Skeletal Tissue
Functions of the skeletal system
Support
Protection
Movement
Storage - Calcium and Phosphorus
Blood cell production
Components of Skeletal System
Bone
Cartilage: 3 types
Hyaline - most common, ends of bones; smooth joint mount
Fibrocartilage - resist mechanical loads
Elastic - Bend and move to function: recoil
Tendons and ligaments
Bone Histology
Bone Matrix
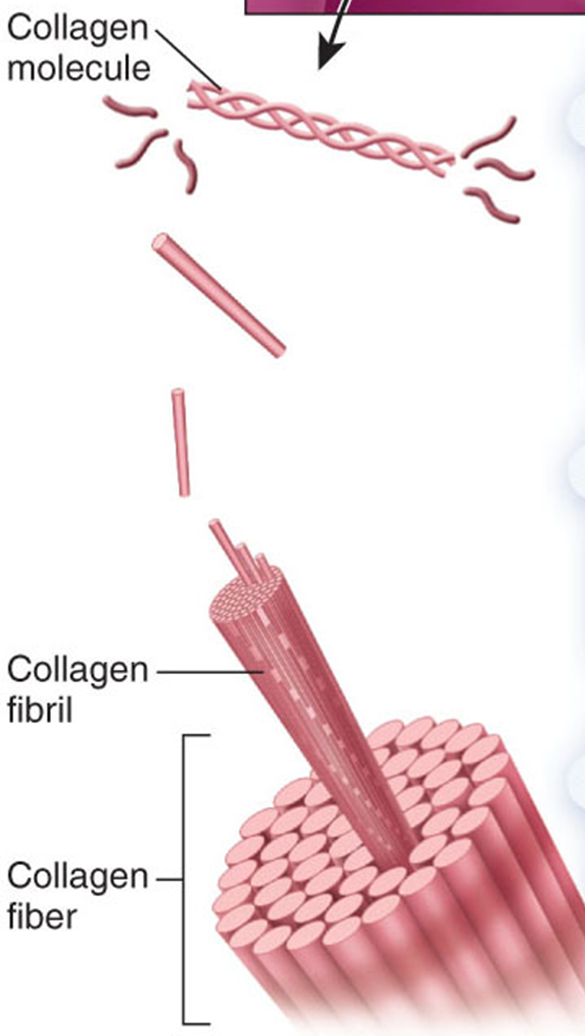
Organic - collagen and proteoglycans: Alive: changing
Inorganic - hydroxyapatite: CaPO4 Crystals (calcium phosphate)
Collagen
Collagen - Found in most issues: Type I collagen in bone, tendons, skin
