health assessment midterm study
Chapter 2: ROS COLDSPA & PQRST
ROS (Review of Systems)
A thorough and systematic approach to gathering patient information across multiple body systems. This involves asking targeted questions to assess the functional status of each system, including but not limited to:
Cardiovascular System
Subjective Data: Patient may report chest pain, palpitations, fatigue, shortness of breath.
Objective Data: Blood pressure, heart rate, ECG findings, and auscultation of heart sounds.
Clinical Tips: Monitor for signs of heart failure; evaluate risk factors for cardiovascular disease.
Respiratory System
Subjective Data: Patients may describe cough, wheezing, chest tightness, difficulty breathing.
Objective Data: Respiratory rate, oxygen saturation, lung auscultation, and potential imaging results.
Clinical Tips: Be aware of patient history with asthma or COPD; assess for signs of hypoxemia.
Gastrointestinal System
Subjective Data: Inquire about appetite changes, nausea, vomiting, abdominal pain.
Objective Data: Abdominal exam findings, bowel sounds, imaging studies like ultrasound or CT scan.
Clinical Tips: Follow up on any changes in bowel habits; consider dietary assessments for nutritional status.
Neurological System
Subjective Data: Ask about headaches, dizziness, memory loss, or changes in mood.
Objective Data: Neurological exam results, GCS (Glasgow Coma Scale) scores, imaging like MRI or CT.
Clinical Tips: Assess for signs of stroke or seizure activity; probe into family history of neurological diseases.
Musculoskeletal System
Subjective Data: Patients may report joint pain, stiffness, or difficulty with mobility.
Objective Data: Range of motion testing, strength assessments, visual inspections for swelling.
Clinical Tips: Check for signs of inflammation; use scales for joint pain severity assessment.
Integumentary System
Subjective Data: Questions regarding skin changes, itching, rashes, or lesions.
Objective Data: Skin inspection notes, description of lesions, temperature, and moisture levels.
Clinical Tips: Regular skin assessments to identify changes that could indicate malignancy; educate on skin protection.
Endocrine System
Subjective Data: Inquire about weight changes, fatigue, heat or cold intolerance, and skin changes.
Objective Data: Blood glucose levels, hormone level assessments, and vital signs.
Clinical Tips: Monitor for signs of hypo- or hyperglycemia; assess for symptoms related to thyroid abnormalities.
Urinary System
Subjective Data: Ask about urination frequency, pain during urination, or changes in urine appearance.
Objective Data: Urinalysis results, abdominal ultrasound for kidneys, and bladder assessments.
Clinical Tips: Be aware of urinary tract infection symptoms and risk factors; assess hydration status.
Reproductive System
Subjective Data: Gather information about menstrual cycles, sexual health issues, or changes in libido.
Objective Data: Pelvic exams, lab tests for hormone levels, imaging if needed (like ultrasound).
Clinical Tips: Discuss contraception options and sexual health openly; educate on STIs.
COLDSPA
An acronym designed to facilitate a comprehensive assessment of pain:
Character: Describe the pain. Is it sharp, dull, throbbing, burning, etc.?
Onset: Document when the pain started. Was it sudden or gradual?
Location: Specify the exact site of the pain and any radiation.
Duration: How long does the pain last? Is it constant, intermittent, or variable?
Severity: Assess the pain intensity on a scale (e.g., 0-10), providing a better understanding of its impact.
Pattern: Identify what factors make the pain better or worse — activities, medications, or changes in position.
Associated factors: Gather information about other symptoms that occur concurrently (nausea, dizziness, etc.), which may be significant for diagnosis.
PQRST
Another structured approach for pain assessment that further categorizes the characteristics of pain:
Provocation/Palliation: Determine what initiates the pain and what actions or treatments alleviate it (e.g., rest, ice, heat, medications).
Quality: Essential in describing the pain (e.g., sharp, cramping, aching).
Region/Radiation: Where is the pain localized? Does it radiate to other areas (e.g., down an arm, into the back)?
Severity: Similar to COLDSPA, assess how intense the pain is.
