8.1 the cardiovascular and respiratory system
the cardiovascular system
- heart
- blood vessels
- blood
function
- delivery of O2, fuel and nutrients to the tissues of the body
- removal of CO2 and waste products from the tissues
- maintenance of a constant body temperature - thermoregulation
- prevention of infection (immune function)
the heart
- formed from myocardium, a specialized muscle tissue
- surrounded by percardium (tough protective sac that fits loosely over the heart) which allows the heart to expland and contract
- epicardium - lines the outside of the heart
- endocardium - lines the inside of the heart
- made up of 4 separate chambers:
- atria and ventricles
- considered a double pump and is divided into the right and left heart separated by the interventricular septum
- right heart: pumps deoxygenated blood to the lungs (pulmonary circulation)
- left heart: pumps oxygenated blood to the rest of the body (systemic circulation)
- working out the heart increases the myocardium
- working out your cardio will increase the size of the ventricles to pump more blood
- healthy hearts have a lower BPM but pump more blood per pump
proper blood flow through the heart
- deoxygenated blood enters the right atrium of the heart through the superior and inferior vena cava
- deoxygenated blood travels from the right atrium through the tricuspid valve into the right ventricle
- deoxygenated blood is pumped from the right ventricle through the pulmonary valve into the pulmonary artery
- the pulmonary artery carries the blood to the lungs to be oxygenated
- blood from the lungs travels through the pulmonary veins into the left atrium of the heart
- oxygenated blood travels from the left atrium through the mitral valve into the left ventricle
- oxygenated blood is pumped from the left ventricle through the aortic valve into the aorta
- the aorta carries the blood to other arteries that bring the blood to the rest of the body
excitation of the heart
- the sinoatrial node (SA node)
- specialized region of tissue found in the wall of the right atrium
- the location where electrical signals are initiated (pacemaker)
- atrioventricular node (AV node)
- passes electrical signal from atria into ventricles
- passes electrical signal to the bundle of His (atrioventricular bundle)
- bundle of His pass electrical signal to the purkinje fibers
- purkinje fibers pass electrical signals to the myocardium
- the myocardium contracts
- leads to contraction of the heart
- leads to the pumping of blood
electrical activity of the heart
- measured using an electrocardiogram (ECG)
- graphical representation of electrical sequence of events occurring with each contraction of the heart
- each wave generated during contraction is named
- P wave - represents contraction of the atria
- QRS complex - represents contraction of the ventricles
- T wave - represents the filling of the ventricles
- missing - filling of the atria (masked by the QRS complex)
cardiac cycle
- the cardiac cycle is a series of events occurring through one heartbeat
- diastole phase - relaxation, heart fills with blood
- systole phase - contraction, heart contracts and ejects blood
the vascular system and blood
