5.Alcohol
Ethyl Alcohol
Alcohol in common use refers to ethyl alcohol (C₂H₅OH).
History of Alcohol
Origin: Alcohol's history is intertwined with the development of human societies.
Early Awareness: Initial recognition likely arose from consumption of yeast-contaminated foods.
Cultural Presence:
Indian: Known as 'sura'; drinking termed as 'surapanam'.
Jewish: Commonly represented in wine.
Arabic: 'Arrack' from 'arag', translating to 'sweet liquor'; 'alcohol' from 'alkohl'.
Modern Alcohol Preparations
Types of Alcoholic Beverages: Includes whisky, brandy, rum, gin, vodka, beer, champagne, etc.
Branding: Notable brands, e.g., Chivas Regal, Bacardi, Smirnoff, possess unique preparation methods and flavor profiles.
Aging Process: For example, Scotch whisky is aged in oak barrels for specific durations (e.g., 12 or 25 years).
Alcohol as a Social Symbol
Cultural Significance: Alcohol often considered a status symbol in social gatherings.
Trends: Increasing number of alcohol consumers leading to various societal challenges.
Societal Issues Related to Alcohol Consumption
Challenges:
Alcohol-related crimes.
Impact on family structures.
Rise in juvenile delinquency and drinking and driving incidents.
Alcohol Concentrations
Types:
Absolute Alcohol: 99.95% ethyl alcohol.
Rectified Spirit: 90% ethyl alcohol.
Methylated Spirit: 95% ethyl alcohol, 5% methyl alcohol.
Proof Spirit: 49.24% alcohol by weight (57.10% by volume).
Proof Classification:
Less than 49.24% is under-proof.
More than this is over-proof.
Regulations in India: According to the Abkari Act, alcoholic beverages shouldn't exceed 42.83% by volume (75-proof).
Alcoholic Beverages
Definition: Alcoholic beverages are mixtures of ethyl alcohol, water, and congeners (≤0.5%).
Congeners: Include propyl alcohol, acetyl alcohol, aldehydes, esters, ketones, and organic acids, contributing flavor and color.
Types of Alcoholic Beverages:
Whisky
Brandy
Vodka
Gin
Rum
Beer (2-6% alcohol)
Light wine (7-12% alcohol)
Reinforced wine (15-20% alcohol)
Champagne (10-15% alcohol)
Feni (Goan spirit from cashew apple)
Toddy (from coconut/palm tree sap)
Ayurvedic Preparations: Arishtas and Savas with various alcohol concentrations.
Absorption of Alcohol
Absorption Sites:
20% absorbed from the stomach
80% absorbed from the small intestine
Absorption Timeline:
60% within 30 minutes
90% within 1 hour
Maximum concentration reached in about 1 hour.
Factors Delaying Absorption
High-fat and protein-rich foods
Chilled or iced drinks
Concentrated drinks without dilution
Gastritis
Pyloric stenosis and spasm
Factors Increasing Absorption
Adding soda or aerated drinks
Drinking on an empty stomach
Dilution to 10-20% concentration
Gastrectomy
Consuming warm drinks
Distribution of Alcohol
Alcohol is evenly distributed throughout the body and can easily pass the blood-brain barrier.
Exists in various concentrations in body fluids and organs.
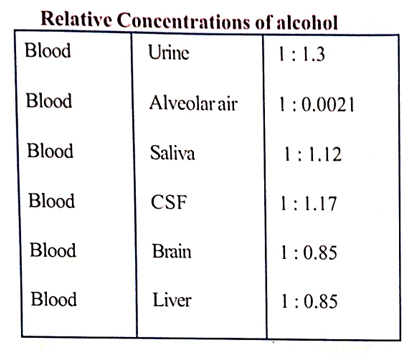
Relative concentrations:
Metabolism of Alcohol
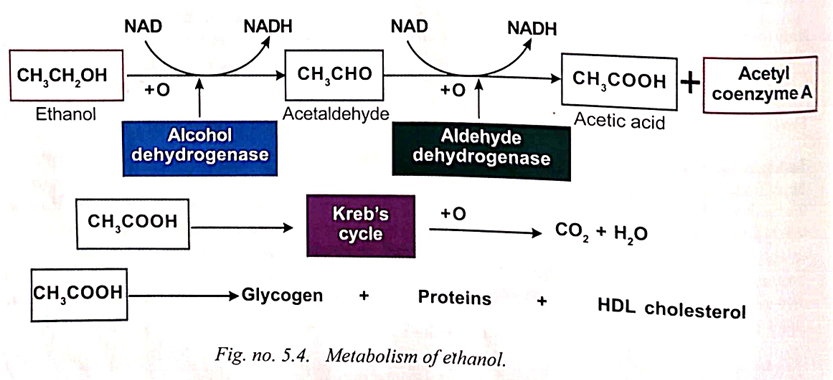
90% of alcohol is metabolized in the liver, specifically:
Step 1: Ethanol is oxidized to acetaldehyde by the enzyme Alcohol Dehydrogenase (ADH) with the coenzyme Nicotinamide Adenine Dinucleotide (NAD).