Proteoglycans
Glycosaminoglycans (GAGs)
Resist compression: Gel like component
Bone cells
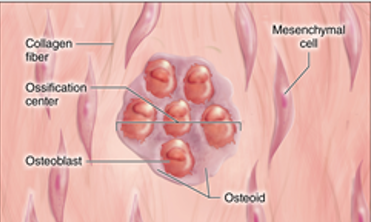
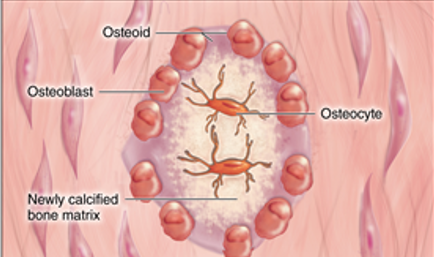
Osteoblasts
formation of bone via ossification or osteogenesis
Ossification - formation of bone by osteoblasts
Osteogenic Cells - become osteoblasts
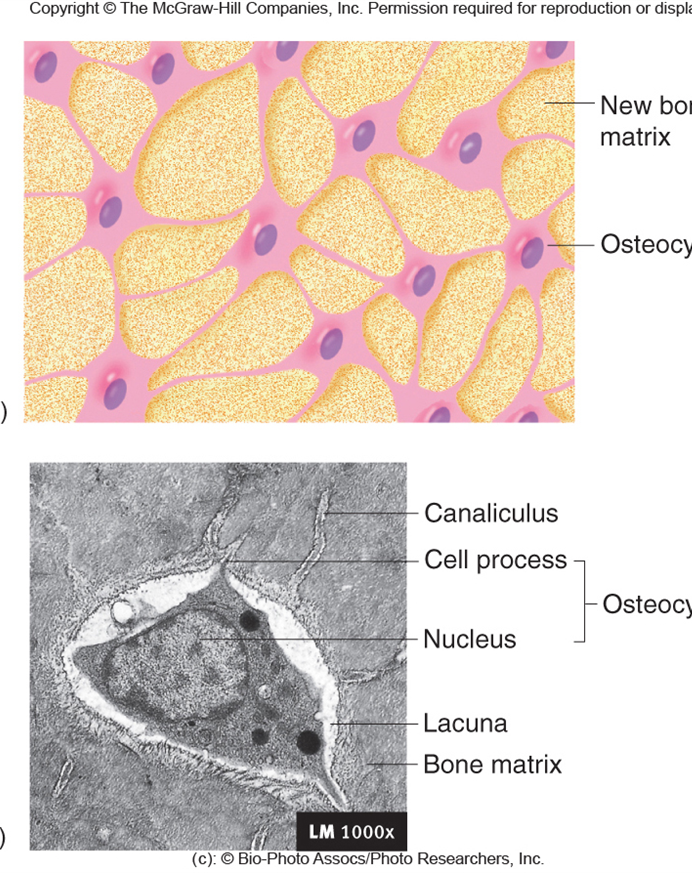
Osteocytes
Lacunae - house and protect osteocytes. found in rings of asse matrix. Spaces occupied by osteocyte cell body
Canaliculi - allows cans to communicate with each other Canals occupied by osteocyte cell processes
