Behavioral Neuroscience - Neuropharmacology
- Neuropharmacology
- the study of how substances affect our nervous system and behavior
- one of the main areas of neuroscience research today
- usually starts with animal research, once safety is established moves to human clinical studies
- often (but not always) involves comparing active substances to a placebo (saline solution)
- may use “active” placebo and may use double-blind research design
- Basic terms
- Agonist --- increases NT activity
- Antagonist --- decreases NT activity
- Placebo --- an inert substance that is given to an organism instead of a physiologically active drug; used experimentally to control for the effects of mere administration of a drug
- sometimes creates same effect as the drug
Research terms
- Half-life --- time it takes 1/2 of the drug to leave the body
- used as a safety and maintenance factor
- must examine drug “metabolites” as well as active ingredients
- Drug metabolism: the process by which the body breaks down and converts medication into altered chemical substances
- can be active or inactive
- may not cause desired effect but affect other things; active = produce effect, inactive don’t
- Elimination of a drug characterized by more than one half-lif every time half is eliminated = half-life
- Time required for a drug concentration to reach steady state is determined by half-life
- in most clinical situations, the attainment of steady state can be assumed after 3-5 half-lives
- When the drug concentration is around 5% it is said to be negligible, therefore around 4 or 5 half-lives must elapse until the drug is eliminated
- Time for drug “negligibility” = half-live * 5
- Dose-response curve
- a graph of the relationship between drug doses and the effects
- attempts to find effective and safe dose of drug
- can be used to plot the results of many kinds of experiments; X-axis usually drug/hormone concentration, Y-axis plots response (can be almost anything) \n
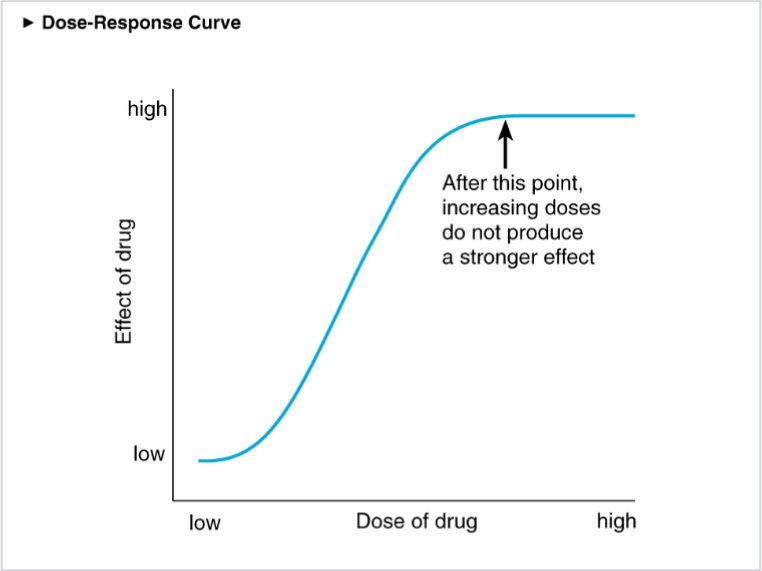
- the specific measurement (DV) will be defined b/c pharmacological agents can have multiple effects
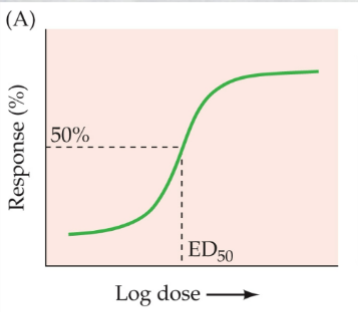
- plots increasing drug dose (usually on a logarithmic scale) against increasing strength of the response being studied
- the dose at which the drug shows half of its maximal effect is termed the effective dose 50% (ED50)
- Therapeutic window--- many drugs only work at specific doses; high and low often have little effect
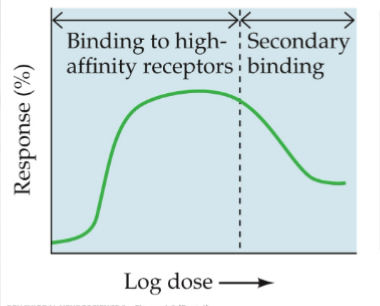
- Nonmonotonic DRC --- a DRC that is normal up to a point but then reverses and the measured response begins to decrease with larger doses
- Dose-response functions
- Minimum effective dose (ED50) --- lowest dose to produce desired effect in 50 % of clinical subjects
- Median Toxic dose (TD50) --- dose which produces the first signs of toxicity in 50% population
- high build-up in blood
