Muscle Anatomy and Physiology
Muscle System Notes
Outline of Key Topics
I. Muscle Anatomy (Skeletal)
II. Neuromuscular Junction (NMJ)
III. Muscle Contraction: Molecular Mechanisms
IV. Muscle Comparison: Cardiac Muscle
V. Muscle Contrast: Smooth Muscle
VI. Muscle Mechanics: Filaments and Fatigue
I. Muscle Anatomy (Skeletal)
Muscles have…
Excitability: Ability of muscle tissue to respond to stimuli (e.g., action potentials).
Contractility: The capability of muscle fibers to shorten when stimulated.
Elasticity: Tendency of a muscle to return to its original shape after contraction.
Extensibility: Ability of muscle tissue to stretch beyond normal length depending on its situation.
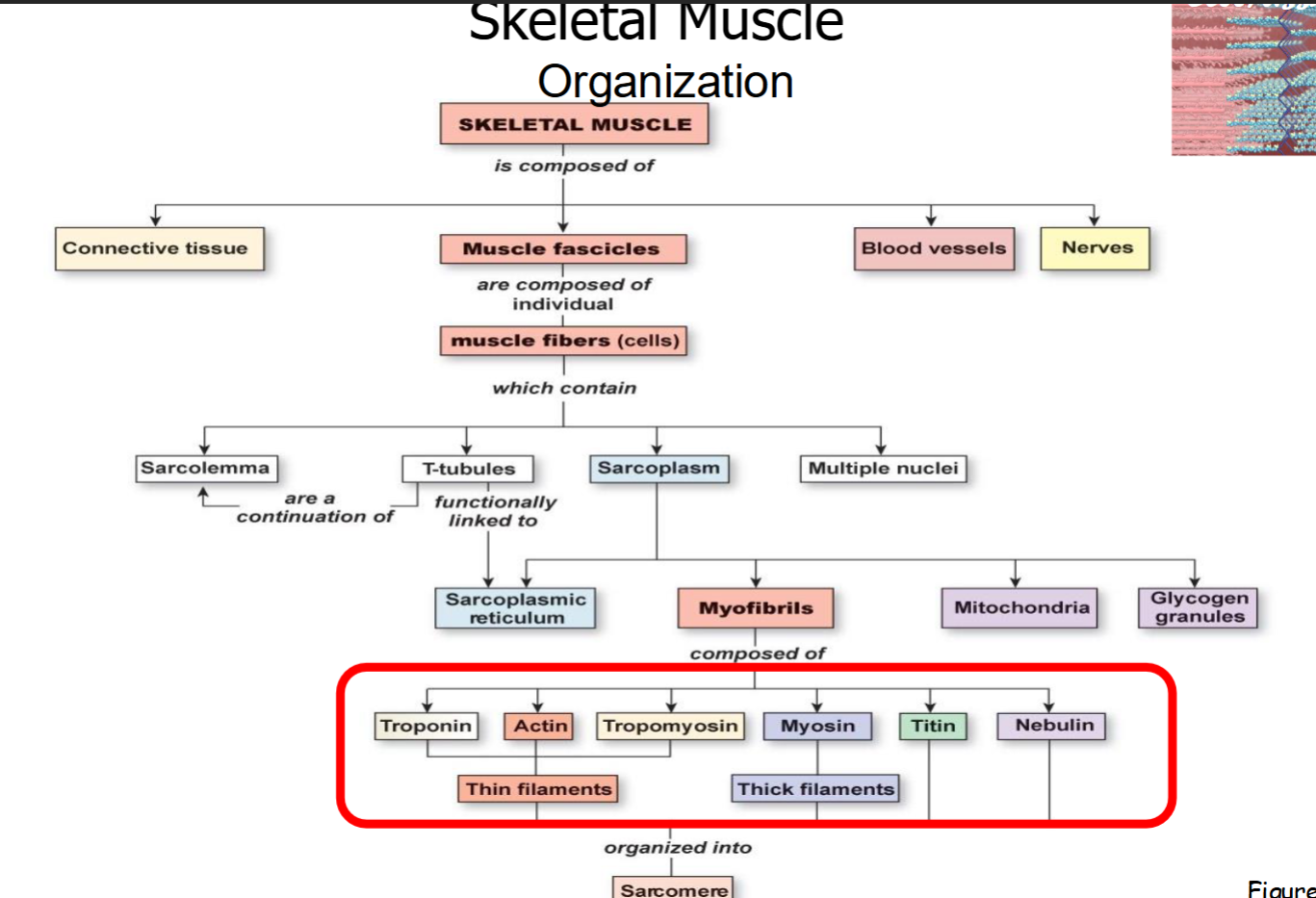
Broad Organization of Muscle
A full "muscle belly" features:
Fascicles: Bundles of muscle cells.
