Human Patholgy, Chapter 19: The Breast
The Breast: Comprehensive Notes
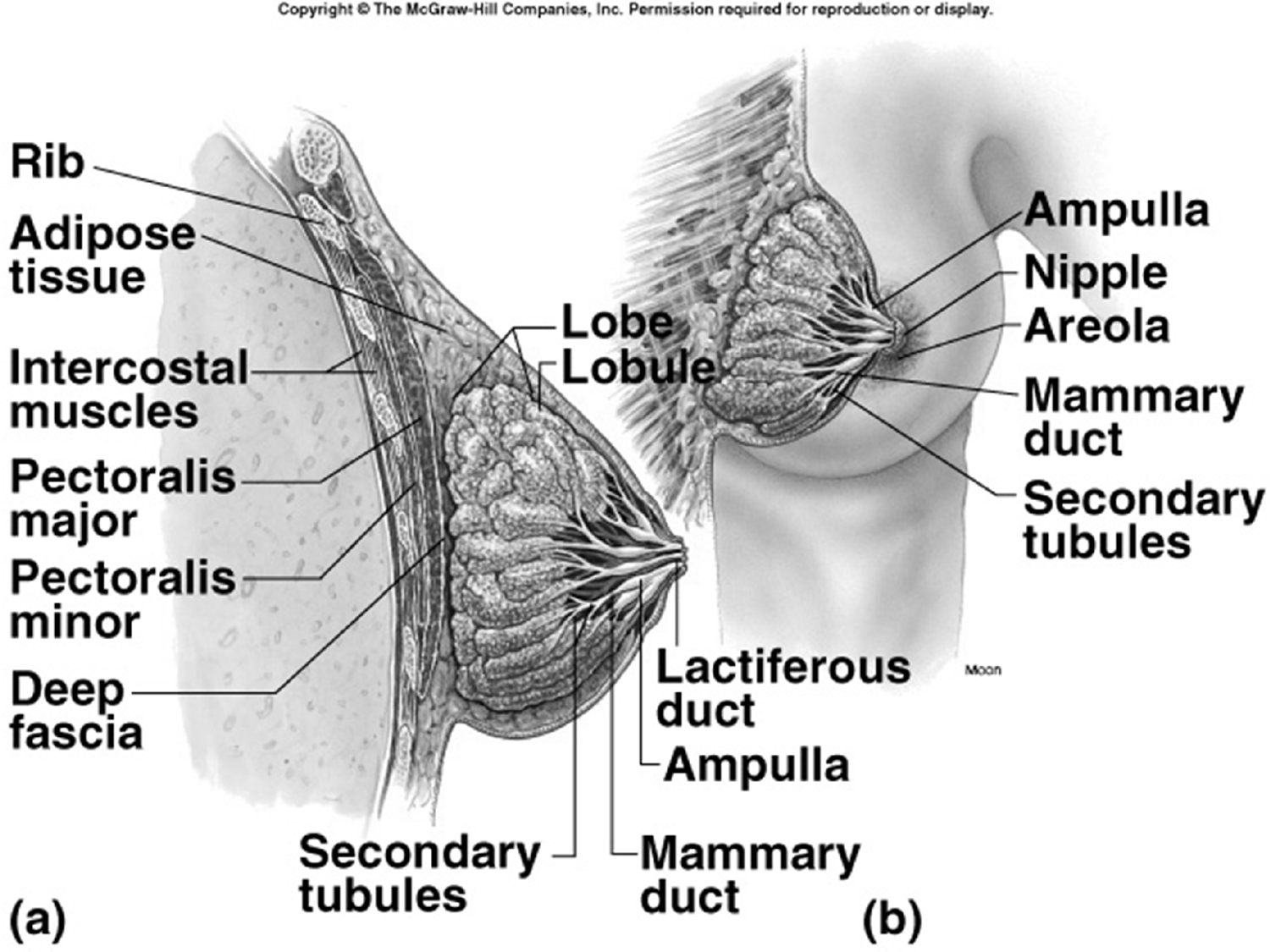
Breast Anatomy
External and Internal Structures:
Rib
Adipose tissue
Intercostal muscles
Pectoralis major
Pectoralis minor
Deep fascia
Lobe
Lobule
Lactiferous duct
Moon (likely a diagram label for "mound" or similar, as depicted)
Secondary tubules
Ampulla
Nipple
Areola
Mammary duct
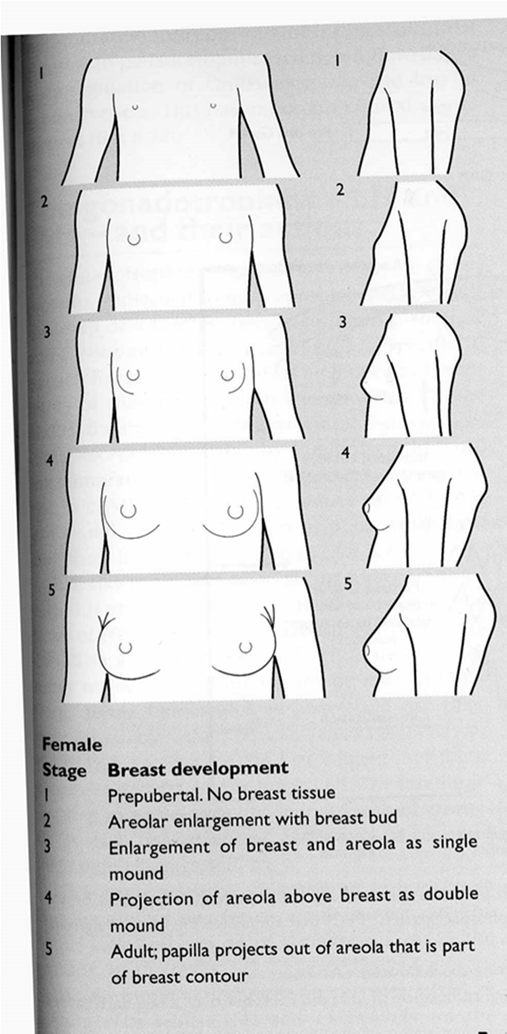
Tanner Stages of Breast Development
These stages are growth development milestones for breast maturation:
Stage 1: Prepubertal. No breast tissue is present.
Stage 2: Areolar enlargement with the development of a breast bud.
Stage 3: Enlargement of both the breast and areola, forming a single mound.
