Respiratory System Lecture Review
Chapter 23: Respiratory System Lecture Objectives - Answers
1. What is the difference between conducting and respiratory portions of the respiratory system? What are the anatomical structures associated with each?
Conducting Portion: Consists of structures that transport air but do not participate in gas exchange (e.g., nasal cavity, pharynx, larynx, trachea, bronchi).
Respiratory Portion: Includes structures where gas exchange occurs (e.g., alveoli).
2. As we move from the nasal cavity all the way down to the alveoli, how does the epithelium change and why?
The epithelium changes from pseudostratified ciliated columnar epithelium in the nasal cavity to simple squamous epithelium in the alveoli to facilitate gas exchange due to its thin structure.
3. What is the mucociliary escalator?
It is a defense mechanism in the respiratory system where mucus traps pathogens and particles, and cilia move them upwards to the pharynx for swallowing or expulsion.
4. How do the nasal sinuses and meatuses help with the function of the respiratory system?
Nasal sinuses and meatuses help humidify and filter the air entering the respiratory system, also reducing the weight of the skull and improving resonance of voice.
5. What are the 3 parts of the pharynx and what epithelium lines each?
Nasopharynx: Lined with ciliated epithelium.
Oropharynx: Lined with stratified squamous epithelium.
Laryngopharynx: Also lined with stratified squamous epithelium.
6. What are the 3 large cartilages that form the larynx? What are their functions?
Thyroid Cartilage: Forms the Adam's apple and provides support.
Cricoid Cartilage: Forms the base of the larynx.
Epiglottis: Prevents food from entering the trachea during swallowing.
7. How does the coughing reflex protect the glottis/vestibular fold?
The coughing reflex ejects air forcefully from the lungs, clearing irritants and foreign objects from the glottis or vestibular folds, thus protecting the airway.
8. What are the 2 smaller pieces of cartilages that are important for producing sound? How do they work with the vocal fold? What leads to a high pitch vs. low pitch sound (2 factors)? Why does our voice change when we have a sinus infection?
Arytenoid Cartilages and Corniculate Cartilages are important for sound production.
They adjust the tension and position of the vocal folds.
Higher pitch results from increased tension and length of vocal folds, while lower pitch results from decreased tension.
A sinus infection can cause swelling and mucus buildup, affecting vocal fold vibration and resonance, leading to voice changes.
9. Why are cartilages of the trachea "C-shaped"? What are the primary, secondary, and tertiary bronchi?
The "C-shaped" cartilages in the trachea allow for flexibility and support while keeping the airway open.
Primary (Main) Bronchi: Branch directly from the trachea.
Secondary (Lobar) Bronchi: Supply lobes of the lungs.
Tertiary (Segmental) Bronchi: Supply specific bronchopulmonary segments.
10. How does the tissue progressively change as we move from primary to tertiary bronchi to bronchioles/terminal bronchioles to respiratory bronchioles?
As airways branch smaller, the epithelium transitions from ciliated columnar to cuboidal epithelium and eventually to simple squamous epithelium in the alveoli. Cartilage decreases while smooth muscle increases, allowing greater flexibility and control of airflow.
11. What does sympathetic activation do to the bronchi? Parasympathetic stimulation?
Sympathetic Activation: Causes bronchodilation (widening of air passages).
Parasympathetic Stimulation: Causes bronchoconstriction (narrowing of air passages).
12. What 3 types of cells make up the alveoli? What does each of them do?
Type I Cells: Form the alveolar wall and facilitate gas exchange.
Type II Cells: Produce surfactant to reduce surface tension and prevent alveolar collapse.
Alveolar Macrophages: Remove debris and pathogens from the alveolar space.
13. What makes up the blood-air barrier and why is it efficient for gas exchange?
The blood-air barrier consists of the alveolar epithelium, fused basal laminae of alveolar and capillary endothelium. Its thin structure allows for efficient diffusion of gases (O2 and CO2) across it.
14. What is the cardiac notch in the lungs for? Is it on the left or right lung? What pleura lines the lungs vs. the thoracic cavity?
The cardiac notch accommodates the heart and is located on the left lung.
Visceral Pleura: Lines the lungs.
Parietal Pleura: Lines the thoracic cavity.
15. What is Boyle’s Law and how does this relate to pulmonary ventilation (inhalation or inspiration/exhalation or expiration)?
Boyle's Law states that decreasing the volume of gas increases its pressure and vice versa. During inhalation, thoracic cavity volume increases, leading to a decrease in intrapulmonary pressure, causing air to flow in. During exhalation, volume decreases, increasing pressure and pushing air out.
What does your diaphragm do? It contracts to increase the volume of the thoracic cavity during inhalation.
16. Why does an increased volume of thoracic cavity lead to increased lung volume?
An increase in thoracic volume lowers pressure within the lungs (intrapulmonary pressure), allowing air to flow in, thus expanding lung volume.
17. What is the difference between eupnea and hyperpnea?
Eupnea: Normal quiet breathing.