Muscle Cells (Fibers): Individual long cylindrical cells containing multiple nuclei; are full of myofibrils.
Myofibrils: Cylindrical bundles of filamentous contractile proteins (e.g., myosin and actin), synonymous with "muscle cell".
Myofilaments: Individual protein bundles within myofibrils (double-helical actin thin filament and myosin thick filament).
Specialized Sub-cellular Structures of Muscle Fibers
Connective Tissue: Provides support, strength, and protects muscle fibers.
Sarcolemma: Cell membrane of muscle fibers.
T-tubules (Transverse Tubules): Extensions of the sarcolemma; rich with leak K^{+} and voltage-gated Na^{+} & K^{+} channels, and DHP receptors (DHPRs); allow for action potentials to propagate throughout the fiber.
Sarcoplasmic Reticulum (SR): Specialized smooth endoplasmic reticulum that stores calcium ions; features extensive terminal cisternae surrounding T-tubules in a "triad" arrangement.
Blood Vessels and Nerves: Supplies nutrients and signals for contraction.
Sarcoplasm: Muscle fiber cytoplasm rich in organelles (e.g., mitochondria and glycogen granules).
Myofibrils
Composed of cylindrical protein structures called myofilaments.
Myofibrils contain repeating contractile units called sarcomeres.
Structural Terminology
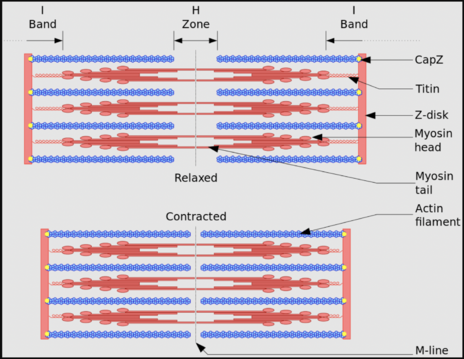
Sarcomere: Defined by the area between two adjacent Z-discs, acts as the functional contractile unit; encompasses:
M-line: Center of the A-band, anchoring thick filaments.
H-zone: Center of the A-band where only thick filaments are present.
I-band: Region containing only thin filaments, bisected by the Z-disc.
A-band: Region corresponding to the length of the thick filaments.
Z-discs: Anchor thin filaments and mark the boundaries of a sarcomere.
Myofilaments: Organized into two types:
Thin Filaments: Composed of actin (double-helical), troponin C, and tropomyosin.
Thick Filaments: Composed of myosin with its own fast endogenous ATPase activity to grant spring potential energy.
Accessory Proteins: Include titin (elastic, anchors myosin to Z-discs), nebulin (aligns the actin double helix thin filaments), and CapZ (holds actin to Z-discs).
Motor Units
Organization & Recruitment: Understand how motor units (a single motor neuron and all the muscle fibers it innervates) are organized and recruited to generate varying forces.
Motor Unit: single motor neuron and the muscle fibers it controls.
Usually contains just a few muscle fibers in an entire muscle.
A muscle may have many motor units.
Larger muscles have more motor units than do smaller muscles.
Each muscle fiber obeys the all or none principle. Either the whole muscle fiber contracts, or not at all.