Step 2: Acetaldehyde is converted to acetic acid and its activated form, acetyl coenzyme A.
Final Conversion: Acetic acid is further converted to CO₂ and water through the Kreb's cycle.
Acetate can also form glycogen, proteins, fats, and HDL cholesterol.
Mild doses of alcohol (e.g., 21 units/week for males, 14 units/week for females) may prevent heart attacks due to its metabolic benefits.
Detoxification Rate
Alcohol is detoxified from the blood at a rate of 15 mg/100 ml/hour.
In chronic alcoholics:
Amount of detoxifying enzymes increases.
Metabolic rate may increase to 40-50 mg/100 ml/hour unless liver damage occurs.
Reduced metabolic rate in chronic alcoholics with liver damage may lead to prolonged intoxication even with small amounts of alcohol.
Excretion of Alcohol
90% of alcohol is eliminated through liver detoxification and oxidation.
Remaining alcohol is excreted unaltered via:
Saliva
Sweat
Urine
Exhaled air.
Action on the Nervous System
Alcohol crosses the blood-brain barrier and affects nerve cells as a selective depressant.
It inhibits several receptors including:
NMDA (N-methyl-d-aspartate) receptors
GABA receptors
5HT3 receptors.
Alcohol depresses higher centres in the cerebral cortex responsible for:
Conduct
Judgement
Self-criticism.
Inhibition of these centres can lead to unrestrained behavior.
Gradual increase in concentration depresses vital centers in the midbrain and medulla, leading to cardio-respiratory failure.
Causes generalized vasodilatation, leading to a feeling of warmth but increased heat loss.
Moderate consumption increases appetite; high doses lead to appetite loss.
Induces diuresis by inhibiting antidiuretic hormone (ADH) release from the posterior pituitary.
Causes hypoglycemia by two mechanisms:
Inhibiting glucose formation from lactate and glycogenic amino acids in the liver.
Stimulating insulin production from pancreatic beta cells.
Synergistic effects can occur with sedatives, tranquilizers, antihistamines, and barbiturates when combined with alcohol.
Stages of Alcohol Intoxication
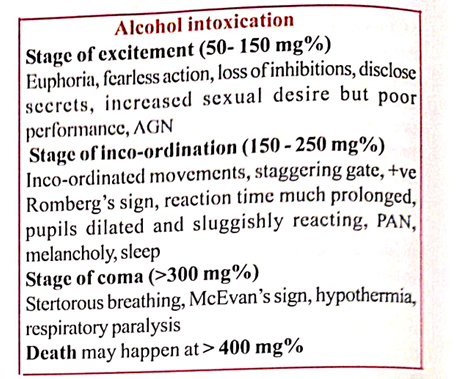
1. Stage of Excitement (50 to 150 mg/100 ml)
Initial feeling of well-being, increased confidence, and lack of self-control.
Normal decorum forgotten; may engage in fearless and reckless behavior.
Visual impairments occur with blood alcohol level over 40 mg%.
Symptoms include alcohol gaze nystagmus (AGN) at 50 to 100 mg%.
Increased sexual desire but impaired performance (erection and ejaculation issues).
Reaction time increases.
2. Stage of Incoordination (150 to 250 mg/100 ml)
Coordination of movements is affected; loss of sense perception.
Difficulty with skilled tasks (e.g., buttoning clothes).
Symptoms include slurred speech, unsteady gait, and possible irritability or quarrelsomeness.