Stage 4: The areola projects above the breast, creating a double mound appearance.
Stage 5: Adult stage; the papilla (nipple) projects out of the areola, which becomes part of the overall breast contour.
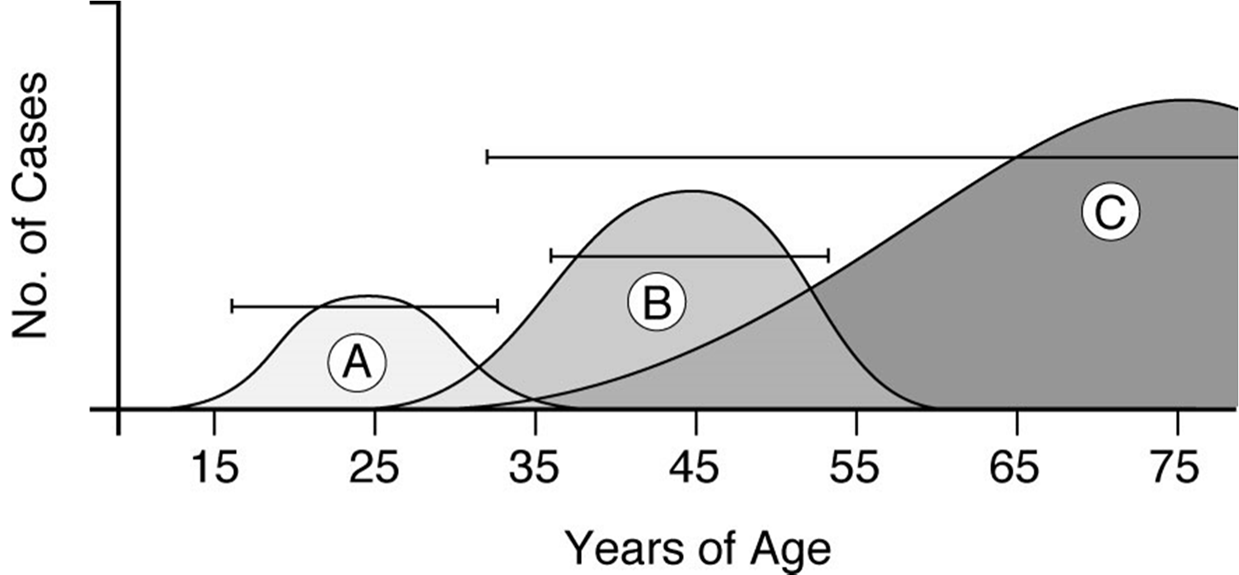
Age-Related Incidence of Breast Diseases
The incidence of various breast diseases varies with age, as depicted in epidemiological curves, showing patterns of increase and decrease across different age groups (e.g., peak incidence for some diseases between approx. 45 and 65 years of age).
Abnormalities in Breast Development
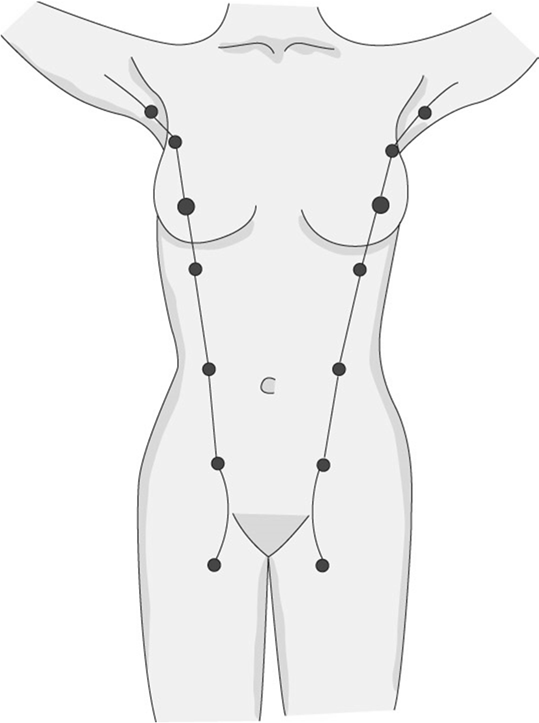
Accessory Breasts and Nipples:
Most commonly found in the armpits or on the lower chest, usually below and medial to the normal breasts.
Unequal Development:
Fully developed breasts are typically similar in size but not perfectly identical.
Sometimes, one breast may fail to develop as much as its counterpart.
Breast Hypertrophy:
Occurs at puberty when one or both breasts over-respond to normal hormonal stimulation.
The hypertrophy is caused by an overgrowth of fibrous tissue, not glandular tissue or fat.
This condition results from the excess production of estrogen and progesterone.
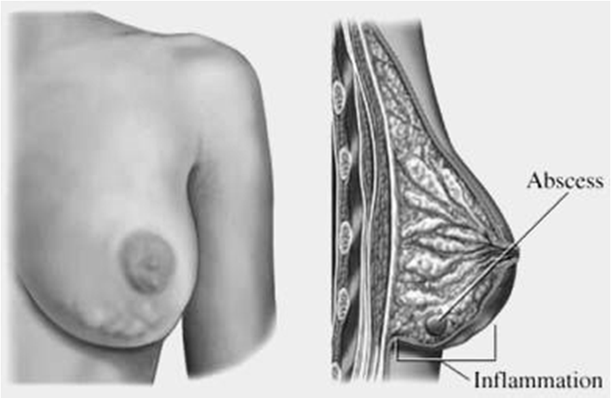
Inflammatory Diseases of the Breast
Acute Mastitis:
Cause: Typically caused by pus-producing bacteria, such as Streptococcus (strep) or Staphylococcus (staph).