As force increases, more and more motor units are recruited to generate larger force: Henneman’s Size Principle
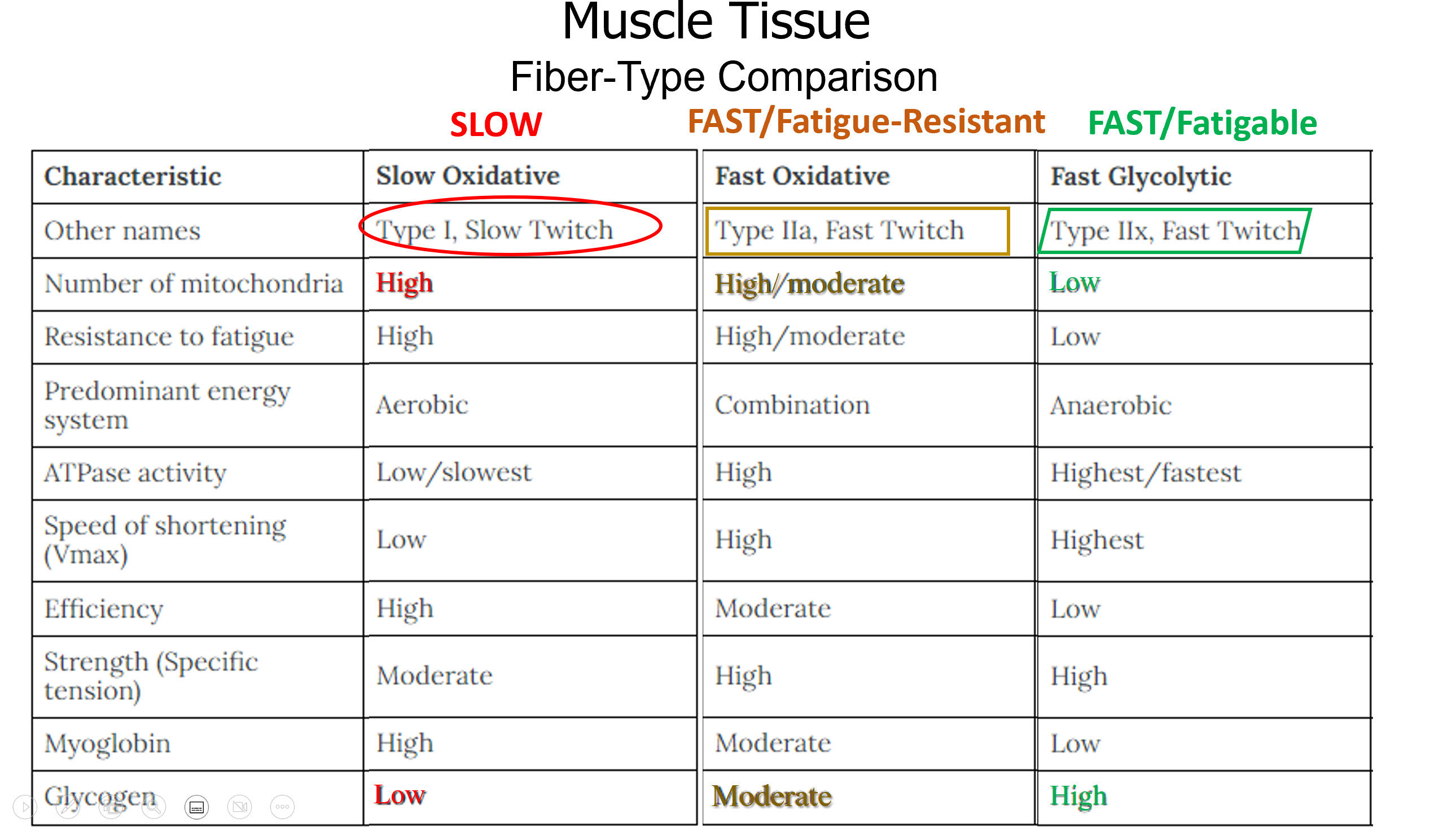
Fiber Types and order of recruitment.
S-Type/ Slow-oxidative fibers (Slow Twitch): Fatigue resistant, high endurance, easily excitable.
This will be ‘dark’ meat; will be found in the legs of the turkey. Dark because of mitochondria.
Fast-fatigue resistant fibers (Fast Twitch): Bigger, Average excitability; resistant to fatigue, helps you maintain an action.
Metabolic mode is glycolysis and oxidative.
Fast-fatigable fibers (Fast Twitch): Very big, low excitability. Not recruited unless needed. High power output but fatigue quickly
Why fatigue quickly? Few mitochondria, Anaerobic metabolism → less ATP available, low levels of myoglobin (that stores O2.)
Fagitable: Easily fatigued.
Only muscles that are activated by the same neuron will activate.
Small number of motor units = weak contraction
Large number of units at greater frequency = stronger contraction.
Fiber Type Comparison
II. Neuromuscular Junction (NMJ)
Definition: The synapse between a motor neuron(pre synaptic) and a muscle fiber (post).
Components of NMJ (in muscle fiber)
Synaptic Knob: Expanded end of the neuron containing vesicles.
Synaptic Vesicles: Membrane-bound sacs filled with acetylcholine (ACh).
Synaptic Cleft: Narrow gap between the synaptic knob and the motor end plate.
Motor End Plate: Region of the sarcolemma that contains folds and indentations to increase surface area, enhancing receptor availability.
ACh Receptors: Nicotinic ACh receptors located in the motor end plate; bind ACh to initiate muscle contraction.
Acetylcholinesterase (AChE): Enzyme that breaks down ACh quickly to terminate the signal.