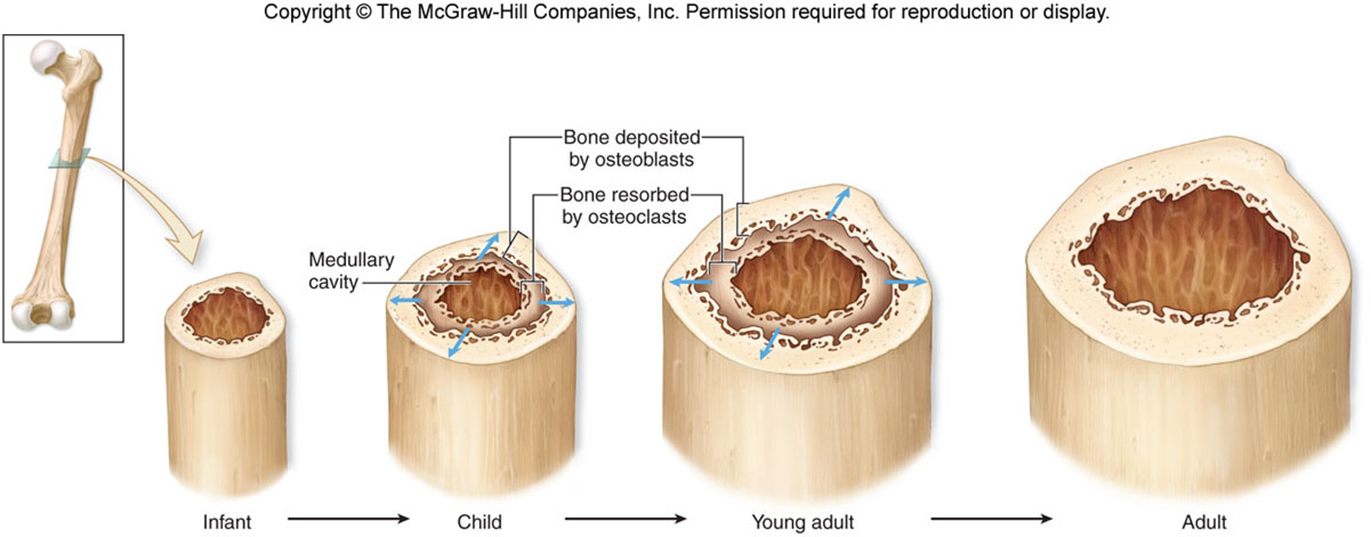
Osteoclasts
Destruction of bone: Necessary when bones need repair or nutrients in bone are needed elsewhere in the body: regulated by hormones: resorption is done w/ enzymes and low PM
Intramembranous ossification
Converts woven bone into Lamellar bone
Woven Bone - collagen fibers randomly oriented
fetal development
fracture repair
conversion
Lamellar bone - fibers are oriented in on direction: strong bone: lamellae fibers
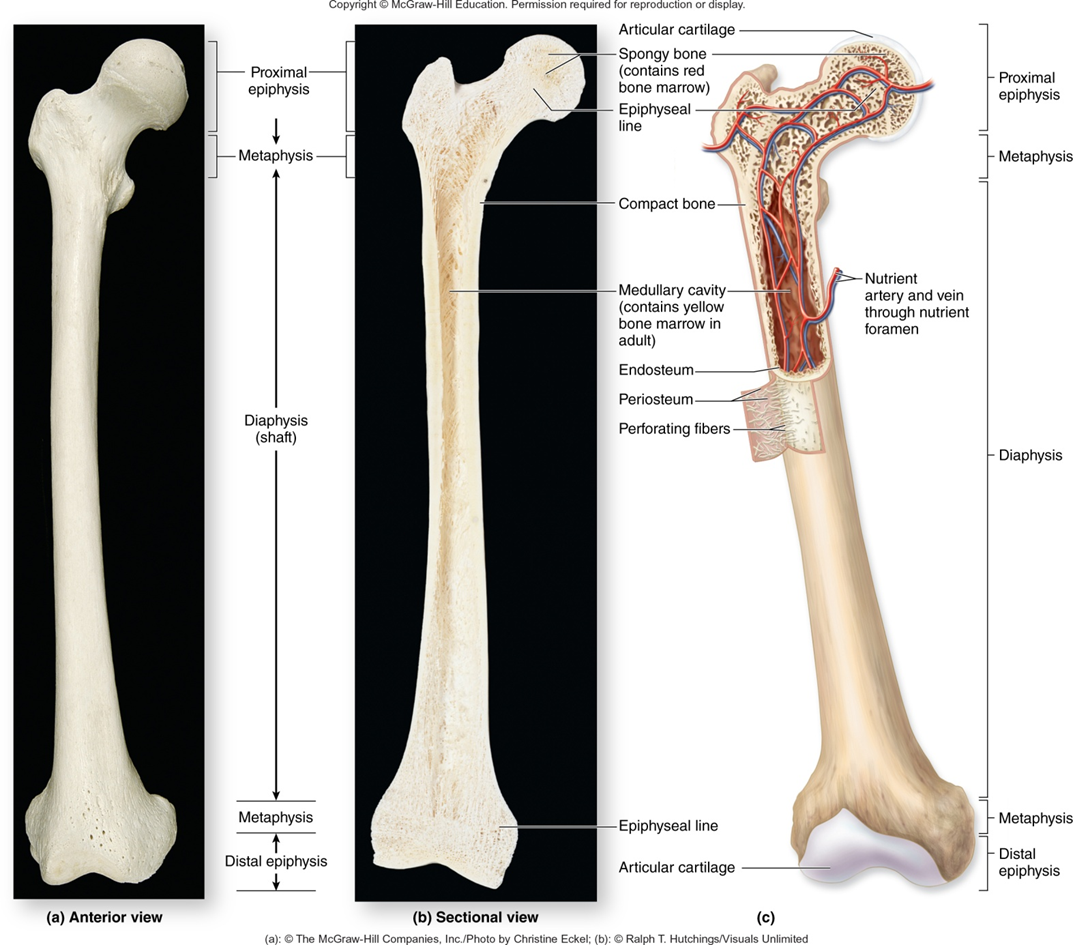
Spongy Bone
more space, less bone
Trabeculae - interconnecting rods or plates of bone. spaces filled with marrow.