Complication: A common complication that arises during lactation.
Symptoms: Usually involves pain and discharge from the breast, which may contain pus or blood.
Treatment: Antibiotics are the primary treatment.
Chronic Mastitis:
Cause: The exact cause is unknown.
Affected Population: Primarily affects premenopausal women.
Symptoms: Produces non-specific symptoms.
Association: Can sometimes stem from secondary tuberculosis (Tuberculous mastitis).
Ductal Ectasia:
Affected Population: Primarily occurs in postmenopausal women.
Pathology: Characterized by the dilation of milk ducts due to inflammation.
Symptoms: Presents as a periareolar mass with a green-brown nipple discharge.
Fat Necrosis:
Pathology: Involves the necrosis (death) of fat tissue within the breast, most commonly due to trauma.
Benign Breast Tumors
Fibroadenoma
Nature: A tumor composed of both fibrous tissue and glands.
Prevalence: It is the most common benign neoplasm of the breast, typically observed in premenopausal women.
Presentation: Appears as a well-circumscribed, mobile, marble-like mass.
Hormonal Sensitivity: It is sensitive to estrogen and progesterone.
Prognosis: Considered benign, with no increased risk of developing carcinoma.
Treatment: Oral Contraceptive Pills (OCP/birth control pills) are a common treatment.
Benign Cystic or Fibrocystic Breast Disease
Commonality: A very common benign condition, also known as fibrocystic change, primarily affecting premenopausal women.
Pathology: Characterized by the proliferation of glandular and fibrous tissue, forming lumps. Cysts often exhibit a distinctive "blue-dome appearance" on gross examination.
Mechanism: Represents an irregular cyclic response of the breasts to hormonal fluctuations during various phases of the menstrual cycle.
Diagnosis: Ultrasound examination is highly valuable for distinguishing between a cystic mass and a solid mass in the breast.
Treatment: Management options include OCP, aspiration of the cyst, or surgical intervention if necessary.
Lesions of the Male Breast
Gynecomastia:
Cause: Results from a temporary imbalance of female and male hormones, specifically an increase in estrogen and a decrease in androgen levels.
Presentation: A distinct nodule of tissue develops under the nipple of the male breast.
Historical Context: Historical figures like King Tutankhamun and his brother Smenkhare are depicted by contemporary artists as having gynecomastia.
More glandular tissue than fat, estrogen increases testosterone decreases. can occur from steroid use. anabolic steroid creates estrogen as a byproduct.
Breast Cancer in Males:
Rarity: Breast cancer is rare in males, accounting for only about 1\% of all breast cancer cases.
Presentation: Typically presents as a subareolar mass in older males.
Location: The highest density of breast tissue in males is located directly underneath the nipple.
Symptoms: May produce nipple discharge.
Associated Conditions: Associated with BRCA2 mutations and Klinefelter syndrome (a genetic disorder).
Carcinoma of the Breast—Basic Facts
Prevalence: This is the most common malignant tumor in women.
Lifetime Risk: Approximately 1 in 9 women will be diagnosed with breast cancer during their lifespan.
United States Statistics:
Around 210,000 new cases are diagnosed annually.
Approximately 40,000 individuals die from this cancer each year.
Risk Factors of Carcinoma of the Breast
Sex: Females have a significantly higher risk than males, whose breasts are not subject to ovarian hormone stimulation.
Early Menarche: An earlier age for the first menstrual period (menarche) is a risk factor.
Genetic Factors: A strong family history and mutations in genes such as BRCA-1, BRCA-2, and BRCA-3 (as listed on the slide) are significant risk factors.