Function: Order of Events at the NMJ
Shorter Order of Events:
Action potential (AP) propagates down motor neuron axon.
Voltage-gated Ca²⁺ channels in the motor axon terminal are activated.
Vesicles containing acetylcholine (ACh) are released.
Acetylcholine (ACh) binds to receptors (nAChR) on motor end plate
Non-specific cation channels (nAChR) open.
Motor end plate depolarization ("end plate potential" or EPP, which is a skeletal muscle EPSP).
Ca²⁺ is released from the sarcoplasmic reticulum (SR).
Ca²⁺ ions bind to troponin, troponin removes blocking sites from tropomyosin, active sites exposed.
Myosin – Actin cross bridges form; contraction.
Motor Neuron - Pre-synaptic Events:
Action Potential (AP): Arrives at the pre-synaptic terminal.
Depolarization: Triggers activation of voltage-gated Ca^{2+} channel. Ca^{2+} ions rush into the pre-synaptic terminal.
Vesicle Release: Ca^{2+} influx causes synaptic vesicles to fuse with the pre-synaptic membrane (exocytosis), releasing ACh into the synaptic cleft. (Know all 5 steps of vesicle release: docking, priming, fusion, release, recycling).
Ach diffuses across the synaptic cleft, 2 each binding to Ach Receptors
Channels (which are the same as the receptors) open.
Sodium ions enter muscle fiber, potassium ecits. Membrane potential becomes less negative- depolarizes.
Once Vm reaches threshold, action potential propagates along the sarcolemma.
ACh Action in Synaptic Cleft:
ACh Diffusion: ACh diffuses across the synaptic cleft.
ACh Binding: Two ACh molecules bind to each nicotinic ACh receptor on the motor end plate.
DHP is a modified Ca2+ channel receptor; voltage centers of t-tubules in muscles
Ryanodine Receptor(Ryr)has mechanical gating.
Muscle Cell - Post-synaptic Events & Excitation(Potential)-Contraction(Action) (Ca2+ )Coupling
Somatic motor neuron releases
ACh at neuromuscular junction.Net entry of Na+ through ACh
