Managing Deep Carious Lesions and Maintaining Pulp Vitality in Permanent Teeth
Let’s start with some questions:
• What is the ultimate aim of preserving the pulp?
The ultimate aim of preserving the pulp is to maintain its vitality and functionality. The pulp is essential for:
Biological defence: It contains cells like odontoblasts that form dentin and help defend against infection or trauma.
Sensory function: It detects changes in temperature, pressure, and pain, warning of potential threats.
Nutritional support: It provides nutrients to dentin and keeps it hydrated.
Preserving the pulp ensures the long-term health of the tooth, delaying or avoiding the need for extensive treatments like root canal therapy.
• Preserving pulp vitality……. Can we and how do we?
Yes, preserving pulp vitality is possible, especially with early diagnosis and timely intervention. Key strategies include:
Accurate Diagnosis: Use tests like cold sensitivity, electric pulp tests, and advanced imaging to determine the pulp's condition (vital or non-vital).
Preventative Care: Address caries and trauma early to minimize pulp damage.
Minimally Invasive Techniques: Techniques like indirect pulp capping, stepwise excavation, or selective caries removal help avoid pulp exposure.
Direct Pulp Therapy: If the pulp is exposed but healthy, applying biocompatible materials like calcium hydroxide or MTA (mineral trioxide aggregate) can promote healing and bridge formation.
Control of Inflammation: Use anti-inflammatory agents or medicaments, like corticosteroids, when indicated.
• Can we create an environment which enables pulp recovery?
Yes, creating a conducive environment for pulp recovery involves the following:
Sterility: Use of a rubber dam during procedures to prevent contamination.
Biocompatible Materials: Materials like MTA, Biodentine, or calcium silicate types of cement can stimulate reparative dentin and seal against bacterial ingress.
Antimicrobial Strategies: Removal of bacteria through proper caries excavation, disinfection, and the use of medicaments like chlorhexidine.
Control of External Factors: Reducing occlusal trauma or excessive temperature changes to minimize stress on the pulp.
Improved Blood Supply: Promoting blood flow to the pulp through minimally invasive procedures, as the pulp’s healing depends on its vascular supply.
What is deep caries? Can you define it?
Deep caries = Reaches inner 1/3 (ICCC)1 or inner ¼ (ESE)2 of dentine but with a zone of hard or firm dentine between the caries and the pulp
Extremely deep caries = Caries penetrating the entire thickness of dentine (ESE)
Why does it matter?
Before going to the next slide, stop and think, why does it matter that we define how deep carious lesions are?
• write down three reasons why it matters…. And reflect on those three reasons.
Guides Treatment Strategy:
The depth of the lesion determines whether non-invasive measures (e.g., fluoride application, remineralization) or invasive measures (e.g., selective caries removal, pulp therapy) are needed.
Shallow lesions may only require remineralization, while deep lesions necessitate careful excavation to avoid pulp exposure.
Predicts Pulp Health:
The closer the lesion is to the pulp, the higher the risk of pulpitis or irreversible damage.
Defining depth helps anticipate the likelihood of pulp vitality preservation or the need for endodontic intervention.
Prevents Overtreatment or Undertreatment:
Misjudging depth can lead to overtreatment (e.g., unnecessary removal of healthy dentin) or undertreatment (e.g., leaving caries untreated, risking progression).
Accurate assessment ensures balance, preserving as much healthy tissue as possible while addressing pathology.
Reflection on These Reasons:
Source of Reasoning:
These reasons are drawn from a combination of taught theory and clinical reasoning.
The focus on treatment strategy and pulp health stems from lecture-based knowledge, where the biology of caries and pulp-dentin interaction was emphasized.
The importance of avoiding overtreatment comes from clinical experience, where misjudgments can have long-term consequences for the patient.
Why They Matter:
Clinically, mismanagement can lead to patient pain, loss of tooth vitality, or the need for more invasive procedures.
Theoretically, understanding lesion depth reflects a fundamental principle: balancing disease control with tissue preservation.
• Did you choose the reasons because of clinical experience or did you draw upon taught theory from lectures you have attended?
Lectures
Thinking points before we proceed.