Race: White women have a higher incidence compared to African and East Asian women.
Age: The tumor is rare before puberty, with risk increasing with age.
Hormones:
Exogenous Estrogen: Exposure to external estrogen sources (e.g., certain hormone therapies) can increase risk.
DHEAS (Dehydroepiandrosterone): This steroid prohormone, present in high quantities in the Western diet, has been linked to an increased risk of breast cancer.
Physical Characteristics:
Obesity: May play a role in breast cancer development.
Body Shape: "Apple-shaped" females (with central obesity) have a higher chance of developing breast cancer than "pear-shaped" women.
Different Types of Breast Cancer
Ductal Carcinoma in situ (DCIS)
Origin: Begins in the cells lining of the milk ducts, which are responsible for supplying milk to the nipple.
Prevalence: Accounts for more than 3/4 of breast cancers and 20-30\% of all breast cancer diagnoses.
Spread: By definition, "in situ" means it has not spread or moved from its original location within the duct.
Invasive Ductal Carcinoma (IDC)
Origin: Starts in the milk ducts but breaks through the duct wall, invading the surrounding breast tissue.
Spread: Can metastasize and spread to other parts of the body.
Prevalence: Accounts for 65 to 80\% of all breast cancers.
Subtypes:
Tubular carcinoma: Characterized by well-differentiated tubules; generally has a good prognosis.
Mucinous carcinoma: Characterized by the presence of extracellular mucin.
Medullary carcinoma: Distinguished by large, high-grade cells growing in sheets, often associated with lymphocytes and plasma cells. It is linked to BRCA-1 mutations.
Inflammatory carcinoma: Characterized by carcinoma (cancer cells) found within the dermal lymphatics. This type has a poor prognosis.
Lobular Carcinoma in situ (LCIS)
Origin: Begins in the milk-secreting glands (lobules) of the breast.
Occurrence: Frequently occurs in multiple areas within one or both breasts.
Invasive Lobular Carcinoma (ILC)
Origin: Starts in the milk-producing glands of the breast but invades surrounding breast tissue and spreads to other parts of the body.
Occurrence: More likely than other types of breast cancer to occur in both breasts.
Metastasis: Tends to metastasize quickly.
Prevalence: Accounts for 10 to 15\% of breast cancers.
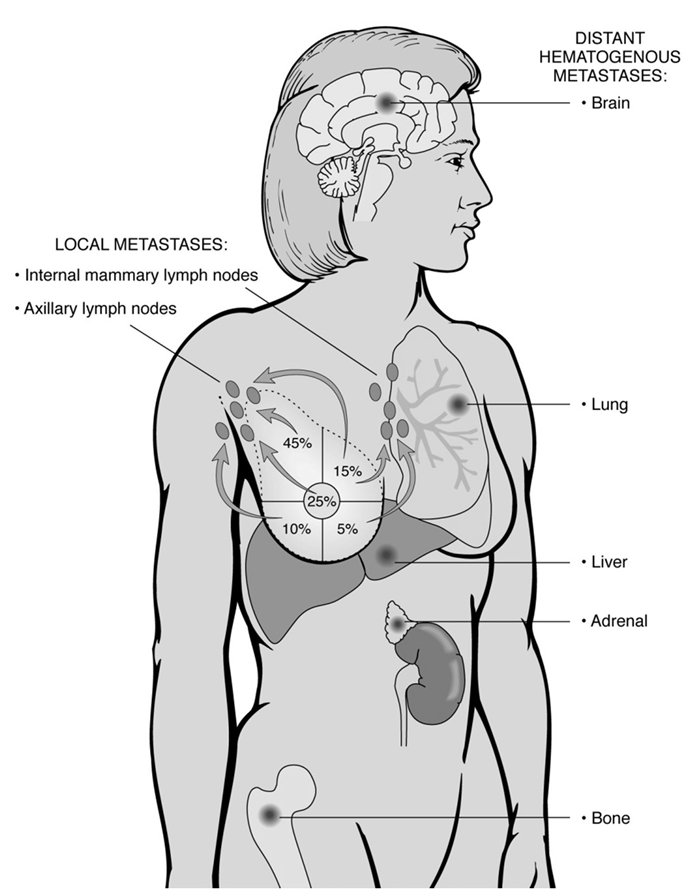
Metastases of Breast Carcinoma
Breast carcinoma can spread through both local and distant pathways:
Local Metastases:
Internal mammary lymph nodes
Axillary lymph nodes
Distant Hematogenous Metastases:
Bone: Approximately 20\% of distant metastases.