Hyperpnea: Increased depth and rate of breathing during exertion or need for oxygen.
18. How do diaphragm and intercostal muscles help with quiet breathing? What two other muscles are helpful for forced breathing?
Diaphragm: Main muscle for inhalation; contracts to increase thoracic volume.
Intercostal Muscles: Assist by contracting to expand the rib cage.
Accessory muscles for forced breathing: Scalenes and sternocleidomastoid muscles.
19. What is intrapulmonary pressure? How does the value change between cycles of inhalation and exhalation?
Intrapulmonary Pressure is the pressure within the alveoli. It decreases during inhalation (negative pressure) and increases during exhalation (positive pressure).
20. How does “compliance” affect the ability to breathe (lower value vs. higher value)? What 3 factors can affect compliance?
Lower Compliance: Indicates stiffer lungs, making breathing more difficult.
Higher Compliance: Means easier lung expansion during inhalation.
Factors affecting compliance: Lung tissue elasticity, surface tension in the alveoli, and thoracic cavity structure.
21. What is the formula for calculating respiratory minute volume? What about alveolar ventilation? What does this formula account for compared with respiratory minute volume?
Respiratory Minute Volume Formula: Tidal Volume × Respiratory Rate.
Alveolar Ventilation Formula: (Tidal Volume - Dead Space Volume) × Respiratory Rate.
Difference: Alveolar ventilation accounts for the volume of air that reaches the alveoli and participates in gas exchange, while minute volume includes all air breathed in and out, including dead space.
22. Know the 6 different respiratory “volumes” and what do they represent.
Tidal Volume (TV): Volume of air inhaled/exhaled in a normal breath.
Inspiratory Reserve Volume (IRV): Additional air that can be inhaled after a normal inspiration.
Expiratory Reserve Volume (ERV): Additional air that can be exhaled after a normal expiration.
Residual Volume (RV): Air remaining in the lungs after maximal exhalation.
Total Lung Capacity (TLC): Total volume of air the lungs can hold (TV + IRV + ERV + RV).
Vital Capacity (VC): Maximum volume of air that can be exhaled after maximum inhalation (TV + IRV + ERV).
23. What do Dalton’s law and Henry’s law state?
Dalton's Law: The total pressure of a gas mixture is equal to the sum of the partial pressures of its individual gases.
Henry's Law: The amount of gas dissolved in a liquid is proportional to the partial pressure of that gas above the liquid.
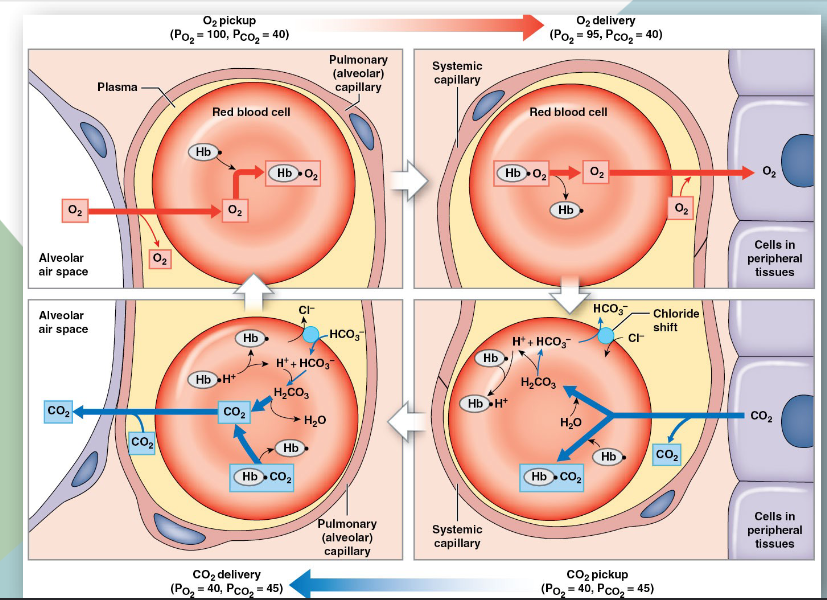
24. What is the difference between external and internal respiration?
External Respiration: Gas exchange that occurs in the alveoli and the capillaries surrounding them, where O2 enters the blood and CO2 leaves.
Internal Respiration: Gas exchange between the blood and peripheral tissues, where O2 is delivered to cells and CO2 is picked up.
In external respiration: alveolar PO2 is higher than capillary PO2, driving O2 into the blood. In internal respiration: capillary PO2 is higher than tissue PO2, driving O2 into tissues and allowing CO2 to diffuse into capillaries, where its pressure is lower.
The pressures of these gases drive the direction of their movement: O2 moves from areas of higher pressure to lower pressure (from alveoli to blood and from blood to tissues) while CO2 moves from blood to alveoli for expiration.
How does pressure of oxygen affect hemoglobin saturation? Is it a linear relationship? Why does this make sense according to what I have discussed in lecture?