- Threshold dose --- smallest dose to produce detectable change
- change must be defined by therapeutic effect
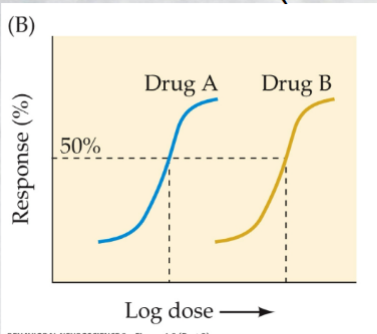
- We can assess the relative potency of two drugs by comparing their ED50 values
- Maximum response (max dose) --- the greatest degree of response that can be achieved with a specific drug
- usually there is a plateau effect past which further dose do not increase effect
- sometimes higher doses decrease effect (like amphetamines) because other effects begin to interfere with desired effect
- We can compare drug efficacies by evaluating maximal responses, rather than doses
- Partial agonist/antagonist - a drug of only moderate efficacy
- Therapeutic index (TI) --- the separation between the effective dose and a toxic one
- Safe index - ratio between TD50/ED50
- TI = 100x safe (over-the-counter), TI =10x hazardous
- becomes an issue with uncontrolled recreational use---tolerance to recreational effect occurs very quickly
- Clinical efficacy---refers to the degree to which a drug is able to induce a given effect
- related to maximal response
- DRC can allow the comparison of difference drugs
- Potency-- the amount of a drug needed to produce a desired effect
- lower the needed dose, more potent
Drug interactions
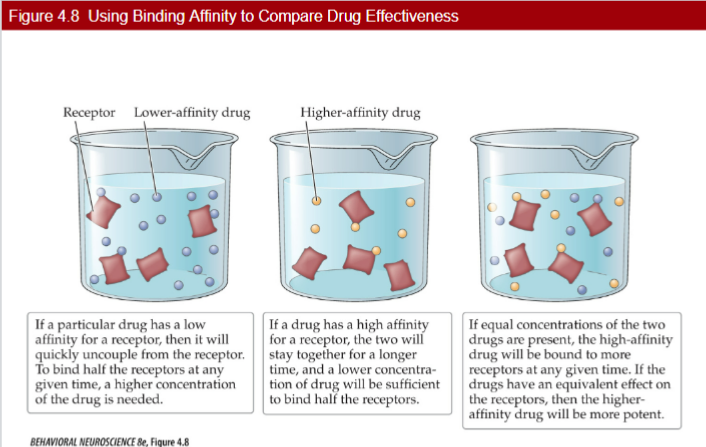
- Affinity - capacity of a compound (drug) to maintain contact or be bound to a receptor
- binding affinity = the degree of chemical attraction between a ligand and a receptor
- a drug with a high affinity for its receptor will be effective at very low doses
- when two substances are being taken, one with the most affinity will have greater effect
- penicillin and alcohol
Tolerance/Dependency
- Tolerance - when there’s a decreased susceptibility or increase in amount of drug being taken needed
- represented by a rightward shift in the dose response curve
- has a physiological and psychological component
- Factors
- Metabolic tolerance --- organ systems become more effective at eliminating the drug
- Elevation in Hepatic Microsomal Enzyme (HME) - reduces drug to metabolites so they become ineffective and easier to eliminate
- ‘hepatic’ = liver
- creates inactive and easier-to-eliminate metabolites
- with repeated use of the brain creates more HMEs
- associated with cross-tolerance to related substances
- tolerance to once drug gives pre-existing tolerance to another (ex. surgical, analgesics, and narcotics)
- creates dangerous interactions between drugs that share the same HMEs---sedatives and alcohol
- biotransformation produces active metabolites that may produce side effects
- Functional tolerance: target tissue may show altered sensitivity to the drug
- up and down-regulation of receptors
- with repeated drug use nervous sys can respond by altering the density of post-synaptic receptors
- increase density = up-regulation, antagonist
- lower density= down regulation; agonist
- Drug dependent
- Physical dependency: when