Lung: Approximately 10\% of distant metastases.
Adrenal: Approximately 10\% of distant metastases.
Brain: Approximately 5\% of distant metastases.
Liver: Approximately 5\% of distant metastases.
Hereditary Breast Cancer
Prevalence: Represents about 10\% of all breast cancer cases.
Clinical Features Suggesting Heredity:
Multiple first-degree relatives diagnosed with breast cancer.
Tumor onset at an early age (premenopausal).
The presence of multiple tumors in a single patient.
Genetic Mutations: The most critical single gene mutations associated with hereditary breast cancer are BRCA1, BRCA2, and BRCA3 (as mentioned in the transcript).
Prophylactic Surgery: Women identified with a genetic predisposition to developing breast cancer may opt for bilateral mastectomy (removal of both breasts) to significantly reduce their cancer risk.
Persistent Risk: Even after mastectomy, a residual risk of cancer may remain due to the potential extension of breast tissue into the subcutaneous tissue of the chest wall.
Notable Cases: Examples include Angelina Jolie, who underwent bilateral mastectomy and oophorectomy due to BRCA1 mutation, and René Syler, discussed in the transcript, who chose prophylactic mastectomy due to a strong family history and abnormal cell growth, despite testing negative for the BRCA gene.
Paget's Disease of the Breast
Nature: This is an invasive breast cancer that originates in the ducts of the breast and subsequently spreads to the skin of the nipple and areola area.
Prognosis: The prognosis is often poor due to frequent misdiagnosis, as the disorder can initially resemble benign skin conditions like eczema near the nipple area.
Stages of Breast Cancer (For Information Only - Not for Exam)
Stage 0: Cancer cells remain entirely within the breast duct, with no invasion into normal adjacent breast tissue.
Stage I: The cancer is 2 centimeters or less in size and is confined solely to the breast. There is no evidence of spread to lymph nodes.
Stage IIA:
No tumor can be found in the breast, but cancer cells are present in the axillary lymph nodes (lymph nodes under the arm), OR
The tumor measures 2 centimeters or smaller and has spread to the axillary lymph nodes, OR
The tumor is larger than 2 centimeters but no larger than 5 centimeters and has not spread to the axillary lymph nodes.
Stage IIB:
The tumor is larger than 2 centimeters but no larger than 5 centimeters and has spread to the axillary lymph nodes, OR
The tumor is larger than 5 centimeters but has not spread to the axillary lymph nodes.
Stage IIIA:
No tumor is found in the breast, but cancer is found in axillary lymph nodes that are sticking together or to other structures, or cancer may be found in lymph nodes near the breastbone, OR
The tumor is any size, and cancer has spread to the axillary lymph nodes (which are sticking together or to other structures), or cancer may be found in lymph nodes near the breastbone.
Stage IIIB:
The tumor may be any size and has spread to the chest wall and/or skin of the breast AND may have spread to axillary lymph nodes that are clumped together or sticking to other structures, or cancer may have spread to lymph nodes near the breastbone.
Inflammatory breast cancer is always considered at least Stage IIIB.
Stage IIIC:
There may be either no sign of cancer in the breast or a tumor of any size, which may have spread to the chest wall and/or the skin of the breast, AND
The cancer has spread to lymph nodes either above or below the collarbone, AND
The cancer may have spread to axillary lymph nodes or to lymph nodes near the breastbone.