Romberg sign +ve
Blood alcohol over 200 mg/100 ml leads to ataxia and positional alcoholic nystagmus (PAN).
Sensory functions (taste, touch, smell, hearing) diminished; pupils dilated and sluggish.
At 200 to 250 mg%, may experience hiccups, retching, and vomiting as a compensatory mechanism.
Gradual sleep, hypothermia, increased sweating
3. Stage of Coma (more than 300 mg/100 ml)
Possible progression to coma; stertorous breathing observed.
Rapid pulse, subnormal temperature, and pupils constricted.
Reflexive dilation of pupils upon irritation (Mc Ewan's pupil).
Coma primarily due to hypoglycemia; becomes irreversible with cortical center hypoxia.
Recovery may transition from coma to deep sleep, often accompanied by waking depression.
Mood changes, nausea, and headache are common symptoms of an alcohol hangover.
About 15% of drinkers may experience a blackout, which is a temporary anterograde amnesia where the person forgets events from a drinking session.
Risk of Death
Death can occur at blood alcohol concentrations (BAC) over 400 mg% due to:
Respiratory failure from brain stem hypoxia.
Aspiration of regurgitated food in intoxicated individuals.
Possible head injuries from falls due to unsteady gait.
Drowning in shallow water.
Blood Alcohol Concentration (BAC) Levels (UQ)
Blood Alcohol Concentration (mg%) | Stage | Clinical Features |
|---|---|---|
< 50 mg% | Sobriety | Near normal behavior. |
50-100 mg% | Euphoria | Feeling of well-being, increases in talkativeness, decreased inhibitions, and heightened self-confidence. |
100-150 mg% | Excitement | Emotional instability, impairment of memory |
150-200 mg% | Confusion | Disorientation, confusion, vertigo, diplopia (double vision), ataxia (lack of muscle control), slurred speech, staggering gait, positive Romberg’s sign, muscular incoordination, and increased reaction time. |
200-300 mg% | Stupor | General inertia, diminished response to stimuli; inability to stand or walk, vomiting, and may fall asleep. |
300-400 mg% | Coma | Unconsciousness, abolished reflexes, subnormal body temperature, labored breathing, and presence of McEwan’s pupil |
400-500 mg% | Death | Death due to respiratory failure. |
Treatment of Acute Alcohol Intoxication
If the patient is in a coma, supportive measures are essential, including airway maintenance.
Endotracheal intubation and gastric lavage should be considered within 2 hours of ingestion.
Intravenous administration of 50-100 ml of fluids may be required.
Dextrose: 5% dextrose should be given.
Warmth: The body can be kept warm.
Metabolic Acidosis: Can be corrected by sodium bicarbonate.
Respiratory Support: Respiratory stimulants and artificial respiration are beneficial.
Dialysis: Hemodialysis or peritoneal dialysis can be performed.
Postmortem Findings
Congestion: Internal organs, especially lungs, will be congested and edematous.
Alcohol Smell: There will be a smell of alcohol in the stomach.
Blood Collection:
Samples collected from neck veins for alcohol estimation.
Free blood from pleural or other cavities should not be collected to avoid false results.
30 ml of blood in a glass bottle with sodium fluoride as preservative (100 mg/10 ml).
Measurement of Alcohol Concentration
Widmark's Formula: (UQ)
a = cpr, where:
a = total alcohol weight (grams)
c = alcohol concentration in blood (gm/kg)
p = body weight (kg)
r = constant (0.6 for men, 0.5 for women)
For urine:
a = ¾ qpr
q = concentration in urine (mg/kg)
Methods for Alcohol Estimation:
Gas chromatography (most accurate)
Kozalka and Hine method, Cavett method (micro-methods)
Drunkenness
Definition (UQ): According to the British Medical Council
State produced by taking alcohol in a quantity sufficient to make him to lose control of his faculties to such an extent to render him unable to execute safely the occupation in which he is engaged at the material time"
Diagnosis: Made based on clinical signs and symptoms.
Blood Collection Procedure:
Clean venipuncture site with soap and water.
Blood collected from anterior cubital vein or femoral vein using a syringe.
10 ml of blood should be collected in a tightly stoppered container with sodium fluoride (preservative 100 mg for 10 ml).
Alcohol Measuring Devices
Breath Analyzer (Breathalyzer):
Estimates blood alcohol concentration from breath sample.