Time: Look at the timing of pain episodes including onset, duration, and frequency, allowing insights into potential chronic issues.
Chapter 3: Physical Examination Techniques
Inspection: Systematic observation of the patient to identify any visible abnormalities or changes.
only expose the part of body being examined
look for symmetry, appearance of skin, size, location, odors
Palpation: Using hands to feel the body structures, noting any tenderness, masses, or abnormalities.
Feel for:
texture (rough/smooth)
temperature (warm/cold)
moisture (wet/dry)
mobility (fixed/mobile)
consistency (soft/hard/fluid filled)
strength of pulse
size/shape
degree of tenderness
Types of Palpation
Light palpation: Gently move one hand in circles on the skin’s surface, pressing less than 1 cm deep. Used to check things like pulse, temperature, and moisture.
Moderate palpation: Press slightly deeper (1–2 cm) with one hand in circular motions to feel organs or lumps.
Deep palpation: Use both hands, with one on top of the other, pressing 2.5–5 cm deep to feel deep organs.
Bimanual palpation: Use both hands on opposite sides of the body—one hand presses while the other feels the organ or structure.
Percussion: A technique of tapping on a surface to assess the consistency and underlying structures, aiding in identifying fluid build-up or organ enlargement.
can determine pain, location, size & shape of organ, density (how much mass [heavy/light]), detect abnormal masses, view reflexes
Direct: Tap a body part directly with one or two fingers to check for pain or tenderness.
Blunt: Place one hand flat on the body and use a fist to tap the back of that hand to check for organ pain.
Indirect: Place one finger on the body and use the other hand’s finger to tap it, helping to detect sounds from deeper inside the body.
Auscultation: Listening to sounds produced within the body using a stethoscope, vital for assessing heart, lung, and bowel functions.
diaphragm - listens to high pitched sounds (hold firmly against body)
bell - listens to low pitched sounds (hold lightly against body)
Chapter 4: Clinical Judgment Model (SBAR)
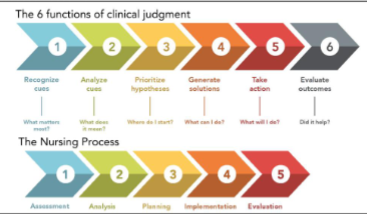
SBAR: A Standardized Communication Framework
An effective tool for ensuring clarity during clinical interactions:
Situation: Provide a clear and concise statement of the current issue.
Background: Give context, including relevant medical history and previous interventions.
Assessment: Offer a professional evaluation of the situation and any interpretation of findings. (what subjective & objective data was found)
Recommendation: Suggest what should be done for the client
Chapter 6: GCS Scoring
GCS (Glasgow Coma Scale)
A standardized tool to assess a patient’s level of consciousness based on three categories:
Eye opening response: Various responses ranging from spontaneous to non-responsive.
4 points for spontaneous eye opening
-3 points for eyes open to speech
-2 eyes open to painful stimuli
-1 point for no eye opening
Verbal response: Evaluation from oriented speech to incoherent or absent verbal responses.
5 points for oriented
-4 points for confused but coherent
-3 points for inappropriate words or jumbled words
-2 points for incomprehensible sounds
-1 point for no verbal response
Motor response: Range from purposeful movement to unresponsive states. This scale provides critical insight into a patient's neurological status.
6 points obeying commands fully
-5 points for localized pain (purposeful moments towards where the pain stimulus is occurring
-4 points for withdrawing from pain
-3 points for abnormal flexion or decorticate posturing
-2 points for abnormal extension or decerebrate posturing
-1 point for no response
maximum score = 15
comatose score = 7
EVM = 4,5,6
alcohol affects GCS score
Dementia vs. Delirium
Dementia: loss of brain function. Refers to a chronic, progressive cognitive decline typically due to degeneration (e.g., Alzheimer's), affecting memory, thinking, and social abilities.
Delirium: An acute, fluctuating change in mental status, often due to underlying medical conditions, medications, or environmental factors. Recognizing these differences is vital for appropriate management.