• Dental caries in the enamel can prompt a pulpal response.
• Evidence suggests significant bacterial contamination and areas of pulp necrosis in extremely deep caries ( See citation below).
As clinicians we need to understand the status of the pulp….it is vital we have this understanding, so the appropriate care can be offered and referral made if required
Pre-operative assessment is key…..
• Dental professionals, will see patients through various care pathways,
• Direct access to dental therapist or dentist
• Referral from a dentist/DWSi/specialist/consultant
• Regardless of how the patient has arrived to you, it is still your responsibility to pre-assess the patient.
Revision: it may be worth reviewing the scope of practice of a dental therapist and dentist.
• obtain a detailed dental history from patients and evaluate their medical history
• carry out a clinical examination within their competence
• complete periodontal examination and charting and use indices to screen and monitor periodontal disease
• diagnose and treatment plan within their competence
• prescribe radiographs
• take, process and interpret various film views used in general dental practice
• plan the delivery of care for patients
• give appropriate patient advice
• provide preventive oral care to patients and liaise with dentists over the treatment of caries, periodontal disease and tooth wear
• undertake supragingival and subgingival scaling and root surface debridement using manual and powered instruments
• use appropriate anti-microbial therapy to manage plaque-related diseases
• adjust restored surfaces in relation to periodontal treatment
• apply topical treatments and fissure sealants
• give patients advice on how to stop smoking
• take intra and extra-oral photographs
• give infiltration and inferior dental block analgesia
• place temporary dressings and re-cement crowns with temporary cement
• place rubber dam
• take impressions
• care of implants and treatment of peri-implant tissues
• Carry out direct restorations on primary and secondary teeth
• Carry out pulpotomies on primary teeth
• extract primary teeth
• place pre-formed crowns on primary teeth
• identify anatomical features, recognise abnormalities and interpret common pathology
• Carry out oral cancer screening
• if necessary, refer patients to other healthcare professionals
• keep full, accurate and contemporaneous patient records
• if working on a prescription, vary the detail but not the direction of the prescription according to patient needs. For example the number of surfaces to be restored or the material to be used.
Dentists:
• diagnose disease
• prepare comprehensive treatment plans
• prescribe and provide endodontic treatment on adult teeth
• prescribe and provide fixed orthodontic treatment
• prescribe and provide fixed and removable prostheses
• carry out oral surgery
• carry out periodontal surgery
• extract permanent teeth
• prescribe and provide crowns and bridges
• provide conscious sedation
• carry out treatment on patients who are under general anaesthesia
• prescribe medicines as part of dental treatment
• prescribe and interpret radiographs
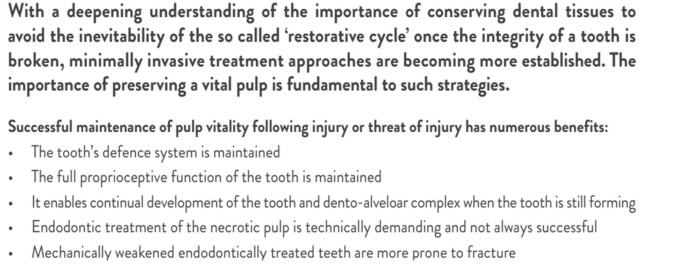
Are selective caries removal techniques appropriate?
Deep Caries in Vital Teeth: To prevent pulp exposure while halting disease progression.
Minimally Invasive Dentistry Philosophy: Emphasizes preserving healthy tooth structure and pulp vitality.
Patients with Good Oral Hygiene: Where long-term restoration success is more likely.
What are the principles of all ‘vital pulp therapies’? stop and think.
Accurate Diagnosis: Confirm that the pulp is vital and either healthy or has reversible pulpitis.
Minimally Invasive Techniques: Limit intervention to what is necessary for preserving pulp health.
Aseptic Conditions: Use of rubber dam and sterile techniques to avoid bacterial contamination.
Biocompatible Materials: Utilize materials like calcium hydroxide, MTA, or Biodentine to promote healing and dentin bridge formation.
Control of Inflammation: Remove infected tissue and create an environment conducive to pulp recovery.