Invented by Dr. Robert Borkenstein.
Based on the principle that 200 ml of alveolar air contains the same amount of alcohol as 1 ml of blood.
Potassium dichromate in the analyzer oxidizes ethanol and indicates concentration through color change.
Infra-red spectroscopic method is used.
Alcometer:
Measures blood alcohol concentration and provides a printout (alcoprint).
Conditions Simulating Alcohol Intoxication
Numerous medical conditions can mimic alcohol intoxication; these must be identified and treated to prevent negligence.
Head Injury: Can confuse symptoms similar to intoxication.
Metabolic Disorders: e.g., hypoglycemia, diabetic pre-coma, uremia.
Neurological Conditions: e.g., intracranial lesions, Parkinson's disease, post-epileptic automatism.
Drugs: Insulin, hypoglycemic agents, barbiturates, morphine, tranquilizers.
Psychological Conditions: e.g., hypomania.
Others: High fevers causing delirium, CO poisoning, LSD, Ganja.
Types of Tolerance to Alcohol
Tissue Tolerance: Increased sensitivity, typically seen in CNS neuronal cells.
Metabolic Tolerance: Increased absorption, metabolism, and elimination rates, involving hepatic enzymes like CYP2E1.
Acute Functional Tolerance: Develops during a single exposure to alcohol.
Hazards of Alcohol Intoxication
Risk of head injuries from falls.
Possible drowning in shallow water.
Aspiration of vomit leading to suffocation.
Choking on food due to impaired gag reflex.
Potential burns from cigarettes in bed.
Saturday night paralysis due to pressure on the radial nerve during sleep.
Increased likelihood of accidents while driving.
Micturition syncope: Sudden loss of consciousness during urination.
Holiday heart syndrome: Atrial fibrillation after heavy drinking episodes.
Acute Alcoholism Complications
Potential for traumatic subarachnoid hemorrhage (SAH) due to:
Loss of muscular coordination with excessive head movements.
Increased hemorrhage risk from dilated vessels.
Bounding pulse effects in intoxicated individuals.
Drunkenness and Driving Regulations
Motor Vehicle Act (1939, amended multiple times until 2019) regulates alcohol consumption while driving.
Legal Limit: Blood alcohol concentration exceeding 30 mg% is an offense (Sec 185 MVA).
Penalties: First offense: up to Rs. 2,000 fine or 6 months imprisonment; subsequent offenses: up to Rs. 3,000 fine or 2 years imprisonment.
Amendment 2019: Penalty increased to Rs. 10,000.
Police can arrest without warrant if in uniform (Sec 202).
Impact of Alcohol on Driving Ability (UQ)
Alcohol may lead to:
Overconfidence: Resulting in reckless driving.
Vision Impairment: Blurring and reduced visual acuity due to pupil dilation.
Tunnel Vision: Narrowing of the field of vision.
Coordination Loss: Impairs control over steering, brakes, and accelerator.
Alcohol prolongs reaction time significantly.
Movements become sluggish; impaired ability to act quickly.
Example: Delayed braking response can lead to vehicle collisions.
Loss of orientation and impaired attention due to alcohol effects.
Symptoms like nystagmus may further affect driving capabilities.
Alcohol and crimes
According to Section 85 IPC(BNS 23), an intoxicated person is not responsible for crimes if they were incapable of understanding the act, and intoxication was administered without knowledge.
Section 86 IPC (BNS 24) states that voluntary drunkenness does not exempt a person from criminal responsibility.
Criminals often consume alcohol for courage before committing crimes.
Alcohol Withdrawal Syndrome (AWS)
Sec 510 IPC,BNS 355: Misconduct in public under the influence can lead to a 24-hour imprisonment or a fine of up to 10 rupees.
Symptoms of AWS:
Appear within 12 to 48 hours post-withdrawal.
Common symptoms: coarse tremors (hands, tongue, eyelids), nausea, vomiting, malaise, hypertension, tachycardia, sweating, anxiety, irritability, headache, insomnia.
Withdrawal seizures can occur 6 to 48 hours after the last drink.
Symptoms can subside with alcohol administration.
Severe complications: hallucinations, memory loss, delirium tremens.
Treatment for Alcohol Withdrawal
Treatment options:
20 mg of Chlordiazepoxide or 100 mg of Diazepam, four times a day.