Chapter 8: Vital Signs
Normal Levels
Defines the standard ranges for vital signs crucial for assessing overall health:
Pulse: Normal range is 60-100 bpm, with variations significant for age and health status.
tachycardia is greater than 100bpm
bradycardia is lower than 60 bpm
Respiration: Normal range is 12-20 breaths per minute, reflecting metabolic and respiratory health.
observe: rate, rhythm, depth
Blood Pressure: Maintains an ideal reading of 120/80 mmHg, as deviations indicate possible cardiovascular issues.
drop of 20 mmHg difference from sitting and standing is normal
elevated blood pressure = 120-129 systolic & 80 (or less) diastolic
hypertension
stage 1 - systolic 130-139; diastolic 80-89
stage 2 - systolic 140 or more; diastolic 90 or more
hypertensive crisis - systolic over 180 and/or diastolic over 120
ORTHOSTATIC hypotension - SUDDEN drop of 20mmHg systolic or diastolic within 3 minutes of lying/sitting down to standing
Temperature: Normal body temperature ranges from 96°F to 99°F (36.5 -37.7 C), with critical implications for infection or systemic conditions.
hypothermia less than 36.5C or 96F
hyperthermia more than 38C or 100.4F
temp can be taken from: oral, temporal, tympanic, axillary, rectal
Chapter 9: Pain Classification
Psychological Pain: Pain linked to emotional issues.
Psychosomatic Pain: Pain affected by mental state, with no clear physical cause.
Nociceptive Pain: Pain from tissue damage or injury.
Neuropathic Pain: Pain caused by nerve damage, often described as burning or tingling.
Inflammatory Pain: Pain due to swelling and inflammation, like in arthritis.
Somatic Pain: Sharp pain from muscles or body tissues, easy to locate.
Visceral Pain: Diffuse pain from internal organs, hard to pinpoint.
Radicular Pain: Pain that radiates from a nerve root, like sciatica.
Phantom Pain: Pain in a limb that has been amputated, as if the limb is still there.
Cancer Pain: Pain from cancer or its treatments.
Referred Pain: Pain felt in a different place from where it actually comes from.
Subjective Data
Understanding a patient's unique experience and interpretation of symptoms enables a tailored approach to pain management. The PQRST framework is pivotal in effectively gathering pain-related information.
Chapter 13: Food Allergies
Severe/Anaphylactic Responses
Critical symptoms could indicate serious allergic reactions requiring immediate medical intervention: difficulty breathing, swelling, hives, or gastrointestinal distress.
Objective Data Indicators
Such as BMI and Waist-Hip Ratio (Waist-Hip Ratio (WHR) measures body fat distribution by dividing the waist circumference by the hip circumference. A higher ratio indicates higher health risks, such as heart disease. Normal values are below 0.90 for men and 0.85 for women.) are vital metrics for evaluating nutritional status and identifying potential health risks.
underweight = less than 18.5 BMI
normal = 18.5 - 24.9 BMI
overweight = 25 - 29.9 BMI
obese = 30+ BMI
Nutritional Deficiency Signs
Common symptoms include dry eyes, sore throat, and mouth ulcers, indicating a need for dietary assessment to improve health outcomes.