- the vascular system is a network of vessels the transport blood throughout the body, vessels are divided into 4 categories
- arteries - carry oxygenated blood away from the heart to different organs (elastic and do not have valves)
- arterioles - smaller arteries
- capillaries - responsible for the exchange of gases and nutrients with the tissue
- venules - smaller veins
- veins - returns deoxygenated blood back to the heart (elastic and do have valves)
the return of blood from the veins
- 4 tools that assist the body in the return of the blood in the veins to the heart
the skeletal muscle pump
- upon contraction of skeletal muscle, blood is pushed back to the heart
the thoracic pump
- pressure in the veins in the chest decrease while pressure in the abdominal cavity increase upon intake of breath
- blood flows from high pressure to low pressure, pushing the blood from the abdomen to the thoracic cavity
the nervous system
- sends signals to the veins allowing the veins to constrict and allow more blood to go back to the heart
valves in the veins
properties of blood
- plasma (55% of blood)
- fluid component of blood (mostly water)
- blood cells
- red blood cells (erythrocytes) (45%)
- made in bone marrow
- transports O2 and CO2 in the blood
- transports nutrients and waste
- contains hemoglobin
- white blood cells (leukocytes) (<1%)
- destroys foreign elements
- critical in the function of the immune system
- platelets
- regulate blood clotting
blood pressure
- blood pressure is the force exerted by the blood against the walls of the arteries
- measuring blood pressure - systolic pressure over diastolic pressure
- systolic BP - pressure observed in the arteries during contraction phase
- diastolic BP - pressure observed during relaxation phase
normal BP
- normal bp is 120mmHg over 80mmHg
- hypertension
- BP greater than 140 over 90
- factors affecting BP that are controllable
- diet (sodium, saturated fat, cholesterol)
- aerobic exercise
- stress
- factors we do not have control over
- age
- genetics
BP and health
- blood pressure is a commonly used indicator of health
- elevated BP (hypertension) is a major risk factor for cardiovascular disease
- aerobic exercise training leads to improvements in resting blood pressure within three weeks to three months of starting exercise
- further improvements are made when exercise is coupled with improvements in diet (low fats, and cholesterol and high in fiber and complex carbohydrates)
- cardiovascular disease: atherosclerosis - associated with the narrowing of the coronary arteries resulting from the accumulation of hard deposits of cholesterol called plaque in the lumen of the arteries
- arteriosclerosis - the hardening of the arteries
- myocardial infarction: heart attack - blockage involving the death of some of the cardiac muscle
cardiac output and stroke volume
cardiac output (q) - the amount of blood pumped out of the left ventricle in one minute (L/min)
stroke volume (SV) - the amount of blood pumped out of the left ventricle with each beat (mL)
- Q = HR x SV
average cardiac output during exercise
- 25-30 L/min
average cardiac output at rest
- 5-6 L/min
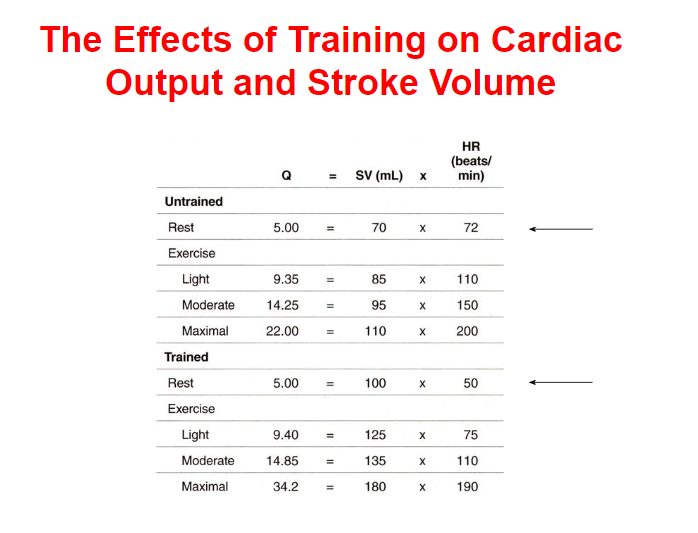
the effects of aerobic training on the cardiovascular system
- Increase in venous return