Chronic Alcoholism
Chronic alcoholism leads to:
Gradual physical, mental, and moral deterioration.
Almost irreversible somatic brain changes from continued alcohol use.
Physical Diseases Associated with Chronic Alcoholism
Loss of appetite, chronic gastritis, wasting, peripheral neuritis, impotence, fatty liver, etc.
Specific Conditions:
Mallory-Weiss Syndrome: Gastro-esophageal junction tears causing hematemesis.
Alcoholic Cirrhosis and portal hypertension.
Beer cardiomyopathy ('Munich beer heart').
Pancreatitis.
Holiday heart syndrome: Atrial fibrillation linked to drinking.
Mental Diseases Associated with Chronic Alcoholism
Memory and Judgment: Significant memory loss and impaired judgment abilities.
Clinical Syndromes:
Delirium Tremens, Wernicke's Encephalopathy, Korsakoff's Psychosis, Alcoholic Hallucinosis, Marchiafava-Bignami Syndrome, Alcoholic Paranoia, Alcoholic Seizures (Rum fits).
Delirium Tremens
Definition: Mental instability due to prolonged alcohol impact on the CNS, especially in chronic alcoholics.
Causes:
Sudden withdrawal of alcohol.
Temporary excessive alcohol intake.
Following injuries or infections.
Symptoms:
Symptoms arise 72 to 96 hours after the last drink.
Acute mental illness with lost time and space orientation.
Uncontrollable fear and anxiety are prevalent.
Coarse muscular tremors of face, tongue, and hands.
Insomnia and restlessness.
Memory loss.
Autonomic Symptoms:
Autonomic hyperactivity.
Increased psychomotor activity.
Hallucinations:
Visual and auditory hallucinations, possibly of a horror type.
Tactile hallucinations (insects crawling under the skin).
Micro-hallucinations (Lilliputian hallucinations).
Carphologia (picking imaginary objects).
Treatment:
Patient should be restrained in bed.
Sedatives (e.g., diazepam 40-80 mg per day in divided doses).
Close monitoring due to suicidal and homicidal tendencies.
Symptomatic management required.
Medico-legal Point:
Actions during delirium tremens (Sec 84 IPC, BNS 22) considered as mentally unsound.
Wernicke's Encephalopathy
Causes:
Chronic alcoholism leading to Vitamin B-1 (thiamine) deficiency.
Affects spinal cord and brain.
Symptoms typically onset after persistent vomiting.
Signs and Symptoms:
Ocular: Nystagmus, ophthalmoplegia (6th nerve), papilledema, retinal hemorrhage.
CNS: Disorientation, confusion, delirium, stupor, possible coma (high mortality risk within 24 hours).
PNS: Peripheral neuropathy, numbness in lower limbs.
Pathology:
Neuronal degeneration and hemorrhage in thalamus, mammillary bodies, periaqueductal region of the midbrain.
Korsakoff's Psychosis
Overview:
Occurs after Wernicke's encephalopathy (Wernicke-Korsakoff syndrome).
Causes:
Severe untreated thiamine deficiency from chronic alcoholism.
Signs and Symptoms:
Impaired recent memory with imaginative confabulation.
Impaired insight and inability to learn new information.
Considered as organic amnestic syndrome or alcohol dementia.
Pathology:
Degenerative changes in peri-ventricular and peri-aqueductal grey matter, thalamus, mammillary bodies, cerebellum.
Treatment:
Intravenous thiamine and electrolyte supplementation.
Significance:
Thiamine serves as a co-factor for essential enzymes in lipid metabolism (e.g., transketolase, pyruvate dehydrogenase).
Alcohol interferes with thiamine absorption, leading to brain injury especially in thalamus and mammillary bodies within about 3 weeks of deficiency.
Marchiafava-Bignami Syndrome
Characteristics:
Symptoms include disorientation, epilepsy, ataxia, dysarthria, spastic limb paralysis.
Possible association with hallucinations and personality/intellectual deterioration.
Cause:
Nutritional deficiency related to chronic alcohol consumption, particularly in red wine drinkers.
Pathological Changes:
Widespread demyelination in the pons, corpus callosum, optic tract, and cerebellum.
Alcoholic Hepatitis
Alcoholic hepatitis is characterized by twisted, rope-like bodies in the cytoplasm of ballooned hepatocytes, known as Mallory-Denk bodies.