Stage IV: The cancer has spread (metastasized) to other distant parts of the body.
Breast Sarcoma
Rarity: Breast sarcoma is rare when compared to breast carcinoma.
Origin: Arises from the fibrous tissue or blood vessels within the breast.
Characteristics: Typically presents as a large, bulky tumor.
Metastasis: Has the potential to metastasize widely.
Treatment: The primary treatment involves surgical resection of the involved breast.
Clinical Manifestations of Breast Carcinoma
Lump in the breast: Often the first noticeable sign.
Nipple or skin retraction: The nipple or overlying skin may pull inward.
Skin edema ("orange peel sign"): Swelling of the skin, leading to a pitted appearance resembling an orange peel.
Tumor infiltration and fixation: The tumor infiltrates breast tissue and can become fixed to the underlying chest wall.
Metastasis: Spread of cancer cells to other parts of the body.
Breast Examination and Diagnostic Modalities
Clinical Examination
Methodology: Involves both inspection and palpation of the breast.
Axillary Tissues: Examination includes the axillary (underarm) tissues.
Positions: Examination is performed with arms at the sides, then elevated and lowered, and finally with hands on hips to observe any changes or retractions.
Palpation Technique: Commences at the periphery of the breast, with all parts palpated systematically, often in a clockwise direction, concluding with examination of the tissues directly under the nipples.
Mammogram
Purpose: Primarily used to identify lesions that may not be detectable during a clinical examination.
Recommendations:
A baseline mammogram is recommended at ages 35-40.
Followed by annual or biannual screenings up to age 50.
Then, annually thereafter.
Utility in Different Age Groups:
Postmenopausal Women: Most useful because their breasts contain more fat and less glandular tissue, allowing a dense tumor to contrast sharply with the less-dense fatty tissue.
Younger Women: Less useful as their breasts appear much denser due to a higher proportion of glandular and fibrous tissue, which can obscure lesions.
Potential Problems with Radiographic Readings:
Breast size (and compression during the procedure).
Breast density.
Patient motion during imaging.
Presence of deodorants, talcum powder, or lotions.
Technician variability and skill.
Breast Self-Examination (BSE)
Involves systematic palpation and inspection of one's own breasts to detect any changes or lumps.
Magnetic Resonance Imaging (MRI)
Efficacy: Highly helpful in defining the full extent of the disease versus clinically occult (hidden) breast cancer.
Implant Assessment: Useful for assessing the integrity of breast implants and detecting ruptures.
High-Risk Screening: Valuable for screening high-risk individuals, especially those with tumor suppressor gene deletions like BRCA1 and BRCA2.
Other Modalities
Ultrasound: Utilized for breast imaging, particularly helpful in distinguishing cystic from solid masses.
Biopsy
Fine-needle aspiration: A minimally invasive procedure to collect cell samples.
Incisional biopsy: Surgical removal of a portion of a suspicious mass for pathological examination.
Sentinel lymph node biopsy: Involves identifying and removing the first lymph node(s) to which cancer cells are most likely to spread from the primary tumor, observing that valves allow fluid to flow in one direction only towards these nodes.
Treatment of Breast Carcinoma: Surgery
Both surgical methods aim to achieve similar long-term outcomes:
Modified Radical Mastectomy (Total Mastectomy with Axillary Lymph Node Dissection):
Involves resecting (removing) the entire breast along with the axillary (underarm) tissue.
The pectoral muscles overlying the chest wall are preserved.
Partial Mastectomy / Lumpectomy with Lymph Node Dissection and Radiotherapy:
This approach involves removing only a part of the breast containing the tumor, or just the tumor itself with a small amount of adjacent healthy breast tissue.
It is typically followed by radiotherapy (radiation therapy) to the remaining breast tissue.