Nutritional disorders on general body:
Weight loss, weakness, fatigue
Can be from anemia, electrolyte imbalance, lack of nutrients
Nutritional disorders on skin, hair, nails:
Dry skin, ecchymosis, dry thinning hair, brittle nails
Can be from Vitamin A,B,C,K,Zinc deficiency, dehydration, lineolic acid deficiency
Nutritional disorders on eyes:
Night blindness, red conjunctiva
Can be from vitamin A deficiency, riboflavin deficiency
Nutritional disorders of throat & mouth:
Cracks @ corner of mouth, magenta tongue, beefy red tongue, soft sponges bleeding gums, swollen neck (goiter)
Can be from riboflavin/niancin, B12, C, iodine deficiency
Nutritional disorders on cardiovascular:
Edema, tachycardia, hypotension
Can be from protein deficiency, fluid volume deficit
Nutritional disorders on gastrointestinal:
Ascites (excess abdominal fluid)
Can be from protein deficiency
Nutritional disorders on musculoskeletal:
Bone pain & bow leg, muscle wasting
Can be from vitamin D, calcium, protein, fat, carbohydrates deficiency
Nutritional disorders on neurologic:
Altered mental status, paresthesia (tingling sensation)
Can be from dehydration, B12, thiamine, pyridoxine deficiency
Chapter 14: Skin Lesions
Primary & Secondary Skin Lesions
Skin Lesions: Primary Lesions:
• Macule—a flat, well-circumcised lesion up to 1 cm in diameter
• Papule—a raised bump up to 1 cm in diameter
• Nodule—an elevated, firm, circumscribed, and palpable area
greater than 5 mm in diameter
• Cyst—an elevated, circumscribed area filled with liquid or semisolid
fluid
• Plaque—an elevated, flat-topped, firm, rough, superficial papule
greater than 1 cm in diameter
• Wheal—an elevated, irregularly shaped area of cutaneous edema;
wheals are solid, transient, and changeable, with a variable
diameter; can be red, pale pink, or white.
• Vesicle—a clear, fluid-filled blister up to 1 cm in diameter
• Bulla—a vesicle greater than 1 cm in diameter
• Pustule—an elevated, pus-filled lesion up to 1 cm in diameter
Skin Lesions: Secondary Lesions
Scale: Flaky skin made up of dead cells
flakey exfoliation
irregular, thick/thin, dry/oily, can be white or tan
Crust: Raised area with dried fluid or pus.
Fissure: A deep crack in the skin.
Ulcer: Open sore that damages deeper skin layers.
Scar: Permanent mark on the skin from healing.
Atrophy: shrinking of skin in one area
Excoriation: Scratches on the skin surface.
Lichenification: Thick, rough skin from constant rubbing/scratching (ex: eczema)
Skin Cancer Education
Emphasizes the importance of regular self-examination using the ABCDE method:
Asymmetry: Uneven shape of lesions.
Border irregularity: Unclear or jagged edges.
Color variation: Multiple colors within a lesion.
Diameter: Greater than 6 mm may indicate malignancy.
Evolving changes: Any change in size, shape, or color warrants further evaluation.
Tips to preventing skin cancer:
reduce sun exposure
use sunscreen
wear protective clothing
adequate vitamin B3 (niancin)
examine skin for suspected lesions
Pressure Injuries
Pressure injuries occur when prolonged pressure on the skin restricts blood flow. They commonly appear over bony areas such as the heels, sacrum, back of the head, and elbows.
Individuals at higher risk include those who are critically ill, immobile, poorly nourished, or have sensory issues.
Stages of Pressure Injuries
Stage 1: Red area that does not turn white when pressed (nonblanchable).
Stage 2: Partial skin loss with exposed dermis; may include blisters.
Stage 3: Full thickness skin loss affecting deeper layers.
Stage 4: Very deep injury exposing bone, muscle, or tendons.
Deep Tissue Injuries
These injuries appear as dark red or purple areas and may show signs of a blood-filled blister. They differ from regular pressure injuries as they affect deeper tissue layers.
Unstageable Injuries
These cannot be accurately staged due to slough (dead tissue) or eschar (scab).
Risk Assessment
The Braden Scale is used to predict the risk of developing pressure injuries. Regular assessments should be done, especially on vulnerable areas.
Prevention Strategies
Change the patient’s position every 2 hours in bed.
Lift heels off the bed (offload).
Reposition every 30 minutes while sitting.
Keep the head of the bed elevated to 30 degrees.
Use special mattresses and moisture-absorbing pads.
Encourage movement as tolerated and ensure nutritional needs are met.
Remove any cords or equipment from under the patient to prevent pressure.
Chapter 15: Head and Neck Assessment
Subjective Data
Hypothyroidism: Patients may report fatigue, weight gain, cold intolerance, dry skin, and hair loss.
Hyperthyroidism: Symptoms to inquire about include weight loss, heat intolerance, increased appetite, anxiety, and tremors.
Goiter: Ask about visible swelling in the neck or any difficulty swallowing or breathing.