Oxygen pressure affects hemoglobin saturation in a non-linear relationship known as the oxygen-hemoglobin dissociation curve. At higher pressures of oxygen, hemoglobin saturation increases significantly, but this increase occurs at a decreasing rate. This relationship makes sense because it allows for efficient loading of O2 in the lungs where pressure is high, while still allowing for O2 unloading at tissues where pressure is lower.
How does pH affect hemoglobin saturation (Bohr effect)? Why does CO2 lead to a lower pH (more acidic)? Know the formula to explain this.
The Bohr effect describes how decreased pH (more acidic conditions) leads to lower hemoglobin saturation with oxygen. CO2 reacts with water in the blood to form carbonic acid (H2CO3), which dissociates into bicarbonate (HCO3−) and hydrogen ions (H+), thus lowering pH:
[
CO2 + H2O \rightleftharpoons H2CO3 \rightleftharpoons HCO3− + H+
]
This increased concentration of H+ ions causes hemoglobin to change shape, reducing its affinity for O2.
How does temperature affect hemoglobin saturation?
Increased temperature leads to decreased hemoglobin saturation with oxygen. Higher temperatures promote the release of O2 from hemoglobin, enhancing oxygen delivery to tissues during periods of increased metabolic activity (like exercise).
What are the 3 ways of transport for CO2? What proportions of CO2 are transported in each way?
Dissolved in plasma: About 7-10% of CO2 is transported in this form.
Bound to hemoglobin as carbamino compounds: Approximately 20-23% of CO2 is transported in this way.
As bicarbonate ions (HCO3−) in plasma: About 70% of CO2 is transported in this form.
Explain the diagram for 'Summary of Gas Transport'.
To explain this diagram, visualize the flow of oxygen and carbon dioxide during external respiration in the lungs and internal respiration at the tissues. In the lungs, oxygen from the alveoli diffuses into pulmonary capillaries (high to low pressure), leading to oxygen loading onto hemoglobin. Meanwhile, the increase of carbon dioxide in the blood (from cells) leads to its diffusion into the alveoli for exhalation. For internal respiration, oxygen from systemic capillaries diffuses into tissues (where partial pressure is lower) and simultaneously, carbon dioxide produced by cellular metabolism diffuses back into the capillaries. This exchange illustrates the driving forces of gas transport based on pressure gradients and the roles of hemoglobin and carbon dioxide. Teaching this to someone would require ensuring they understand both the pressure gradients and the context of metabolism.
In terms of chemoreceptor reflexes, what happens when we have hypercapnia? Hypocapnia?
Hypercapnia: Elevated CO2 levels lead to increased respiratory rate in order to expel more CO2 and restore pH levels.
Hypocapnia: Decreased CO2 levels result in a reduced respiratory rate to retain CO2 and stabilize pH.
What happens in terms of baroreceptor reflexes when BP falls?
When blood pressure falls, baroreceptors send signals to the central nervous system, triggering reflexes to increase heart rate and constrict blood vessels. This helps restore blood pressure to normal levels.
What are the Hering-Breuer reflexes?
The Hering-Breuer reflex is a protective mechanism that prevents over-inflation of the lungs by sending signals to stop inhalation when lung stretch receptors are activated.
What are the 3 different protective reflexes we have with the respiratory system?
Cough Reflex: Clears respiratory passages from foreign irritants.
Sneezing: Similar to the cough reflex, but specifically clears particles from the nasal passages.
Yawning: May help increase oxygen intake and stretch lung tissue.
How does the respiratory system differ in newborns vs. elderlies?
In newborns, the respiratory system is immature, with higher respiratory rates and underdeveloped alveoli, leading to potential breathing difficulty. In elderlies, there’s decreased lung elasticity, reduced respiratory muscle strength, and a higher likelihood of respiratory conditions, contributing to lower overall pulmonary function.
Conditions associated with this chapter (know what these are and causes if applicable):
Laryngitis: Inflammation of the larynx; often due to infection or overuse.
Acute Epiglottitis: Inflammation of the epiglottis, potentially life-threatening; often bacterial.
Bronchitis: Inflammation of the bronchi; often caused by infection or smoking.
Asthma: Chronic inflammation leading to airway narrowing; triggers include allergens, smoke.
Respiratory Distress Syndrome: Difficulty in breathing due to insufficient surfactant in newborns.
Pneumonia: Lung infection leading to inflammation; can be viral or bacterial.
Pleurisy: Inflammation of the pleura; could be due to infections or autoimmune diseases.
Pneumothorax: Accumulation of air in the pleural space, causing lung collapse; often from trauma.
Atelectasis: Collapsed lung; can occur post-surgery or due to blockage.
Hypoxia: Deficiency in oxygen reaching tissues; can be due to respiratory or circulatory issues.
Anoxia: Complete deprivation of oxygen; can lead to death of tissues.
Emphysema: Condition that involves damage to alveoli, leading to reduced gas exchange; often due to smoking.
Apnea, Eupnea, Hyperpnea: Different breathing patterns; apnea (no breathing), eupnea (normal), and hyperpnea (increased rate/depth).