Effective Sealing: Ensure that the final restoration prevents reinfection.
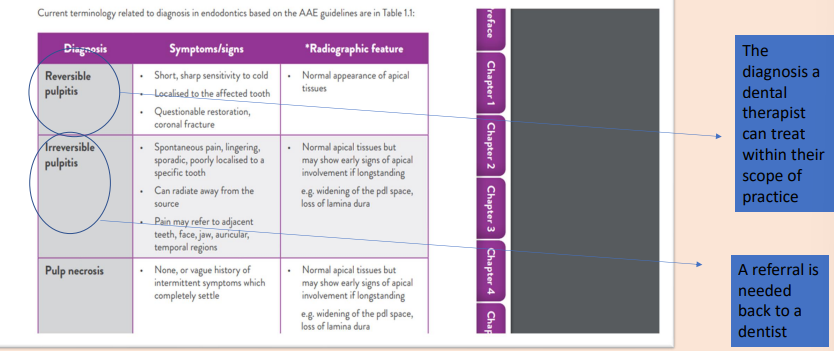
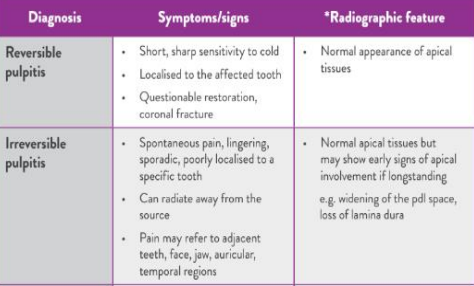
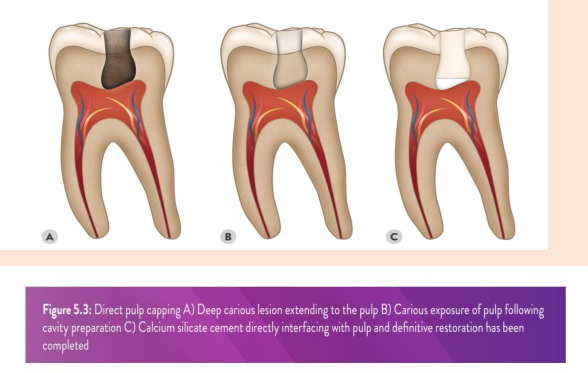
Revision: Signs and Symptoms
Comprehensive history…… a conversation with a patient… should not be an interview with a checklist…..
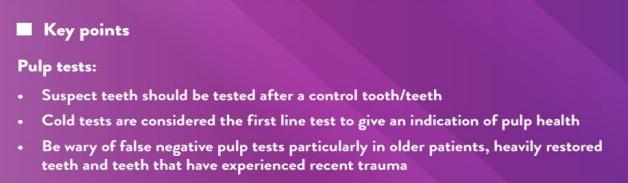
Sensibility testing
TTP
Pressure
Mobility
Sinus
Electric pulp test
Cold
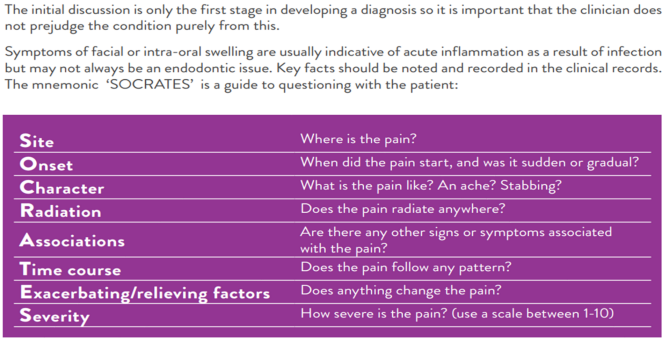
History taking….
Making a diagnosis is a process that begins with collecting accurate information from the patient verbally, conducting a clinical examination, carrying out special tests and assimilating the facts to determine the disease or the problem that the patient has.
Key points.
History and examination:
• Give time to your patients and listen to them carefully
• Gather information in a methodical and systematic fashion
• Optimise the clinical examination by using good light, magnification and ensuring nothing obscures vision
Pain history and conversation with patients
What can we do in primary dental care settings ….
