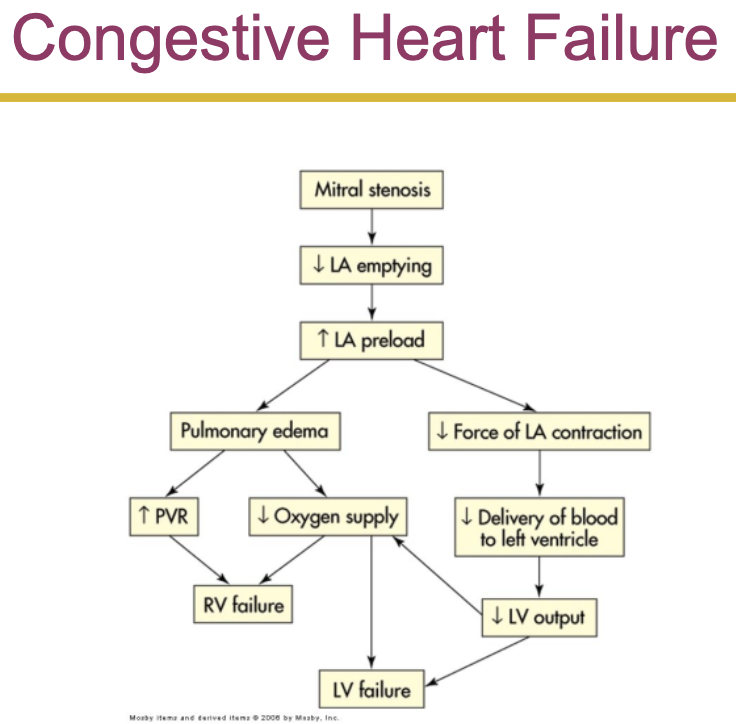
congestive heart failure
systolic heart failure
angiotensin 2 increases preload and increases afterload stroke volume
im guessing theres not enough?
inability of the heart to generate adequate cardiac output to perfuse tissues
diastolic heart failure
pulmonary congestion despite normal stroke volume and cardiac output
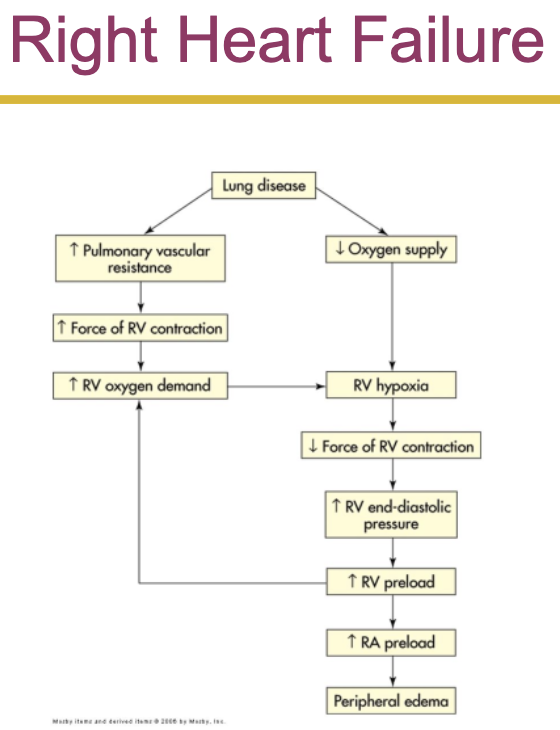
right heart failure
most commonly caused by a diffuse hypoxic w pulmonary disease and elevated pulmonary vascular resistance
can result from an increase in left ventricular filling pressure that is reflected back into the pulmonary circulation
high output failure
inability of the heart to supply the body with blood borne nutrients, despite adequate blood volume and normal or elevated myocardial contractility
dysrhythmias:
disturbance of the heart rhythm
range from occasional ‘missed’ or rapid beats to severe disturbances that affect the pumping ability of the heart
can be caused by an abnormal rate of impulse generation or abnormal impulse conduction
ex.
tachycardia, flutter, fibrillation, bradycardia, premature ventricular contractions (pvcs), premature atrial contractions (pacs), asystole