Musculoskeletal Issues Notes (Week 9)
Skeletal Muscle Structure
Epimysium
Perimysium
Endomysium
Muscle fascicle
Muscle fiber
Sarcolemma
Bone Structure
Articular cartilage
Cancellous bone
Epiphyseal plate
Marrow cavity
Periosteum
Compact bone
Epiphysis, Head, Diaphysis (shaft)
Conceptual Focus
Functional ability
Infection
Mobility
Pain
Perfusion
Safety
Soft Tissue Injury (Table 67.2 – Key Injuries and Management)
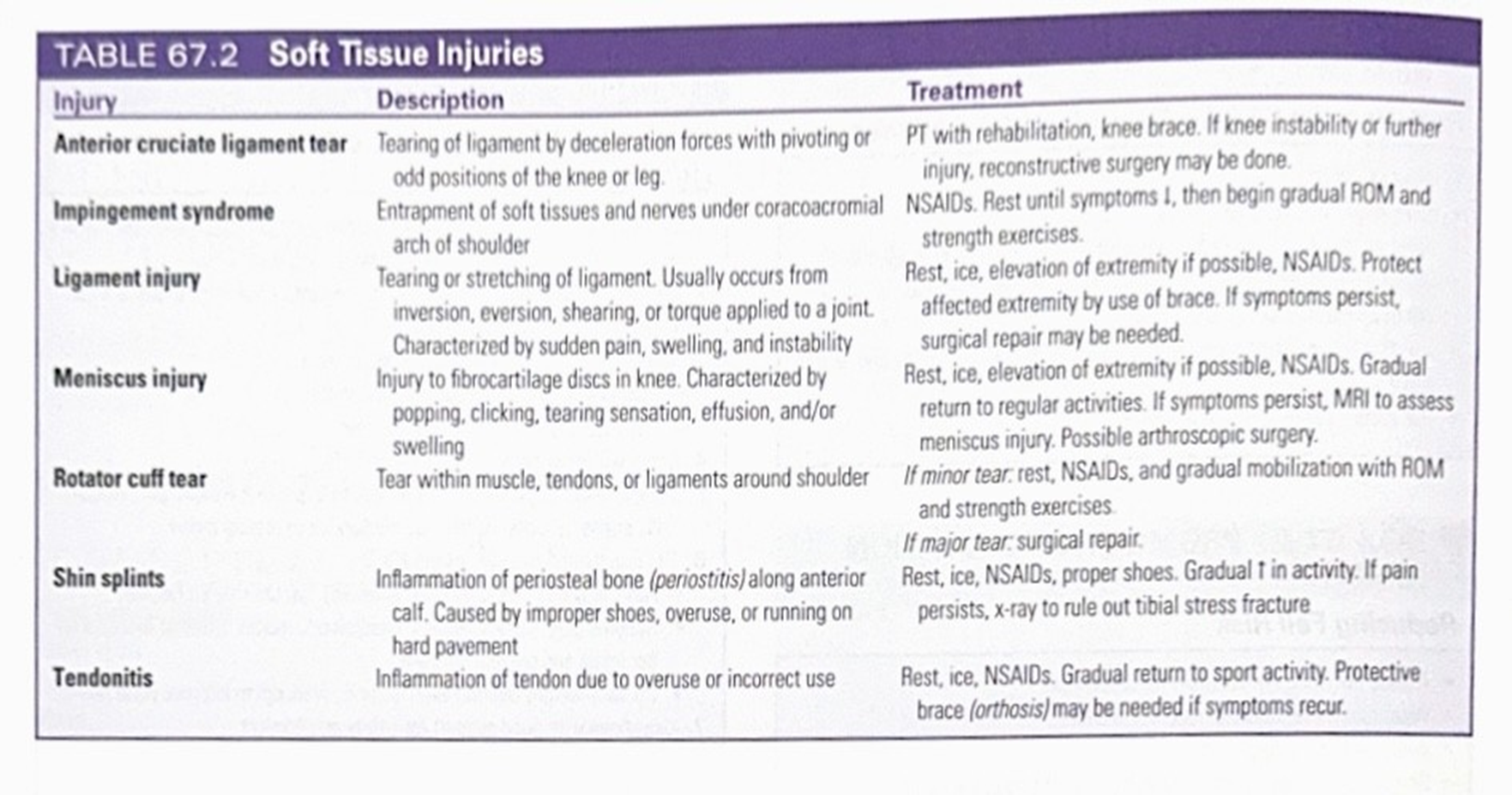
Anterior cruciate ligament (ACL) tear
Cause: deceleration with pivoting
Management: physical therapy with rehab, knee brace; reconstructive surgery if instability persists
Impingement syndrome / rotator cuff issues
Management: rest, NSAIDs, gradual ROM; surgical repair if persistent
Meniscus injury
Management: rest, NSAIDs, gradual ROM; MRI if persistent; possible arthroscopic surgery
Shin splints
Management: rest, ice, elevation, NSAIDs; gradual return to activity; proper footwear
Tendonitis
Management: rest, NSAIDs, gradual strengthening
Periostitis (periosteal inflammation)
Management: rest, ice, NSAIDs; gradual activity; brace if recurrent
Emergency Management (Table 67.3 – Acute Soft Tissue Injury)
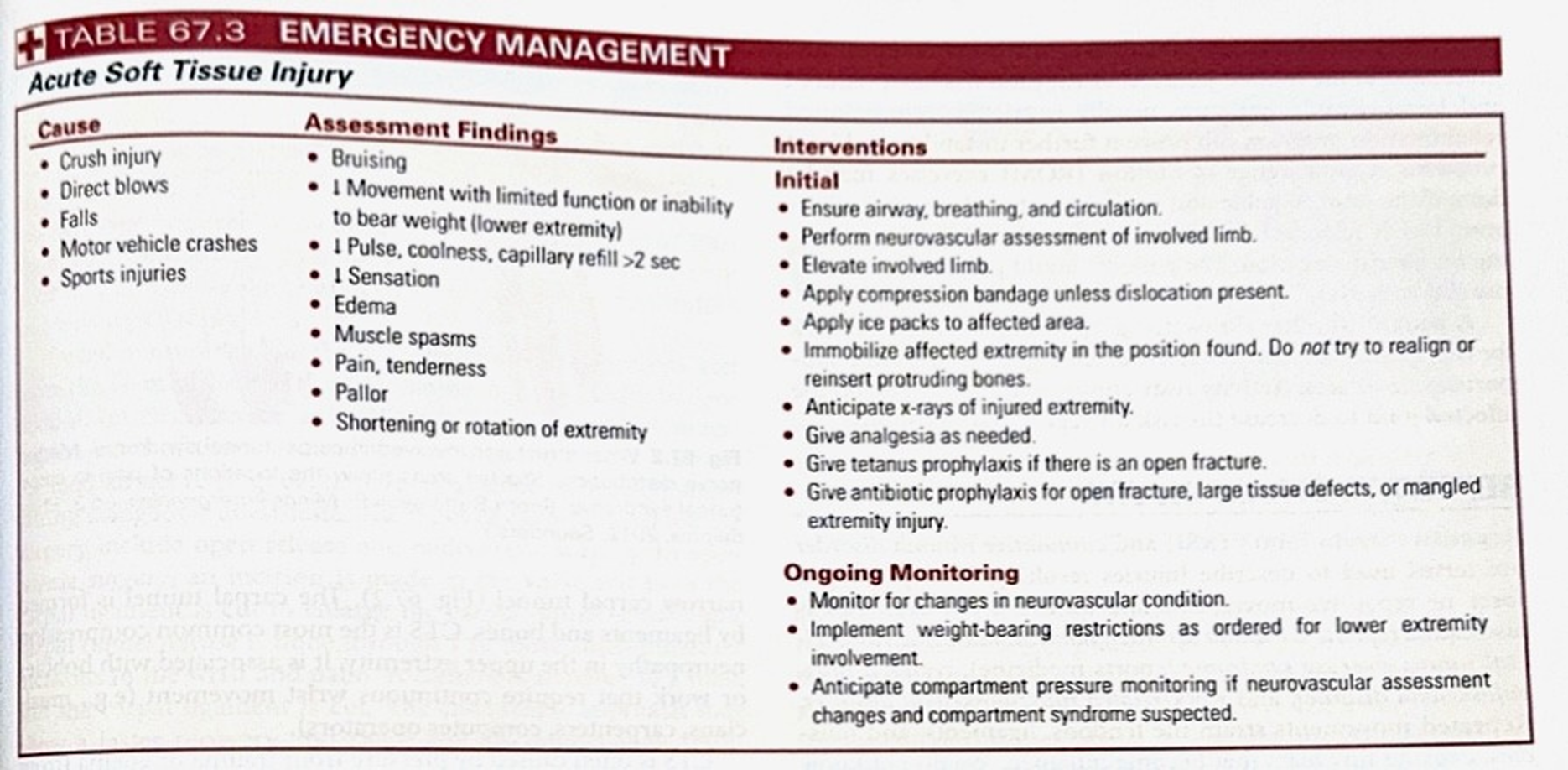
Causes include crush injuries, direct blows, falls, MVCs, sports injuries
Assessment findings: bruising, edema, pain, tenderness, pallor, limited movement, sensory changes
Interventions (Initial):
Ensure airway, breathing, circulation; neurovascular assessment
Elevate involved limb; apply compression if no dislocation; apply ice
Immobilize in position found; do not realign protruding bones
Obtain x-rays; provide analgesia; tetanus prophylaxis for open injuries
Antibiotic prophylaxis for open fractures or mangled injuries