Also referred to as alcoholic steatohepatitis.
While characteristic, Mallory-Denk bodies are not pathognomonic for the condition.
Classification of Alcohol Dependence
Alpha Alcoholism: Excessive drinking without dependence.
Beta Alcoholism: No dependence, but develops physical complications (e.g., gastritis, cirrhosis).
Gamma Alcoholism: Physical and psychological dependence, with tolerance and withdrawal symptoms.
Delta (French) Alcoholism: Strong dependence due to long-term use.
Epsilon Alcoholism: Dipsomania leading to drinking to death.
Treatment for Chronic Alcohol Intoxication/Dependence
CAGE Questionnaire: Used to assess the level of alcohol dependence
Alcohol addicts: Individuals who cannot stop drinking or suffer from withdrawal symptoms requiring treatment.
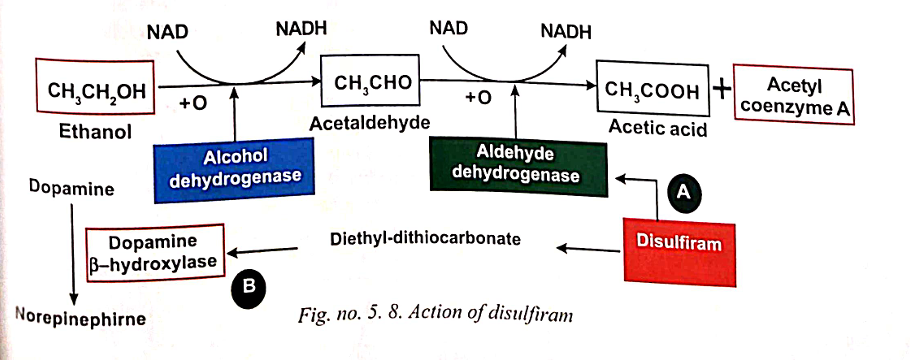
Disulfiram (Antabuse)
Administered in a starting dose of 250 mg, gradually reduced to 0.125-0.25 mg.
Inhibits aldehyde dehydrogenase, causing accumulation of acetaldehyde, which leads to unpleasant symptoms, causing aversion to alcohol.
Symptoms include flushing, palpitations, anxiety, sweating, headache, abdominal cramps, nausea, and vomiting.
It is also converted to diethyl-dithiocarbonate, stimulating dopamine β-hydroxylase and increasing norepinephrine production from dopamine.
Figure : Shows the action of Disulfiram.
Alternative Treatments
Alcoholics Anonymous: An international self-support organization of ex-alcoholics encouraging sobriety, established in the USA in 1925 with branches worldwide, including India.
Methyl Alcohol (Methanol, CH₃OH)
Toxicity: 3 times more toxic than ethyl alcohol.
Sources: Obtained by destructive distillation of wood; also known as wood naphtha or wood spirit. Can be found in some homemade beverages.
Physical Properties: Colorless liquid, similar smell to ethyl alcohol.
Absorption, Fate, and Excretion
Incidents: Mass casualties reported in India due to consumption of ethyl alcohol adulterated with methyl alcohol, leading to blindness.
Absorption: Rapidly absorbed through stomach, intestine, lungs, and skin.
Distribution: Distributed in tissues relative to water content; high concentration in vitreous body and optic nerve.
Metabolism: Oxidized in the liver, slower than ethyl alcohol (1/5 rate).
Oxidation Process:
Methyl alcohol → Formaldehyde → Formic acid
Enzymes: Alcohol dehydrogenase (first step) and aldehyde dehydrogenase (second step).
Co-enzyme: NAD converted to NADH.
Toxic Action and Effects
Action: Depressant of CNS; resembles ethyl alcohol but causes earlier toxic symptoms.
Toxicity of Metabolites:
Formaldehyde: 33 times more toxic than methyl alcohol.
Formic acid: 6 times more toxic than formaldehyde.
Health Impacts: Causes high anion gap metabolic acidosis and renal toxicity. Damage to retinal cells due to formic acid accumulation.
Ingestion Effects: Formic acid does not cause retinal toxicity since it cannot enter retinal cells.
Mechanism: Inhibition of cytochrome oxidase chain, leading to increased lactic acid production.