Look with a mirror
Radiographs
Pulp Test
Endofrost
Pulpal diagnosis.
• The key is to recognise the pulpal diagnosis as a continuum (that can also change with time)
After assimilation of the symptoms, clinical examination and results of the special tests, a diagnosis or provisional diagnosis can be made.
Carious Tissue removal revision.
• Carious Tissue removal:
• Selective carious tissue removal in one-stage
To ‘soft’ dentine (can be removed with hand instruments)
To ‘firm’ dentine (resists hand instruments)
To ‘hard’ dentine (sound dentine, resists probe penetration and scratching
What next?
• Imagine you have been referred an upper left second permanent molar to restore, you have concluded that you are able to restore the tooth and maintain pulp vitality by using selective caries management, removing carious tissue to soft dentine. You have a bitewing radiograph, quality rating A.
• The carious lesion is deep and reaches the inner 1/3 of dentine, the lesion is positioned mesio-occlusally. You have an updated treatment plan and PSD for the LA.
• The patient is fit and well (ASA1). You proceed with treating the UL7, under dental dam, the carious lesion is more extensive than you thought, and you have a carious exposure.
Food for thought…
We need to start to think about diagnosis again……
Strategies for vital pulp treatment (VPT)
• 1. Indirect pulp capping: The application of a material onto a thin layer of dentine which is close to the pulp with the aim of producing a positive biological response so the pulp can protect itself.
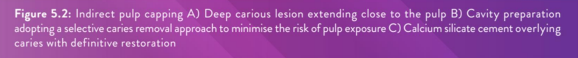
• 2. Direct pulp capping: The application of a material directly onto the pulp with the aim of producing a positive biological response so the pulp can protect itself.
• 3. Partial pulpotomy: The removal of a small portion of superficial coronal pulp tissue followed by the application of material directly onto the pulp with the aim of producing a positive biological response so the pulp can protect itself.
• 4. Full pulpotomy: Complete removal of the coronal pulp to the root canal orifice level followed by the application of material directly onto the remaining pulp with the aim of producing a positive biological response so the pulp can protect itself.
Strategies for vital pulp treatment (VPT) for the dental therapist/dentist
• 1. Indirect pulp capping: The application of a material onto a thin layer of dentine which is close to the pulp with the aim of producing a positive biological response so the pulp can protect itself.
• 2. Direct pulp capping: The application of a material directly onto the pulp with the aim of producing a positive biological response so the pulp can protect itself.
Dental therapists, ideally should not be referred extremely deep carious lesions, caries penetrating the entire thickness of dentine. Number two should only be undertaken if a carious breach of the pulp has occurred during the caries removal process, you should not be referred a direct pulp capping treatment on a permanent tooth as a dental therapist, however, you should be able to manage this scenario if it occurs e.g., during treatment of a direct access patient.
• 3. Partial pulpotomy: The removal of a small portion of superficial coronal pulp tissue followed by the application of material directly onto the pulp with the aim of producing a positive biological response so the pulp can protect itself.
• 4. Full pulpotomy: Complete removal of the coronal pulp to the root canal orifice level followed by the application of material directly onto the remaining pulp with the aim of producing a positive biological response so the pulp can protect itself.
The above points are outside of the scope of practice of a dental therapist. You will need to refer the patient back to the dentist for points, four and five.
Teamwork and thinking of the patient’s best interest is key whether you are a dentist or dental therapist.
How is the skill mix most suitably used to gain the optimal result for the patient?
Delegation of Roles:
Dentists focus on diagnosis, complex restorative procedures, and treatments requiring higher levels of expertise (e.g., crown preparation, surgical extractions).
Dental therapists handle preventive and routine restorative care, freeing up the dentist to manage more complex cases.
Hygienists focus on periodontal care and oral health education, improving overall patient outcomes through prevention.
Example: While the dentist performs a root canal, the dental therapist can manage a child patient’s fissure sealants or basic restorative treatments.
Patient-Centered Approach:
Skill mix ensures that patients see the right professional for their specific needs, reducing waiting times and enhancing satisfaction.