receptor-channel initiates a
muscle action potentialAction potential in t-tubule alters
conformation of DHP receptor.Ca2+ binds to troponin, allowing
actin-myosin bindingMyosin (motor protein) heads execute power
stroke, pulling the actin filaments toward the center of the sarcomereActin filament slides toward center
of sarcomere bc of pulling.
Calcium Center in…
Neurons: synaptotagmin 1,
Muscles: troponin
NMJ Dysfunction/Disorders
Myasthenia Gravis: An autoimmune disorder characterized by muscle weakness, especially in the face and throat, resulting from antibodies blocking or destroying nicotinic ACh receptors at the motor end plate.
TTX (Tetrodotoxin): Blocks voltage-gated Na^{+} channels, preventing nerve and muscle action potentials.
BoTox (Botulinum Toxin): Prevents the release of ACh from pre-synaptic terminals, leading to muscle paralysis.
Predictive Ability: Be able to predict the effect of under- or over-activity of any given part of the NMJ based on its normal function.
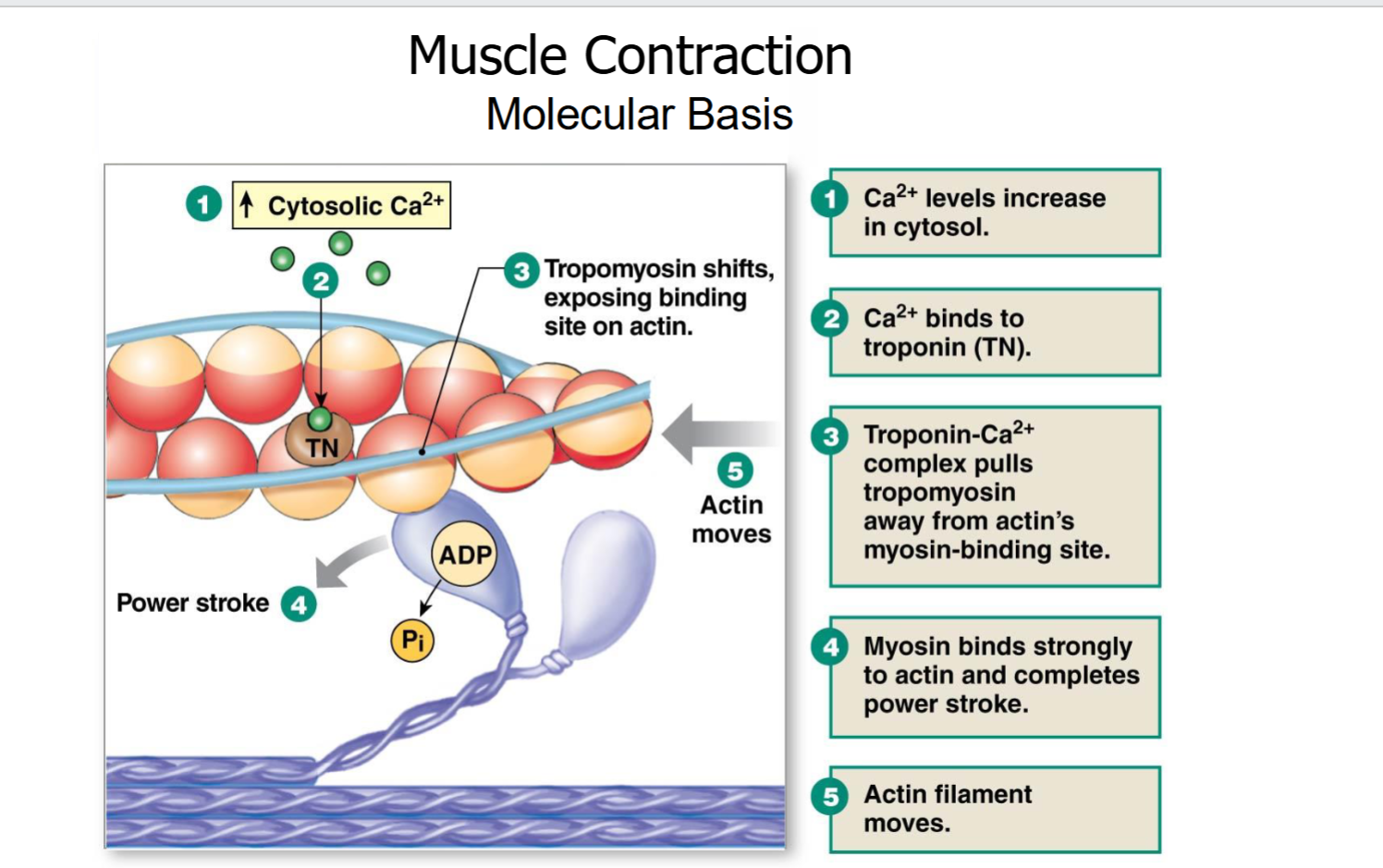
III. Muscle Contraction: Molecular Mechanisms
Myofibrils are made of myofilaments.
Myofibrils: run entire length of muscles. Myofibrils have the ability to shorten, resulting in contraction of the muscle and the production of motion.
Myofibrics are made of many muscle units: sarcomeres.
Sarcomeres: the functional contractile unit in a skeletal muscle fiber: the area between 2 adjacent Z discs/lines (these are at the ed.)
Myofibrils contain multiple and repeating sarcomeres
Each sarcomere shortens as the muscle fiber contracts
-
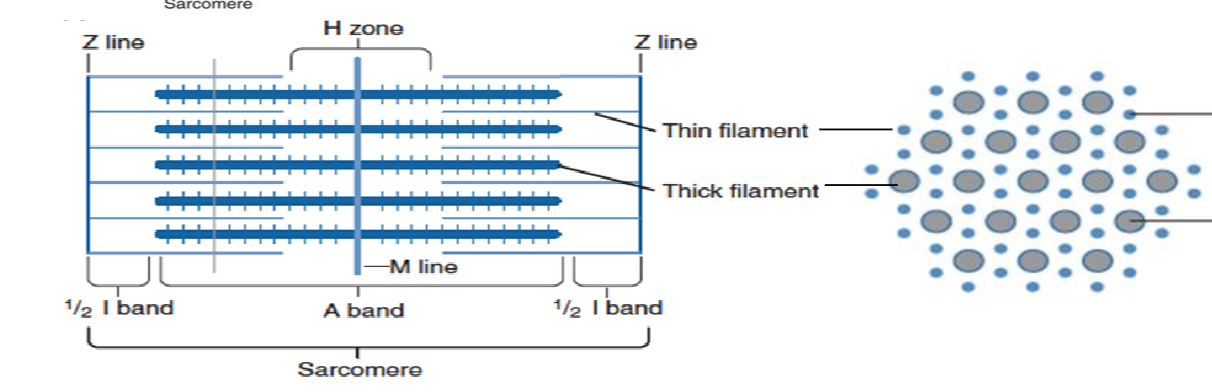
Thin filaments slide across thick filaments towards the center of the sarcomere, resulting in
shortening of the H zone & I Zone. A-Band does not change. The Z-Lines move closer togetherI band: has actin but no myosin overlapping with it.