Cancellous
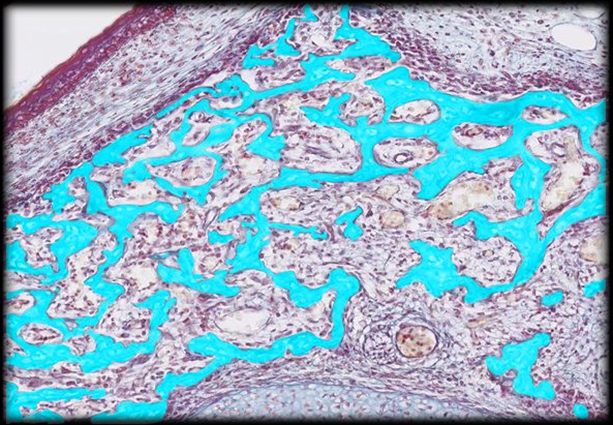
Bone Marrow
Red Marrow - ends of tons bones and center of other bones: manufactures blood cells
Yellow Marrow - in diaphysis of long bones; compose a of mainly fat; Deep to red
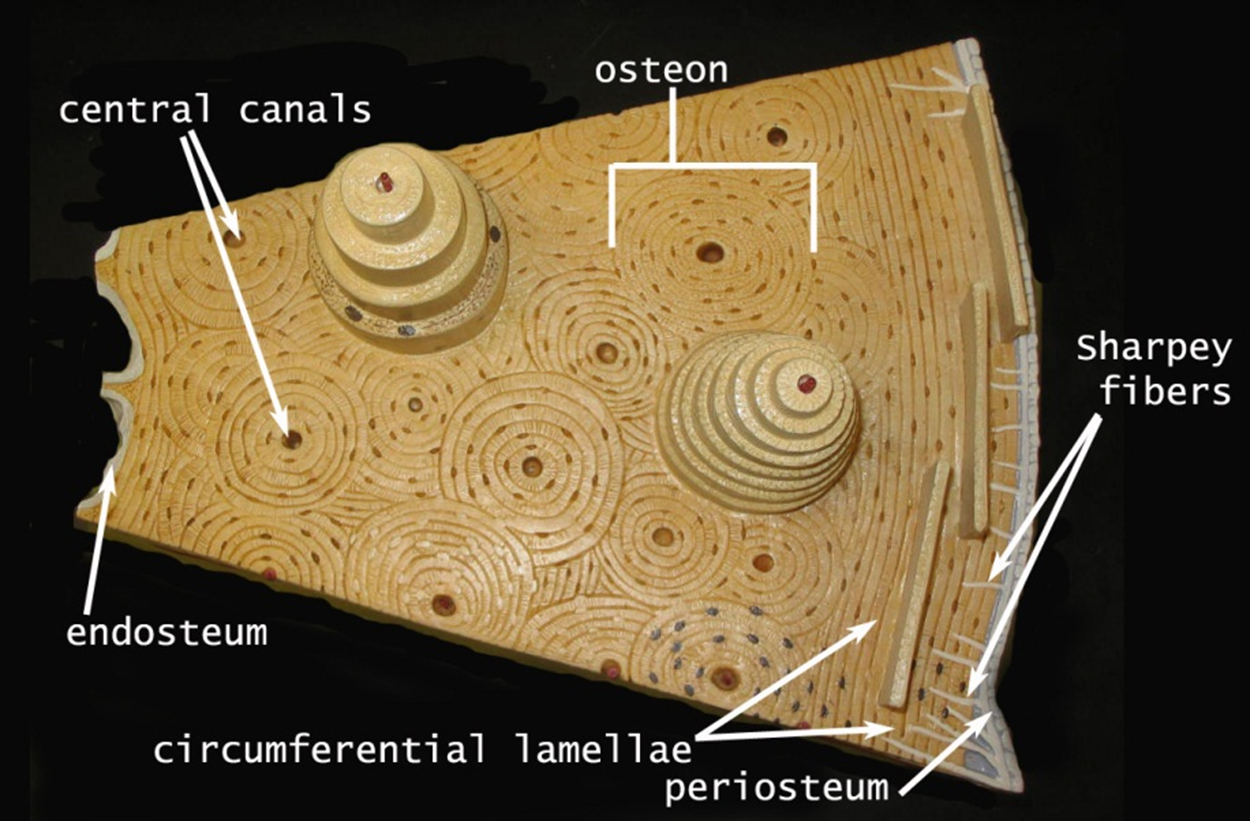
Compact Bone
Osteons (Haversian system) - Blood vessel-filled central canal (Haversian)
Concentric lamellae of bone surround central canal
Lacunae and Canaliculi contain osteocytes and Fluid
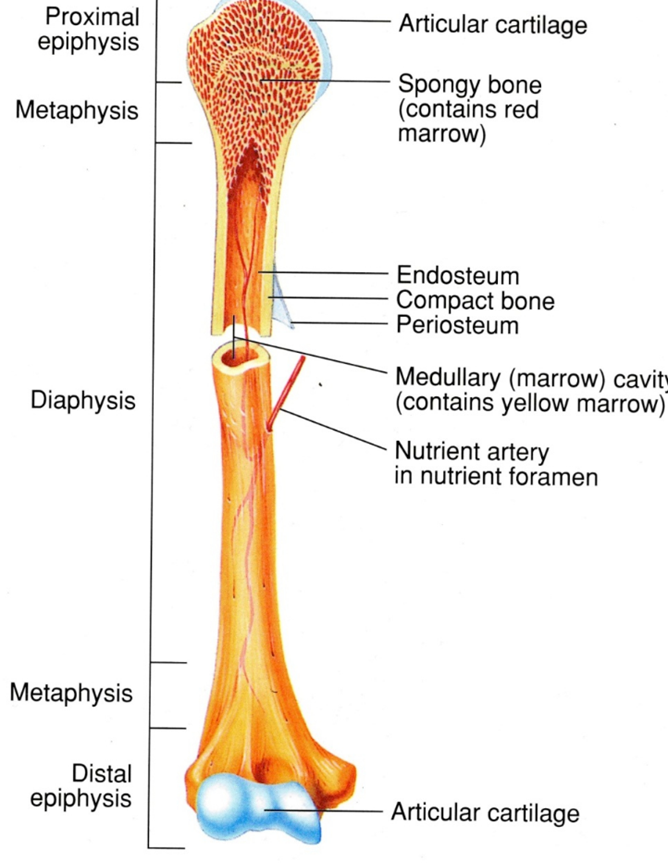
General structure and Gross Anatomy of Long Bones
Diaphysis - elongated cylindrical shaft, Yellow Bone Marrow
Epiphysis - knobby, Enlarged regions at ends: strengthens joints: Attach site for tendons and ligaments rec bone marrow
Metaphysis - region between diaphysis and epiphysis: contains epiphyseal (growth) plate
Articular cartilage - Thin layer of hyaline cartilage covering the epiphysis: reduces friction and absorbs shown in movable joints
Medullary Cavity - Hollow, cylindrical space in diaphysis: contains yellow rea bone marrow in children
Endochondral Ossification