Therapists and hygienists can build rapport with patients during routine visits, encouraging compliance with preventive measures.
Efficiency and Cost-Effectiveness:
Delegation minimizes duplication of tasks and maximizes productivity within the practice.
It can reduce treatment costs for the patient, as therapists or hygienists can handle less invasive procedures.
Enhanced Continuity of Care:
Therapists and hygienists often provide ongoing maintenance, spotting early signs of issues that require a dentist’s intervention.
Communication within the team ensures seamless transitions between providers, benefiting the patient’s overall experience.
Focus on Prevention:
Therapists and hygienists play a pivotal role in preventive care through oral health education, dietary advice, and fluoride treatments, reducing long-term oral health issues.
This preventive approach aligns with minimally invasive dentistry, which prioritizes preserving natural tooth structure.
Indirect pulp cap
• Indications: dentine is lost due to caries, trauma or a previous iatrogenic intervention and a cavity exists which is close to the pulp but dentine still remains over the pulp tissue.
• The tooth should be isolated with a rubber dam and the cavity preparation completed as appropriate, with attention to peripheral caries removal before carefully approaching the floor and axial wall where a pulpal exposure might be anticipated. It is worth noting, that when dealing with proximal cavities, the pulp horn breach is more likely on the wall and less likely on the floor of the cavity.
• The cavity should be disinfected using cotton pellets soaked (removing gross excess) ideally with sodium hypochlorite (0.5-5%) for 30 seconds to one minute.
• Having dried this, the deepest part of the cavity closest to the pulp should ideally be covered with a CSC e.g., Bio Dentine but setting calcium hydroxide is suitable if an appropriate CSC is not available.
• If calcium hydroxide is used it should be sealed with glass ionomer cement (GIC) or a resin glass ionomer cement (RMGIC). The tooth is then definitively restored and kept under review.
Indirect pulp cap, stages as outlined below:
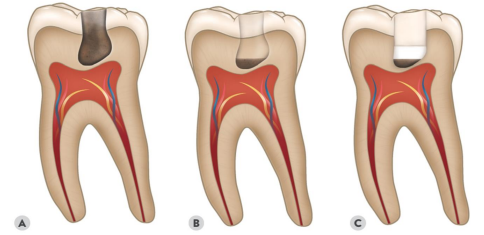
It is worth noting, that in picture B, the brown area could be either soft carious tissue or hard.
Direct pulp capping
• Indications: dentine is lost due to caries, trauma or a previous iatrogenic intervention and a cavity exists. However, in this case, the soft tissue of the pulp is exposed and in most cases is bleeding. If symptoms exist they should be relatively mild and not considered to be indicative of irreversible pulpitis.
• The tooth should be isolated immediately with a rubber dam. It should be disinfected using cotton pellets soaked (removing gross excess) ideally with sodium hypochlorite (0.5 -5%) until bleeding is controlled.
• If bleeding is not controlled within five minutes a partial pulpotomy should be carried out. This is outside the scope of practice of a dental therapist, the dental therapist should, therefore, dress the tooth and make the referral to a dentist/specialist for review.
• The exposed pulp should be covered preferably with a CSC but setting calcium hydroxide is suitable if an appropriate CSC e.g. Bio Dentine is not available. If calcium hydroxide is used it should be sealed with glass ionomer cement (GIC) or a resin glass ionomer cement (RMGIC).
• The tooth can be definitively restored and kept under review. The patient should be warned of the possibility of further treatment should symptoms occur.
Direct pulp capping pulp capping stages
Direct Pulp Capping Key Points
VPTs should monitored carefully by history and clinical examination at 6 months with a PA at 1 year.
VPTs carry a high success rate
Are there any more questions we need to ask ourselves?
• Are you working within your scope of practice i.e. is the referral appropriate if an extremely deep radiographic carious lesion is present?
• What is the radiographic assessment that is needed and why?
• Can you assess the degree of pulp horn recession/tertiary dentine formation?
• If you are referred to a patient who presents with extremely deep radiographic carious lesions, what will you do?