H zone: myosin without actin.
Cap-Z helps anchor actin protein and anchor it to the Z lines
Titin: anchors myosin thick filaments to the z line, provides
elasticity and
stabilizes myosin.
Nebulin: orients how the actin thin filaments are positioned.
During muscle contraction, the A-band does not change its length
Thin filaments:
5-6 nm in diameter
Double helix of two strands of bead shaped actin molecules twisted around each other
Individual actin molecules: G-actin, globular actin monomers.
Strands of actin molecules: F-actin, fiilamentous actin polymer.
Two primary regulatory proteins are also part of it:
Tropomyosin: cover the myosin-binding sites on actin
Troponin C: it initiates a conformational change that causes tropomyosin to shift, thereby exposing the myosin-binding sites on the actin filaments.
Thick Filaments
Bundles of myosin molecules:
Thick globular heads, long filamentous tails
Myosin heads form cross bridges with actin thin filaments while there’s muscle contraction
11nm
Sliding Filament Theory: Describes the process of muscle contraction by which thin (actin) filaments slide over thick (myosin) filaments, shortening the sarcomere.
A feedback loop.
The response here is: contraction.
Cross Bridge Cycle: Essential for muscle contraction involving several key steps:
Calcium Ion Release & Troponin-Tropomyosin Shift: Increased cytosolic Ca^{2+} ions, released from the SR, bind to troponin C, which then shifts tropomyosin, exposing myosin-binding sites on actin.
Myosin Binding to Actin (Cocked State): A "cocked" myosin head (energized by ATP hydrolysis) binds to the actin active site.
Phosphate Ejection: Inorganic phosphate (P_i) is ejected from the myosin head, strengthening the cross-bridge bond.
Power Stroke: The spring-loaded myosin-head pivots, undergoes a conformational change, pulling the actin filament toward the M-line (center of the sarcomere);
ADP is ejected.
ATP Binding & Myosin Release: A new ATP molecule binds to myosin, causing it to detach from actin (no MLC in skeletal muscle).
ATP Hydrolysis & Resetting: The myosin head's endogenous ATPase activity hydrolyzes ATP to ADP and P_i , re-cocking and spring-loading the myosin heavy chain head, preparing for another cycle.
Importance of ATP: ATP is required for myosin to attach (hydrolysis for cocking) and detach from actin.
Why is Ca2+ important in the contraction?
Binds to troponin, exposes the binding site.
Molecular Basis of Muscle Contraction:
Twitch: a single contraction-relaxation cycle
Motor-axonal AP→ Skeletal muscle fiber AP(longer in duration, lower resting potential -85mV) → contraction (twitch)
Latent period: AP in skeletal muscle but no contraction.
Contraction Phase: can range. Tension rises, we contract our muscle
Relaxation Phase: The muscle fiber relaxes after contraction, leading to a gradual decrease in tension and ultimately returning to its resting state.
To get stronger force → more twitches
Recruit more motor units
Recruit larger motor units
Faster-twitch fibers
Faster frequency of APs
IV. Muscle Comparison: Cardiac Muscle
Cardiac myocytes
Cardiac muscle fibers= heart muscle cells
Found almost exclusively in heart wall
Striated, organized similarly to skeletal muscle with sarcomeres.
One (or 2) nuclei
Y shaped branching
Join other cells at intercalcated discs(= gap junctions + desmosomes)
Ca^{2+} plateaus— prolonged APs
What is NOT different between neuronal and muscle AP?
Peak
WHY is there such a negative skeletal
& cardiac resting potential (Vm)?High permeability to K+
Unlike the skeletal, it is
Shorter fibers and smaller cells
often branched w/ gap junction & desmosomes
Uni or bi nucleate
No direct innervation of most of the muscle cells.
Like the skeletal, it is
striated
sarcomere base unit
Troponin-C Ca^{2+} sensor, with contraction occurring via a mechanism identical to skeletal muscle.
Na+ upstroke
K+ downstroke
~90mV resting potential
Cardiac Action Potentials: Feature a long plateau phase with high levels of Ca^{2+} influx through Voltage-Gated Calcium Channels (VGCCs).
Rapid depolarization due to opening of voltage-gated fast Na^{+} channels.
Plateau (of maintained depolarization) due to opening of voltage-gated slow Ca^{2+} channels (VGCCs) and closing of some K^{+} channels; voltage-gated K^{+} channels it remains open.