Headache: Inquire about headache characteristics (e.g., onset, duration), types (e.g., tension, migraine, cluster), locations, and associated symptoms (nausea, light sensitivity).
Traumatic Brain Injury (TBI): Assess history of head trauma and related symptoms such as confusion, balance issues, or changes in consciousness.
Objective Data
Normal Findings:
Thyroid size is usually not palpable and appears normal in imaging studies; no signs of goiter.
No abnormalities in neurological examination, with normal pupil responses and strength.
Headaches typically not associated with abnormal neurological signs.
Abnormal Findings:
Hypothyroidism: Enlarged thyroid (goiter), decreased metabolic rate, potential bradycardia observed.
Hyperthyroidism: Enlarged thyroid, increased heart rate, tremors, warmth, and moist skin may be noted.
Goiter: Visible swelling in the neck.
Headaches: Identify patterns indicating migraines or tension headaches.
TBI: Changes in consciousness, imbalance, or neurological deficits may be seen.
Abnormal Findings (Signs & Symptoms)
Acromegaly: Enlarged hands and feet, facial changes (prominent jaw), potential glucose intolerance.
Cushing Syndrome: Weight gain, hypertension, facial puffiness, and purple striae may be present.
Scleroderma: Tight skin, joint pain, difficulty swallowing, and Raynaud's phenomenon observed.
Bell's Palsy: Sudden weakness in one side of the face, drooping mouth, and inability to close one eye.
Parkinson's Disease: Bradykinesia, resting tremor, rigidity, and postural instability noted in the examination.
Chapter 16: Biologic and Cultural Behavior Variations
Eye Color and Structural Features
Epicanthic Folds: Commonly observed in individuals of Asian descent and in some individuals with Down syndrome of non-Asian descent.
Protrusion of Eyes: Slightly more prevalent in African Americans, with less occurrence in Hispanic populations.
Freckles on Sclera: More frequently seen in darker-skinned individuals.
Optic Disc Size: Typically larger in African Americans compared to other ethnic groups.
Visual Impairment by Demographics
Visual impairment rates can vary based on age, gender, and geographic location.
Highly developed countries show different incidences of visual disorders compared to poorly developed nations.
Common Visual Disorders
Glaucoma: More prevalent in African Americans.
Age-Related Macular Degeneration (AMD): Higher rates found in Non-Hispanic Whites than in African Americans and Hispanics.
Cataracts: Higher incidence rates in Hispanic populations.
Diabetic Retinopathy: Lower rates in Non-Hispanic Whites compared to African Americans and Hispanics.
Trachoma and Corneal Diseases: Vary by geographic and socioeconomic status.
Children's Visual Diseases: Include cataracts, retinopathy of prematurity, and vitamin A deficiency.
Visual Acuity in the United States
Poorest Corrected Visual Acuity: Observed in Japanese and Chinese Americans, followed by African Americans and Hispanics.
Best-Corrected Visual Acuity: Generally found in Native Americans and Whites.
Epidemic of Myopia: Notably prevalent among Eskimo populations.
Causes of Visual Impairment by Ethnic Groups
Non-Hispanic Whites: Display lower rates of diabetic retinopathy and glaucoma but higher rates of AMD.
Hispanics: More frequently diagnosed with cataracts compared to Non-Hispanic Whites.
African Americans: Show a higher prevalence of glaucoma compared to other ethnic groups.
Vision Acuity Test
Techniques for properly evaluating vision and interpreting results provide insights into ocular health.
Interpretation of Results from Eye Tests
Snellen Chart: Measures visual acuity, determining how well a person can see at a distance. A higher number indicates better vision.
E Chart: This chart is like the Snellen Chart but is made for people who can't read letters. It helps to check how well someone can see by using different pictures instead of letters.
Jaeger Test: Assesses near vision, commonly used for determining reading and close-up vision capabilities; the smallest readable print size indicates the level of near vision acuity.
Glaucoma
Causes: Glaucoma usually happens when the pressure inside the eye gets too high, which can hurt the optic nerve. Age, family history, and health issues like diabetes can increase your chances of getting it.