- Increase in ventricular volume and thickness of ventricle walls (myocardium) = increase in SV
- Increase in Q
- Increase in the number of capillaries that deliver oxygen to the myocardium
- Increase in diameter of coronary arteries
- Increase in blood volume
- Increase in red blood cells
- at rest: increase in SV and decrease in HR
- during exercise: blood flow is redirected to the muscles from the organs (except the brain where blood flow is unaltered)
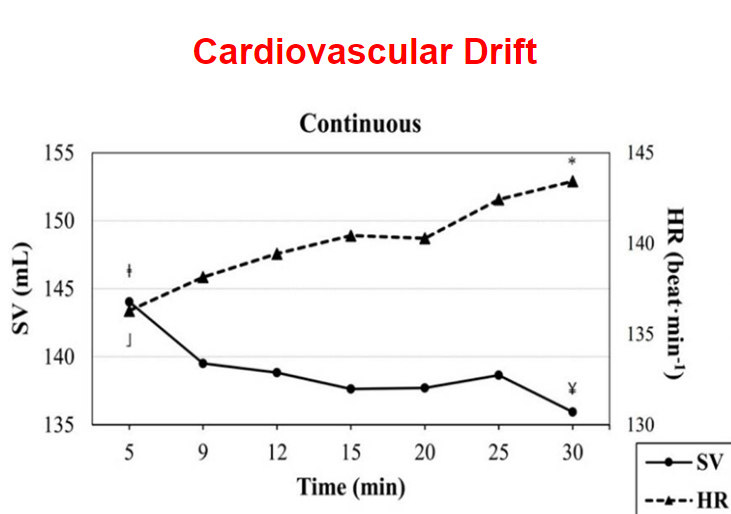
cardiovascular drift
- cardiovascular drift is a phenomenon that occurs when during an easy steady state aerobic activity (run) there is an increase in HR and decrease in SV to maintain Q
- begins after 10-20 minutes (without an increase in effort)
- heightened during warm temperatures
- caused by:
- increase in body temperature and redistribution of blood flow to the skin for cooling
- decrease in plasma volume due to dehydration
how endurance and resistance exercise affect blood pressure
- during endurance exercise
- systolic blood pressure increases (but diastolic does not due to vasodilation of the arteries)
- during resistance exercise
- systolic and diastolic blood pressure increases
- post exercise hypotension
- blood pressure drops below normal resting values persisting for about 24 hrs after exercise due to pooling of blood in vasodilated muscle beds
the respiratory system
- composed of structures that allow
- passage of air from outside the body to the lungs
- gas exchange to occur
- 3 main functions
- supply O2 to the blood
- remove CO2 from the blood
- regulate blood pH
- divided into 2 zones
- conductive zone
- respiratory zone
the conductive zone
- composed of structures that transport air to the lungs
- mouth and nose
- pharynx
- larynx
- trachea
- primary and secondary bronchi
- tertiary and terminal bronchioles
- warms and humidified air
- filters air (hair and mucous)
the respiratory zone
- composed of structures involved with the exchange of gases
- respiratory bronchioles
- alveolar sacs (ab. 300 million)
mechanisms of breathing
- inspiration
- contraction of diaphragm (lowers)
- thoracic cavity expands
- air enters
- expiration
- relaxation of diaphragm (goes up)
- air is expelled
ventilation and control of ventilation
- ventilation (Ve) - the volume of air that is moved by the lungs in one minute
- can increase up to 100/200 L of air/minute
- tidal volume (Vt) - volume of air in each breath
- respiratory frequency (f) - the number of breaths per minute
- at rest - 12 breaths/min
- during exercise - 30/40 breaths/min
- central chemoreceptors are found in the brain stem and they detect changes in brain CO2 and pH
- peripheral chemoreceptors are found in places like the aorta
adaptations to training
- regular aerobic training leads to very few adaptations in the respiratory system at rest
- increase in Vt
- decrease in f
- no changes in Ve
- during sub-maximal exercise
- increase in Vt
- decrease in f
- increase in Ve
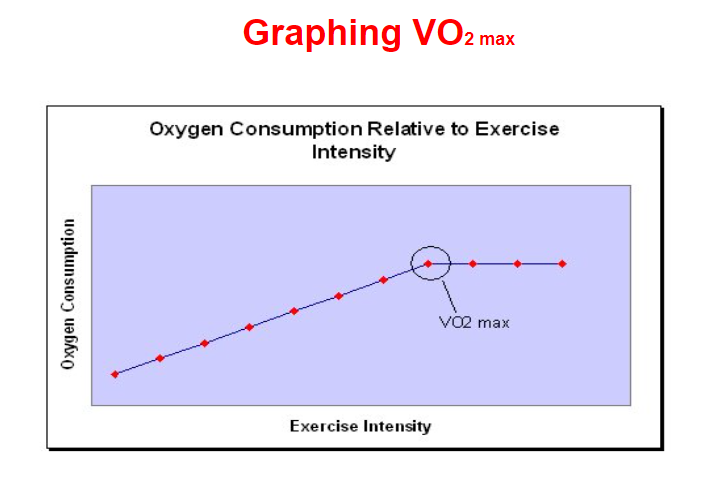
maximal oxygen consumption (VO2 max)
- maximum rate of oxygen consumption (VO2 max) - maximal amount of oxygen that can be taken in and used for metabolic production of ATP in 1 minute/kg of body weight during maximal exercise