Ongoing Monitoring: monitor neurovascular status; apply weight-bearing restrictions as ordered; monitor for compartment syndrome if concerns arise
Clinical Manifestations of Fractures
Bruising: discoloration distal to injury; usually normal and resolves
Crepitation: grating/crunching; may indicate risk of nonunion if moving ends excessively
Deformity: abnormal position; may impair bony union if not corrected
Edema and swelling: may indicate bleeding; risk of compartment syndrome if unchecked in closed spaces
Loss of function: impaired use of limb
Muscle spasm: protective response; may displace nondisplaced fractures
Pain & tenderness: due to tissue trauma and fragment movement
Diagnostic Tests for Fractures and Soft Tissue Injuries
Laboratory tests: CBC, BMP/CMP, CRP & ESR, PT/PTT, UA
Imaging:
X-ray: plain view, usually 1-view or 2-view; fracture/subtle fractures vs soft tissue injury; 2D picture
CT: detailed bone assessment; 2D/3D views for complex fractures; can show bleed
MRI: soft tissue, ligament, tendon, and occult fractures; show small details
Imaging Views
X-ray
CT
MRI
Types of Fractures
Open vs Closed
Open: skin broken; bone exposure with high infection risk
Closed: skin intact
Displaced vs Non-displaced
Displaced: bone ends off alignment; may be comminuted or oblique
Non-displaced: alignment preserved; often transverse, spiral, or greenstick
Complete vs Incomplete
Complete: break through entire bone
Incomplete: partial crack (e.g., bending/crushing)
Management and Interventions
Fracture Reduction
Closed reduction (manual) or Open reduction (surgical)
Traction as needed (skeletal/traditional)
Fracture Immobilization
Casting or splinting; external fixation; skeletal traction
Open Fractures
Surgical debridement and irrigation; antibiotics; tetanus immunization
Prophylaxis