Signs: In the early stages, there may be no obvious signs. As it gets worse, you might notice problems with your side vision and, in severe cases, can go blind.
Symptoms: Common symptoms include blurry vision, seeing halos around lights, and difficulty seeing in dim light.
Screening: It's important to have regular eye check-ups for early detection. These exams often include checking eye pressure, looking at the health of the optic nerve, and testing side vision. People over 40, especially with risk factors, should get screened regularly.
Risk Factors: Key risk factors include:
Being over 40 years old
Family history of glaucoma
Having health problems like diabetes or high blood pressure
Being of African descent
Injuries or surgeries to the eye
Long-term use of steroids.
Macular Degeneration
Causes: Macular degeneration occurs when the central part of the eye (macula) gets damaged, often due to aging, genetics, or other health problems.
Signs: Look for blurred vision in the center, problems seeing details, and straight lines looking wavy.
Symptoms: Common signs include blurry vision, dark spots in the center of sight, and difficulty recognizing faces or reading.
Screening: It's important to have regular eye exams. Eye doctors can use special tools to look for early signs.
Risk Factors: Key factors that increase risk include being over 50, having a family history of the condition, smoking, being overweight, and having high blood pressure.
Cataracts
Causes: Cataracts often happen with age when the eye lens gets cloudy. They can also be caused by diabetes, long-term steroid use, and too much sunlight.
Signs: Early signs include blurry vision, trouble seeing at night, and being sensitive to light. Without treatment, they can make daily activities hard.
Symptoms: People may notice colors look faded, see double, or need frequent updates to their glasses prescription.
Screening: Regular eye exams can catch cataracts early. An eye doctor checks for cloudiness in the lens during exams.
Education: Protect eyes from UV light with sunglasses, get regular eye check-ups, and eat a healthy diet to help lower the risk of cataracts.
Abnormal Findings of the External Eye
Presentations: Look for any unusual shapes, colors, or sizes of the eyes, swelling, redness, or discharge that shouldn't be there.
Abnormal Findings of Extraocular Muscle
Terms: Common terms include strabismus (eyes point in different directions), nystagmus (involuntary eye movement), and limited eye movement.
Abnormal Findings of the Pupils
Terms: Key terms include anisocoria (unequal pupil sizes), non-reactive pupils (pupils that don't respond to light), and sluggish pupils (slow to react to light).
Chapter 17:
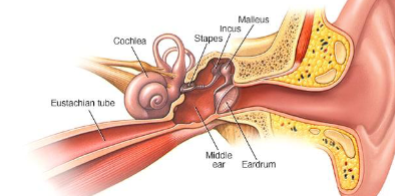
Middle Ear
Tympanic Cavity: This is a small chamber filled with air that is situated within the temporal bone of the skull.
Tympanic Membrane: Commonly known as the eardrum, this membrane acts as a barrier that separates the outer ear from the middle ear.
Windows: The middle ear contains two essential openings called the round window and the oval window, which help transmit sound vibrations.
Auditory Ossicles: The middle ear houses three tiny bones known as the malleus (hammer), incus (anvil), and stapes (stirrup). These bones work together to amplify sound waves that enter the ear.
Eustachian Tube: This tube connects the middle ear to the back of the throat, helping to maintain equal pressure on either side of the eardrum and allowing for drainage of fluids.
Hearing Loss
Conductive Hearing Loss: This happens when something blocks or hurts the inner ear, making it hard for sound to get through.
Sensorineural or Perceptive Hearing Loss: This type of loss is due to damage in the inner ear, which makes it hard to notice and understand sounds.
Abnormal Findings
Acute Otitis Media (AOM)
Acute Otitis Media (AOM) is an infection in the midd le part of the ear. It happens when bacteria or viruses cause swelling and fluid buildup behind the eardrum. AOM often comes after a cold or other respiratory infection.
Symptoms:
Ear pain, especially when lying down.
Fussiness and irritability in children.
Fever and trouble sleeping.
Difficulty hearing things clearly.