Cartilage formation begins at end of fourth week of development
Some ossification at about week eight:
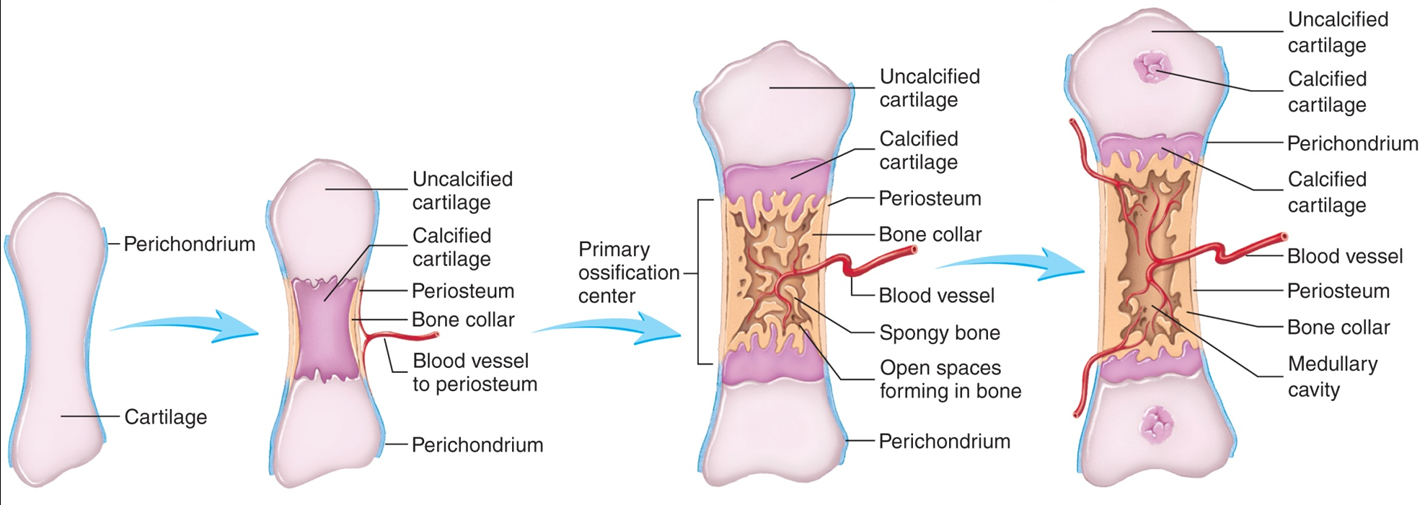
Steps of Ossification
Fetal hyaline cartilage develops
Cartilage calcifies and a periosteal bone collar forms
Primary ossification center forms in diaphysis
Secondary ossification centers form in diaphysis
Bone replaces cartilage, except articular cartilage and epiphyseal plates
Epiphyseal Plates ossify and form epiphyseal lines
Endochondral Ossification - formation of long bones: Bone growth: bone healing: closure of epiphyseal plate is ossified becoming the epiphyseal line (12-15 yrs old)
Growth of Bone
Interstitial growth - long bones growth in length: occurs in epiphyseal plate
Appositional growth - bones growth in diameter: occurs in periosteum
Factors Affecting Bone Growth
Nutrition
lack of calcium and other nutrients during development can cause bones to be small
Vitamin D
necessary for absorption of calcium from intestines
Rickets - lack of vitamin D during Childhood
Osteomalcia - lack of vitamin ) during Adulthood