Antibiotics for open fractures; tetanus/diphtheria vaccination as indicated
Internal/External Fixation
Open reduction internal fixation (ORIF); external fixation if needed
Emergency Management – Fractured Extremity (Table 67.7)
Initial: treat life-threatening injuries first; assess circulation, airway, and breathing
If deformity present: evaluate and monitor distal pulses; avoid realignment of joints; immobilize
Do not straighten fractured/dislocated joints; do not manipulate protruding bone ends
Apply ice; obtain x-rays; tetanus prophylaxis if skin breach
Mark pulses and monitor neurovascular status distal to injury
Ongoing: monitor vital signs, consciousness, oxygen saturation, pain
Monitor for compartment syndrome (pain with passive stretch, pallor, paresthesia, paralysis, pulselessness)
Monitor for fat embolism syndrome (dyspnea, chest pain, fever)
Nursing Management
Cardiovascular: assess distal pulses, skin temperature, cap refill
Neurovascular: assess sensation, paresthesia; monitor changes
Skin: look for lacerations, pallor, edema distal to injury
Functional status: resistance loss, deformity, limited movement
Diagnostics: X-ray, bone scan, CT, or MRI as indicated
Complications to Anticipate and Monitor
Infection: open fractures and soft tissue injuries have higher infection risk
Compartment syndrome: swelling increases pressure; monitor for 6 P's (pain, pressure, paresthesia, pallor, paralysis, pulselessness)
Venous thromboembolism (VTE): high risk with immobilization; initiate prophylaxis
Fat embolism: long bone fractures; monitor for respiratory symptoms; supportive care (O2, possible ECMO/Vasodilators)
Early detection and management are critical to reduce morbidity
Questions
Review key terms, injury mechanisms, and the corresponding urgent management steps for quick recall