Repolarization due to opening of more voltage gated K^{+} channels, and blocking of Ca^{2+} channels.
Depolarization, refractory period, and contraction are all simultaneous in cardiac myocytes.
V. Muscle Contrast: Smooth Muscle
General Characteristics: Non-striated muscle, involuntary control, and mostly found in hollow organs (e.g., intestines, blood vessels).
Filament Organization: Contractile filaments are organized differently than in striated muscle; they are anchored to dense bodies (analogous to Z-discs).
Contraction Mechanism: Unlike skeletal and cardiac muscles, the contraction mechanism utilizes calmodulin (CaM) instead of troponin.
Molecular Components: Roles of:
Calmodulin (CaM): Binds Ca^{2+} ions.
Myosin Light Chain Kinase (MLCK): Activated by Ca^{2+}-CaM complex; phosphorylates myosin light chain (MLC) regulatory protein.
Myosin Light Chain Phosphatase (MLCP): Dephosphorylates MLC, leading to relaxation.
Smooth Muscle Sarcoplasmic Reticulum (SR):
Ca^{2+}-induced Ca^{2+} release at SR RyRs (Ryanodine Receptors).
G-protein coupled receptor (GPCR)-triggered IP3 production leading to IP3-induced Ca^{2+} release at SR IP3Rs. (Note: Ca^{2+} release from smooth muscle SR can be triggered by Ca^{2+}'s opening of RyRs (Ca^{2+} channels) OR G-protein coupled receptor (metabotropic receptors) action, indirectly causing IP3 receptors (which are ALSO Ca^{2+} channels) on SR to open. All GPCRs are considered "metabotropic" receptors).
Control and APs:
Smooth muscle may be controlled by APs, graded potentials, neurotransmitters (NTs), stretch, and hormones.
Smooth muscle can undergo MANY different types of APs and rests less negative (\sim -40 to -50 mV).
Predictive Ability: Be able to predict the effect(s) of altering the activity of various proteins or transporters in smooth muscle.
VI. Muscle Mechanics: Filaments and Fatigue
Muscle Tension: force created by muscle
Load: weight (force or resistance) that opposes contraction
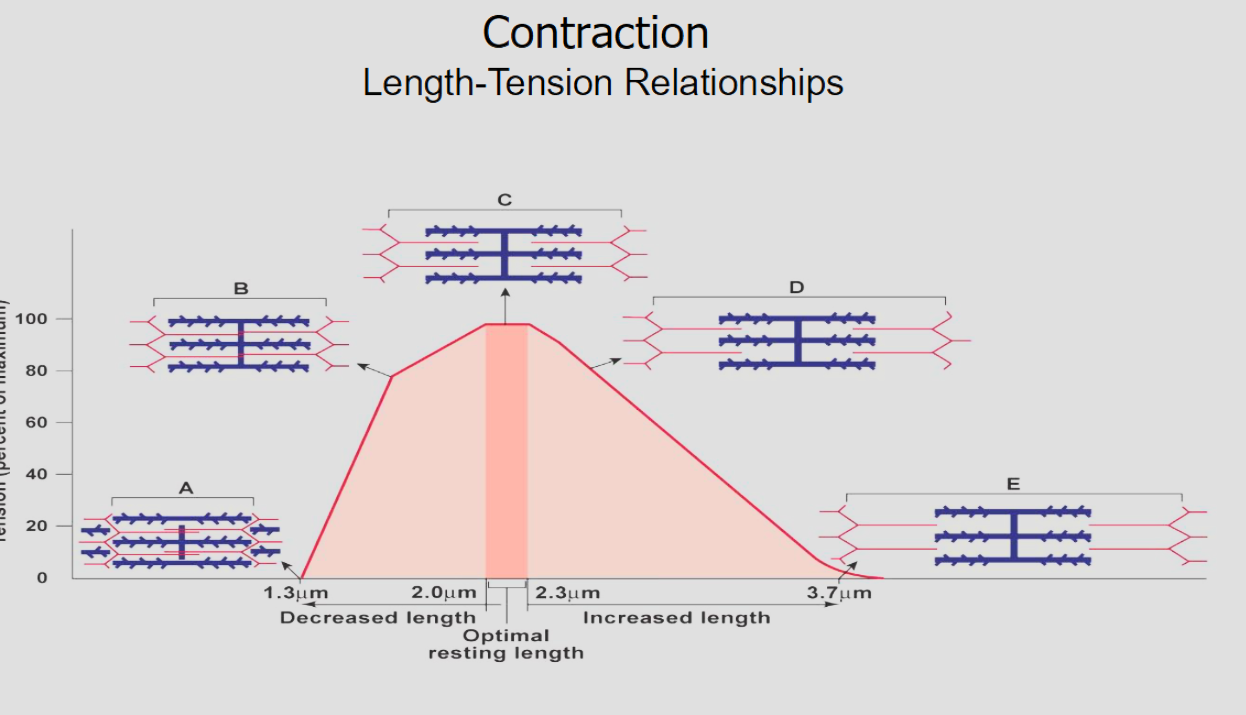
Contraction: creation of tension in a muscle by sarcomere shortening. Length-Tension Relationship: Understand length-tension curves; be able to relate sarcomere length to tension generation (optimal overlap of thick and thin filaments produces maximal tension).