Vitamin C
Necessary for collaged synthesis by osteoblasts
lack of vitamin C can cause wounds not to heal and teeth to fall out
Hormones
Thyroid hormone required for growth of all tissues
sex hormones: Estrogen and testosterone: HGH
Bone Stress
Bone Repair
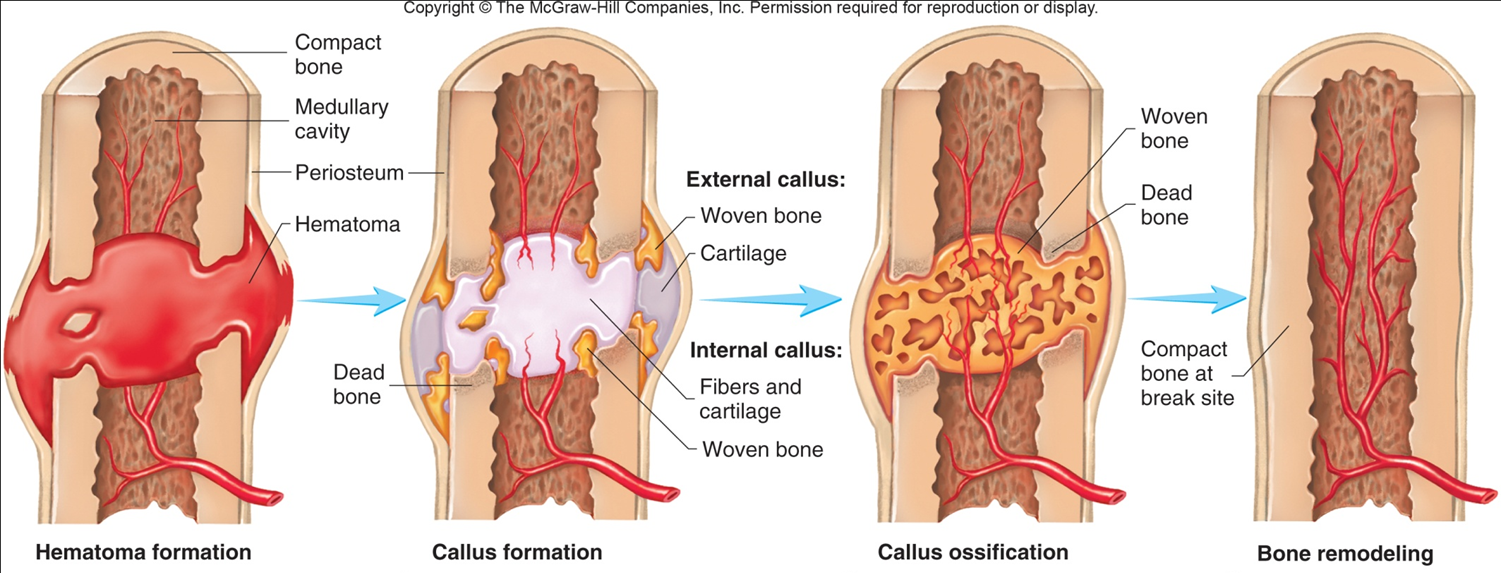
Ossification
Ossification centers form within thickened regions of mesenchyme
Osteoid undergoes Calcification
Woven bone and surrounding periosteum form

Lamellar bone replaces woven bone as compact and sponger, bone form
Cartilage
Consists of specialized cells that produce Matrix
Chondroblasts - form Matrixes
Chondrocytes - surrounded by Matrix launce
matrix - collaged and Proteoglycans
Perichondrium - Double-layer CT Sheath. Covers except at articulations
Inner - more delicate, has fewer fibers, contains chondroblasts
Outer - Blood vessels and nerves penetrate. No blood vessels in cartilage
Articular cartilage - covers bones at joints; has no perichondrium
Growth
Appositional - new cells at periphery
Interstitial - cells divide and add more matrix between the cells