Diagnosis:
A doctor checks the eardrum using an otoscope to see if it's red, swollen, or has fluid behind it.
They may also ask about symptoms and health history.
Treatment:
Pain relief with medications.
Antibiotics may be given if symptoms are severe or do not improve in a few days.
Sometimes, small tubes may be placed in the ear to help drain fluid and ease pressure.
Serous Otitis Media (OM)
Serous Otitis Media (OM) means there is fluid in the middle ear without an active infection. This can happen after AOM or for other reasons without sickness, often leaving fluid behind.
Symptoms:
A feeling of fullness in the ear.
Hearing loss or sounds might seem muffled.
Some people may hear popping or clicking noises when they yawn or swallow.
Diagnosis:
A doctor checks for fluid in the ear.
Hearing tests may help see how much hearing is affected.
Treatment:
It usually goes away on its own without special treatment.
If fluid stays for too long (over 3 months) or hearing loss is significant, doctors may suggest putting in tubes to drain the fluid and improve hearing.
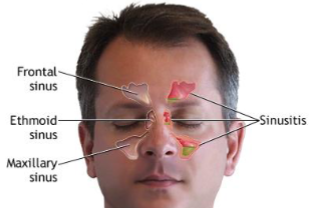
Chapter 18: Sinuses
four sinuses: frontal, maxillary, ethmoidal, sphenoidal
These sinuses are important for various functions, including lightening the weight of the skull, producing mucus, and contributing to sound produced by voice
Abnormalities of Mouth and Throat
Oropharyngeal Cancer:
What It Is: A type of cancer that occurs in the oropharynx, the part of the throat at the back of the mouth.
Signs:
Persistent sore throat
Difficulty swallowing
Unexplained weight loss
Changes in voice or speech
Growths or lumps in the neck
Symptoms:
Pain in the throat
Ear pain
White patches in the mouth
Bleeding in the mouth
Risk Factors:
Tobacco use (smoking/chewing)
Heavy alcohol consumption
Infection with human papillomavirus (HPV)
Being older (more common in people over 50)
Being male
Poor oral hygiene practices
Previous history of head and neck cancer.
Education:
Emphasize the importance of regular dental check-ups and good oral hygiene.
Encourage vaccination for HPV as a preventive measure.
Inform about the harmful effects of tobacco and excessive alcohol.
Educate on recognizing early signs and symptoms and seeking prompt medical advice if they occur.
Treatments:
Surgery to remove the tumor
Radiation therapy
Chemotherapy
Targeted therapy based on cancer characteristics, often done in combination for effectiveness.
Abnormalities of the Mouth and Throat
cold sores
sis of lips
carcinoma of lip
candida albicans infection
canker sore
gingivitis
receding gums
acute tonsillitis
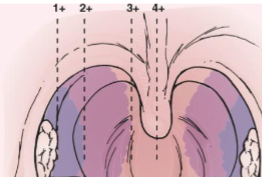
Grading of tonsils
1+ = visible
2+ = midway between tonsillar pillars and uvula
3+ = touch uvula
4+ = touch each other
Chapter 19:
Thoracic Cavity Components:
Suprasternal Notch: A small dip at the top of the breastbone (sternum) that helps doctors feel for structures in the chest during exams.
Sternal Angle: The point where the upper part of the sternum meets the lower part, used to find the second rib and help count the ribs.
Trachea: The tube (windpipe) that carries air from the throat to the lungs.
Bronchi: The big tubes that split from the trachea and go into each lung. They are the passageways for air.
Lungs: The main organs in the thoracic cavity that take in oxygen and get rid of carbon dioxide.