-
Time-Tension Summation & Contraction Types:
Single twitches: muscle relaxes completely between stimuli
Summation: Stimuli closer together do not allow muscle to relax fully
Summation leading to unfused tetanus(repetitive stimuli): stimuli are far apart. they can relax slightly between stimuli
Summation leading to complete tetanus: muscle reaches steady tension. If muscle fatigues, tension decreases rapidly.
Tetanus: sustained muscle contraction from sustained stimulus.
Fatigue: Defined as the decline in the ability of a muscle to generate force.
Muscles fatigue when strong stimulation keeps a muscle in a state of tetanus too long.
Isometric Contraction: Force without moving load
Isotonic Contraction: Create force and move load
Concentric Action: Shortening Action
Eccentric Action: Lengthening Action
Sarcomeres vs Series elastic elements:
Series shorten, elastic elements stretch.
Little change in overall length
Contraction Mechanics at the sarcomere
Muscle at rest
Isometric Contraction: Muscle has not shortened.
Sarcomeres shorten, generating
force, but elastic elements
stretch, allowing muscle length
to remain the same
Isotonic contraction:
Sarcomeres shorten
more but, because elastic
elements are already
stretched, the entire
muscle must shorten
Possible causes of fatigue
Central fatigue: within the CNS. Psychological effects or protective reflexes.
Peripheral fatigue: Anywhere post Somatic motor neuron. Could be due to a change in muscle membrane potential
Modes and Mechanisms of Muscle Fatigue (Depletion/Accumulation Theories):
Depletion Theories: Focus on the exhaustion of energy substrates (e.g., ATP, glycogen) or neurotransmitters (e.g., ACh).
Accumulation Theories: Focus on the buildup of metabolic byproducts (e.g., lactate, inorganic phosphate, H^{+} ions) that interfere with contraction machinery or Ca^{2+} handling.
Fiber-type comparison reveals different characteristics:
Slow-oxidative fibers: Fatigue resistant, high endurance.
Fast-fatigue resistant fibers: Intermediate characteristics.
Fast-fatigable fibers: High power output but fatigue quickly due to limited ATP production.
Skeletal v Cardiac Comparisons
Similar resting potential; in skeletal (-85mV) and cardiac(-90 mv)
The resting potential in skeletal and cardiac is so low because it has higher potassium permeability.
Neuronal and muscle AP have similar peaks.
Cardiac AP upstroke is due to Na+
Muscle Atrophy: a wasting of tissue that
results in reduction of muscle size, tone and power. This can be caused by a lack of stimulation (exercise) to the muscle.
Muscle hypertrophy: an increase in muscle fiber size (not an increase in the number of muscle fibers).
results from repetitive stimulation of muscle fibers.
Mitochondria increase in number therefore the amount of ATP increases.
Both myofibrils and myofilaments increase in number, allresulting in the muscle increasing in size.
Myostatin (growth differentiation factor 😎) is a protein that inhibits muscle growth; therefore, its levels must be carefully regulated to support optimal muscle development.
Clinical Applications
Rigor Mortis: The stiffening of muscles after death due to lack of ATP, preventing myosin from detaching from actin, causing sustained contraction.
-
Muscle Tone: Sustained muscle contraction (low-level) that keeps muscles healthy and maintains posture, and joint stability. Tells muscles that they should be ready in case something happens.
Key Concepts Recap
Muscle fibers consist of myofibrils that contain thick (myosin) and thin (actin) filaments, organized into sarcomeres.
Sliding filament theory explains how muscle contraction occurs via interactions between actin and myosin.
Calcium (Ca^{2+}) and ATP are crucial for muscle contraction, cross-bridge cycling, and muscle relaxation.
Distinction between the types of muscle tissue (skeletal, cardiac, smooth) based on structure, function, and regulatory mechanisms.
-