- measured while participant performs incremental exercise to exhaustion
- used as a measure of aerobic fitness
- the limiting factor in healthy people is the cardiovascular system, when this system is unable to meet the demands of the working muscle and deliver adequate amounts of oxygen
- limitations due to:
- inadequate Q
- inadequate hemoglobin concentration
how is VO2 max calculated
- VO2 max - mL/kg/min
- VO2 max = (volume of air inspired x %O2 inspired) - (volume of air expired x %O2 expired)
- average female in the good range is 40-43 mL/kg/min
- average male in the good range is 46-50 mL/kg/min
- the most effective way to improve VO2 max is to train using high intensity interval training where the athlete maximizes the amount of time he/she is at or close to VO2 max
- VO2 max is largely based on genetics, specifically hemoglobin concentrations and types of muscle fibers
- VO2 max peaks at age 18 and decreases by 1% per year
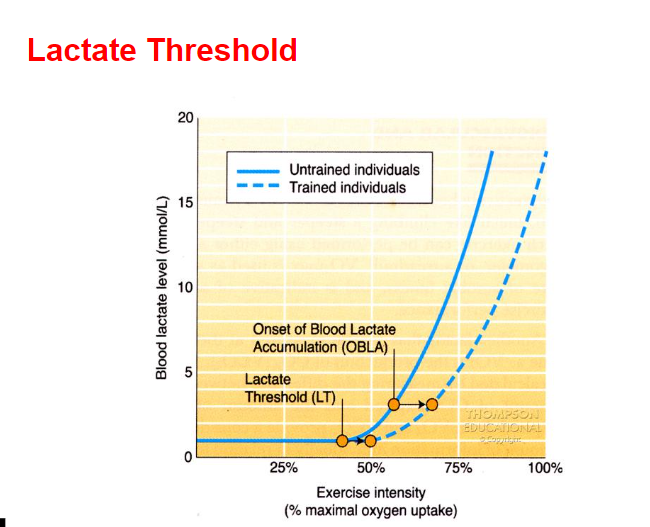
ventilatory and lactate thresholds
- ventilatory threshold - point when ventilation increases much more rapidly than workload
- usually occurs at 65-85% of VO2 max depending of level of fitness
- due to increase in lactic acid and decrease in blood pH (due to increase in CO2)
- lactate threshold - point where blood lactate exceeds the body’s ability to clear it
- the best predictor of performance in endurance events
- onset of blood lactate accumulation - point when blood lactate levels begin to accumulate rapidly
- both LT and OBLA can be shifted to the right with aerobic training
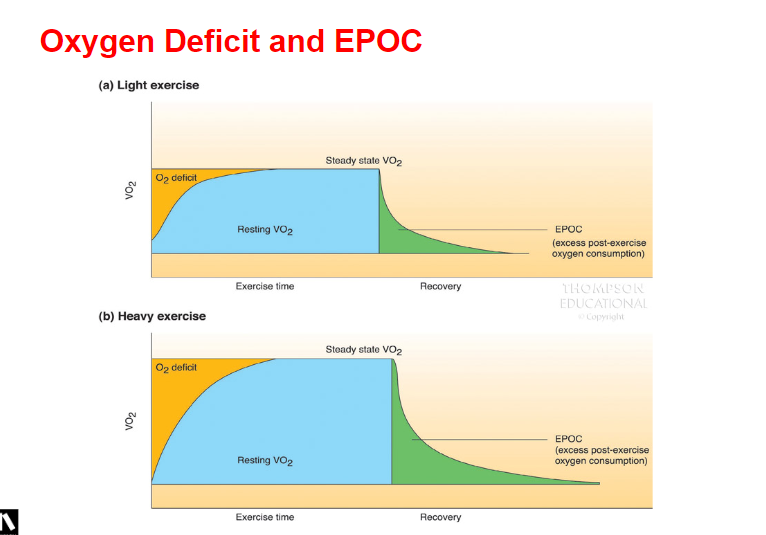
oxygen deficit
- ultimately the delivery of oxygen is matched to the demand of oxygen but there is a lag since the physiological mechanisms are not instantaneous
- oxygen deficit - the difference between the oxygen required to perform a task and the oxygen actually consumed prior to reaching a new steady state
- steady state - submaximal exercise levels where oxygen uptake and heart rate level off, where oxygen demands and energy production are evenly balanced and where the body maintains a steady level of exertion for a fairly extended period of time
- the trained person will reach this plateau quicker than an untrained person and will have a smaller oxygen deficit for an exercise of a given duration
excess post-exercise oxygen consumption (EPOC)
- excess post-exercise oxygen consumption - the additional oxygen taken in during this recovery period in order to restore balance
- the additional oxygen requirements are used for
- replenish oxygen to the various body systems that were taxed during the exercise which include
- refilling phosphocreatine reserves in muscles
- replenishing oxygen in the blood and tissue
- lowering elevated heart rate and breathing
- lowering body temperature
- increased blood lactate removal
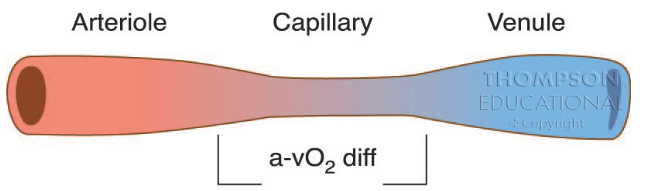
amount of oxygen delivered to the skeletal muscle
a-VO2 difference - one way to measure the amount of oxygen that has been delivered to a skeletal muscle by measuring the amount of arterial blood before it arrives and venous blood after it leaves indication how much oxygen is removed from the blood in the capillaries
at rest: 4.5 mL/100L/min
during exercise: 16mL/100L/min (80-85% extraction)