Hepatotoxicity: Methanol is liver toxic.
Fatal Dosage and Blood Concentration
Fatal Dose: 60-120 ml of methyl alcohol.
Critical Blood Concentration: > 100 mg%; > 80 mg% is dangerous.
Fatal Period: 24-36 hours; death may be delayed 2-4 days with treatment.
Signs and Symptoms of Methyl Alcohol Poisoning
Gastrointestinal: Nausea, vomiting, dehydration, abdominal pain.
Respiratory: Dyspnoea, cyanosis.
Central Nervous System: Headache, dizziness, vertigo, muscular weakness, bradycardia, hypothermia, coma, delirium, convulsions.
Renal: Scanty urine with acetone, formates, and lactates. Metabolic acidosis due to enzyme inhibition.
Ocular: Early symptoms include visual disturbances (photophobia, blurring-snowfield vision, scotoma). Accumulation of formic acid leads to blindness.
Fundoscopic Findings: Degenerative changes and edema in retinal cells and optic disc.
Pancreatic Effects: Possible pancreatitis.
Outcome in Fatal Cases: Coma, convulsions, respiratory failure, potential complete blindness in survivors.
Treatment (UQ)
Gastric Lavage:
Perform with 5% sodium bicarbonate solution in warm water, leaving some solution in the stomach.
Activated Charcoal: Reduces mortality by decreasing absorption from the GIT.
Calcium Folinate i.v.:
Reduces blood formic acid levels.
Dosage: 50-75 mg every 6 hours.
Ethyl Alcohol:
Dosage: 60 ml orally every 2 hours for 4-6 days.
Alcohol dehydrogenase has a higher affinity for ethyl alcohol than methyl alcohol, promoting elimination of methanol.
Sodium Bicarbonate i.v.:
Recommended in cases of severe metabolic acidosis.
Hemodialysis:
Treatment of choice in critical cases.
Fomepizole (4-Methyl Pyrazole):
An alcohol dehydrogenase inhibitor that prevents CNS depression.
Dosage: 15 mg/kg body weight every 12 hours. Not available in India.
Symptomatic Treatment
Keep eyes covered to protect from light.
Postmortem Findings
Froth at Mouth and Nostrils.
Congestion and inflammation of stomach and intestinal mucosa.
Cerebral Congestion and Edema.
Congested Lungs and Possible Bronchopneumonia.
Fatty Change in the Liver.
Congestion in Spleen, Kidneys, and Adrenals.
Tubular Degeneration in Kidneys.
Necrosis and Hemorrhage in Pancreas.
Retina may exhibit necrosis and edema of optic disc.
Preserve viscera and the brain for chemical analysis.
Higher Alcohols:
1. Ethylene Glycol
Neurotoxic substance.
Properties:
Colorless, odorless, non-volatile liquid with a bitter sweet taste. Used as an industrial solvent, coolant, antifreeze.
Action:
Converted to glycolic, lactic, and oxalic acids, inhibiting oxidative phosphorylation.
Oxalic acid forms calcium oxalate crystals, causing acute renal failure.
Metabolic acidosis results from glycolic acid.
Acidosis Types:
High Anion Gap Acidosis: Ethanol, methanol, ethylene glycol, paraldehyde, salicylates, diabetic ketoacidosis, lactic acidosis.
Normal Anion Gap Acidosis: Caused by diarrhea and renal tubular acidosis.
Signs and Symptoms:
CNS depression, renal failure, metabolic acidosis, breathlessness, convulsions, coma.
Death may be due to renal or respiratory failure.
Histopathology:
Calcium oxalate crystals appear as brown-black pigments in renal tubules and vessels.
Fatal Dose: 100-200 ml.
Fatal Period: 1 to 2 days.
Treatment: Same as methanol poisoning.
2. Isopropanol (Isopropyl Alcohol)
Properties: Colorless, volatile liquid.
Action:
2-3 times more toxic than ethanol; more toxic than methanol.
Causes CNS depression, coma, respiratory failure; fruity odor due to acetone.
Signs and Symptoms:
CNS depression, hypothermia, hypotension.
Does not cause metabolic acidosis.
Treatment: Similar to methanol poisoning.
Mickey finn
Knockout drink laced with psychoactive drug chloral hydrate
Given to incapacitate someone
Date rape drug
 Knowt
Knowt