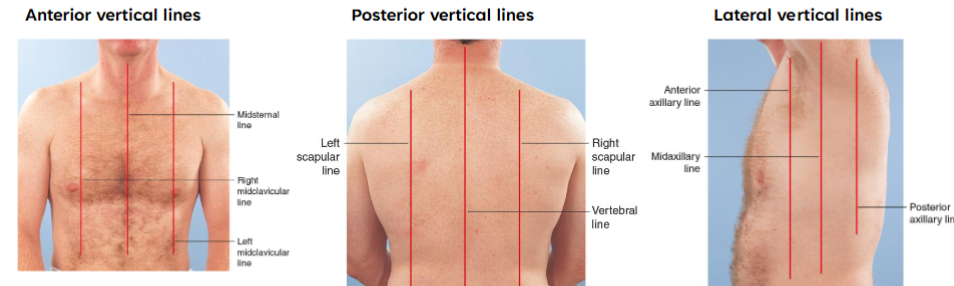
Vertical Reference Lines:
Anterior Axillary Line
Midclavicular Line
Sternal Line
Posterior Axillary Line
Scapular Line
Vertebral Line
Subjective Data:
Rationale: Information about the patient's breathing problems, chest pain, or lung infections.
Objective Data:
Normal Findings: Both sides of the chest expand equally, clear breath sounds are heard, and there’s no extra muscle use when breathing.
Abnormal Findings: Uneven chest movements, wheezing or crackling sounds when listening to the chest, or signs of trouble breathing.
Clinical Tips:
Keep an eye out for signs of lung infections and check for risk factors like smoking.
Breath Sounds:
Normal: Clear and soft sounds in the lungs.
Adventitious: Unusual sounds like wheezing (high-pitched), crackles (bubbling or rattling), and rhonchi (snoring).
Respiratory Patterns:
Normal: 12–20 breaths/min and regular.
Tachypnea: More than 24 breaths/min and shallow; may occur due to anxiety or exercise.
Bradypnea: Less than 10 breaths/min and regular; common in well-conditioned athletes, medication-induced depression of the respiratory center, diabetic coma, or neurological damage.
Hyperventilation: Increased rate and depth; often seen during extreme exercise, fear, or anxiety.
Kussmaul: Rapid, deep, and labored breathing; typically associated with diabetic ketoacidosis.
Hypoventilation: Decreased rate and depth with an irregular pattern; can result from narcotic or anesthetic overdose.
Cheyne-Stokes respiration: A regular pattern featuring alternating periods of deep, rapid breathing followed by apnea; associated with severe congestive heart failure, drug overdose, elevated intracranial pressure, or renal failure.
Biot's respiration: Irregular pattern marked by varying depth and rate followed by apnea; may indicate meningitis or severe brain damage.
Ataxic: A significant disorganization with irregular and varying depths of respiration; indicates respiratory compromise.
Air trapping: Increasing difficulty in expelling breath; commonly seen in COPD.
Lung Cancer:
Screening: Low-dose CT scans are recommended for people at high risk (like heavy smokers aged 55-80).
Risk Factors: Smoking, being around secondhand smoke, exposure to asbestos, and some genetic factors.
Education: Encourage quitting smoking, regular health check-ups, and being aware of symptoms like a persistent cough or unexpected weight loss, no beta carotene supplements.
Thoracic Deformities:
Thoracic Deformities and Their Effects on Breathing:
Barrel Chest:
What it looks like: The chest appears rounded and bulging.
How it affects breathing: This shape can make it hard for the diaphragm to move, which decreases how much air the lungs can hold and makes breathing less efficient.
Pectus Excavatum:
What it looks like: The chest has a noticeable inward curve, making it look sunken.
How it affects breathing: This can limit how well the lungs grow and work, making it harder to take deep breaths, especially when active.
Pectus Carinatum:
What it looks like: Often called pigeon chest, the chest sticks out.
How it affects breathing: This shape can restrict how well the lungs can expand, which makes breathing less efficient.
Scoliosis:
What it looks like: The spine bends sideways.
How it affects breathing: Depending on how severe it is, scoliosis can twist the rib cage and reduce the space for the lungs to expand and contract during breathing.
Kyphosis:
What it looks like: The spine curves outward excessively, leading to a hunched back appearance.
How it affects breathing: This can push down on the lungs, making it harder to take full, deep breaths.
Athletes with Overhead Movements:
What it looks like: Athletes who frequently raise their arms can develop posture issues.
How it affects breathing: Repeated overhead movements can tighten the chest muscles and limit how well the chest can move, affecting breathing during intense exercise.