Understand when to stop and ask yourself if are you trained and competent to do the treatment within your scope of practice. We will discuss this further in your clinical skills session. Start to think about the above, and write down your answers and thoughts, so we can draw upon these in the taught sessions.
What about treatment alternatives for the dental therapists and dentists?
Stepwise carious lesion management is extremely beneficial for therapists working under direct access.
• What is the step wise technique?
Procedure Overview:
First Visit:
Partial Caries Removal: Excavate carious dentin, leaving a thin layer of softened dentin over the pulp to avoid exposure.
Temporary Restoration: Seal the cavity with a suitable temporary material to create a bacteria-tight environment, promoting remineralization and reducing bacterial load.
Second Visit (After 2–24 Months):
Re-entry and Assessment: Reopen the cavity to evaluate the condition of the dentin.
Complete Caries Removal: Remove any remaining carious dentin, which may have hardened due to remineralization.
Definitive Restoration: Place a permanent restoration to ensure a durable seal and restore tooth function.
Advantages:
Reduced Risk of Pulp Exposure: By initially leaving a layer of carious dentin, the technique minimizes the chance of exposing the pulp, which can lead to complications.
Pulp Healing Promotion: Sealing the cavity temporarily allows the pulp to initiate reparative processes, potentially leading to the formation of tertiary dentin.
Bacterial Load Reduction: The temporary seal decreases bacterial activity, limiting further caries progression.
Considerations:
Patient Compliance: Success depends on the patient returning for the second visit; failure to do so may compromise treatment outcomes.
Material Selection: Choosing appropriate temporary and permanent restorative materials is crucial for effective sealing and durability.
Clinical Judgment: Dentists must assess each case individually, considering factors like lesion depth, tooth vitality, and patient-specific circumstances.
Stepwise removal (Summary)
• Stepwise removal is carious tissue removal in 2 stages, i.e., visits
• Soft carious tissue is left over the pulp in the first step, A provisional restoration is placed e.g. GIC. while peripheral dentine is prepared to hard dentine to allow a complete and durable seal of the lesion.
The reasoning for stepwise removal is the expectation that in the first step, tertiary dentine is formed, demineralized dentin becomes remineralised, and the amount of viable bacteria is reduced.
The restoration is removed, possibly 6-12 months later, this is patient-dependent. An opportunity to re-evaluate changes in intralesion colour and hardness can now occur. Why is this important?
1. Assessment of Caries Arrest and Progression
Colour Changes:
Darker or brownish discolouration in the lesion often indicates remineralization or caries arrest.
Yellowish or lighter areas may suggest persistent or active caries.
Hardness:
Hardened dentin signals remineralization, indicating that the pulp's reparative process is occurring.
Soft or tacky dentin may suggest remaining bacterial activity, requiring further excavation.
2. Risk Evaluation for Pulp Exposure
If the lesion shows hardening and remineralization, less dentin needs removal during re-entry, reducing the risk of pulp exposure.
Conversely, soft dentin might necessitate careful excavation to eliminate active infection, balancing the need to protect the pulp.
3. Optimizing Restorative Outcomes
Seal Longevity:
Harder intralesional dentin provides a more stable base for the definitive restoration, enhancing its longevity.
Informed Material Choice:
Observations about lesion hardness and remineralization inform the choice of restorative material, ensuring the best outcomes for sealing and durability.
4. Monitoring Pulp Vitality
Re-assessment provides insight into the pulp's healing process. Signs of successful tertiary dentin formation suggest pulp vitality has been preserved.
If symptoms of irreversible pulpitis or necrosis arise, alternative treatments like root canal therapy can be considered.
• Stepwise carious lesion management is extremely beneficial for therapists working under direct access. It is less cost-effective, but it could avoid pulpal exposure that would potentially necessitate onward referral to a dentist or specialist.
Summary points for the dental therapist.
• Take a careful history and listen to the patient.
• Ensure you have a clear pulpal diagnosis before starting.
• Work within your scope of practice i.e. refer appropriately if an extremely deep radiographic carious lesion is present
• Understand when to stop and reassess the tooth, are you trained and competent to do the treatment within your scope of practice?
• Understand the reasons for referral and referral pathways.