Prognosis and Systemic Treatment of Breast Carcinoma
Prognosis Factors
TNM Staging: Prognosis in breast cancer is primarily based on the TNM (Tumor, Node, Metastasis) staging system.
Metastasis: The presence of distant metastasis is the most critical prognostic factor, though most patients are diagnosed before metastasis occurs.
Lymph Node Involvement: Spread to the axillary lymph nodes is the most useful prognostic factor in cases where distant metastasis is not yet evident at presentation.
Receptor Status and Gene Amplification: The most important biological factors for prognosis and treatment guidance are:
Estrogen Receptor (ER) status
Progesterone Receptor (PR) status
HER2/neu gene amplification (overexpression) status
Treatment Modalities Based on Receptor Status
Hormone Receptor-Positive Cancers (ER/PR-positive):
The presence of ER and PR is associated with a favorable response to anti-estrogenic agents.
Mechanism: Estrogen binds to specialized receptors within the cancer cell's nucleus, signaling the tumor to grow and divide.
Anti-estrogenic Agents:
Selective Estrogen Receptor Modulators (SERMs): Such as Tamoxifen and Raloxifene (e.g., EVISTA, which also treats osteoporosis by acting like estrogen in bones and blocking it in breasts).
Estrogen Receptor Downregulators: Such as Fulvestrant (ICI/Faslodex).
Anti-progesterone agents: Such as RU486.
Aromatase Inhibitors: New drugs (e.g., Ibrance) that stop the conversion of androgens to estrogen, thereby reducing estrogen levels available to fuel cancer growth. Ibrance is a CDK 4/6 inhibitor that works inside the nucleus to inhibit CDK 4 and CDK 6 (cyclin-dependent kinases 4 and 6), thereby stopping cell growth and division. It is typically given daily for 3 weeks on, 1 week off, combined with an aromatase inhibitor, which is taken daily for all 4 weeks.
Cost of Ibrance: Approximately $10,242 per month or $124,110 per year per patient.
HER2/neu-Positive Cancers:
Mechanism: Cells have HER2/neu receptors that help them grow. Breast cancer cells with too many HER2/neu receptors tend to be very fast-growing due to overactive growth signals.
Targeted Therapy: HER2/neu amplification is associated with a positive response to Herceptin (trastuzumab).
Herceptin (Trastuzumab): A designer antibody directed against the HER2 receptor, a growth factor receptor present on the cell surface. It attaches to HER2 receptors and may stop them from signaling the cell to grow.
First dose infusion time: 90 minutes. Subsequent doses: 30 minutes (when taking weekly).
Treatment may stop if severe allergic reaction, swelling, or lung problems occur.
Enhertu: A newer HER2-directed antibody and topoisomerase inhibitor conjugate.
Indication: For adult patients with unresectable or metastatic HER2-positive breast cancer who have received 2 or more prior anti-HER2-based regimens in the metastatic setting.
Administration: Administered via intravenous (IV) infusion once every 3 weeks (21-day cycle) until disease progression or unacceptable toxicity.
Cost: Wholesale acquisition cost of $2,295.97 for a 100mg vial (launched January 2020).
"Triple-Negative" Tumors:
Characteristics: These tumors test negative for Estrogen Receptor (ER), Progesterone Receptor (PR), and HER2/neu amplification.
Prognosis: They generally have a poor prognosis.
Demographic: African American women have an increased propensity to develop triple-negative carcinoma.
PARP Inhibitors for BRCA1/2 Mutation Patients:
Lynparza (Olaparib): An inhibitor of poly (ADP-ribose) polymerase (PARP) enzymes (PARP1, PARP2, and PARP3).
Mechanism: PARP enzymes are involved in normal cellular functions, including DNA transcription and DNA repair. By blocking these enzymes, DNA damage in cancer cells (especially those with BRCA1/2 mutations, which already have impaired DNA repair pathways) is less likely to be fixed, leading to cancer cell death and potentially slowing or halting tumor growth.